Principles of infant nutrition
Breastfeeding
Learning outcomes
Having read this chapter, the reader should be able to:
There can be no doubt as to the suitability of human milk for human infants. It is an internationally recognized fact that babies should be breastfed exclusively for the first 6 months of life, and then preferably (with a weaning diet) until 2 years old and onwards (WHO 2011). However, while the UK 2010 Infant Feeding Survey (HASCIC 2012) noted an increase (since the 2005 survey) in the number of babies being breastfed at 6 weeks of age, the figure still remains low at 34%. Colson (2005a) questions the advice and care given to breastfeeding women over the last few decades and suggests that the relationship of particular maternal/child positions stimulate innate breastfeeding behaviours and so significantly aid the initiation of breastfeeding (Colson 2007a). Colson (2007a) terms this new approach to breastfeeding initiation as biological nurturing (BN). This will be reviewed in this chapter as well as the traditional approach to breastfeeding practice. Also discussed are basic breast anatomy, feeding cues and patterns, assessing for effective feeding and problem solving. The chapter ends by discussing the safe expressing and storage of breast milk.
Understanding lactation
Each breast functions independently. Each has a rich blood, nerve and lymphatic supply and is comprised of glandular tissue and fat. Support is provided from ligaments. The proportions of fat and glandular tissue vary for each woman, glandular tissue increases in pregnancy under hormonal influences in preparation for lactation. In some women the proportion of glandular tissue to fat is 2 : 1.
The glandular tissue is an extensive convoluted ductal network separated into lobes. These are subdivided into lobules; within each lobule are alveoli, each of which is a cavity lined with lactocytes surrounded by myoepithelial cells. Under the influence of prolactin, milk is produced in the lactocytes. When the infant suckles (under the influence of oxytocin) the milk is propelled into the network of ducts by the muscular contraction of the myoepithelial cells. The lactiferous ducts branch to join other larger ducts, eventually opening out onto the surface of the nipple. Geddes (2009) suggests that there are 4–18 ducts opening onto the nipple, the average being 9. The network of ducts has been identified much nearer to the surface of the breast than originally thought and the milk collecting areas (lactiferous sinuses) were not visualized, suggesting that milk is transported freshly through the ducts on demand, rather than being stored.
Colostrum is present from about the 16th week of pregnancy but it is the loss of placental hormones, particularly progesterone, that initiates the rise in oxytocin and prolactin and therefore the availability of increasing volumes of milk for the newborn infant. Colson (2008, 2007b) suggests that practice should protect and encourage the mechanisms that stimulate breastfeeding hormones in order to ensure effective transfer of nutrition from mother to child. These include prolonged cuddling and baby holding, skin-to-skin contact, privacy, feeding in biological nurturing positions (below), and maintaining the physical environment in a calm, warm, safe manner (minimal neocortical stimulation). Early priming of the lactocytes is essential for the long-term production of breast milk. This occurs with an early first feed after delivery, under the influence of rising prolactin levels.
Milk is supplied according to demand; consequently it is the effective removal of milk from the breast, according to the baby’s appetite and feeding action, that stimulates the milk supply. Milk composition changes during the feed (and changes over time as the infant grows) so that both the hunger and thirst are satisfied. Consequently, babies require nothing other than breast milk for the first 6 months of life. As the baby comes off the breast, the second one is always offered, the baby will only take from the second one if he is still hungry or thirsty.
Successful attachment at the breast using a traditional approach
There is no doubt in any part of the literature that an incorrect attachment at the breast potentially damages the nipples and prevents effective transfer of milk.
These are the principles for achieving successful attachment at the breast:
• Encourage the mother to be comfortable.
• Ensure that the baby’s body is turned in, close to the mother’s body.
• Keep the baby’s head and body in a line.
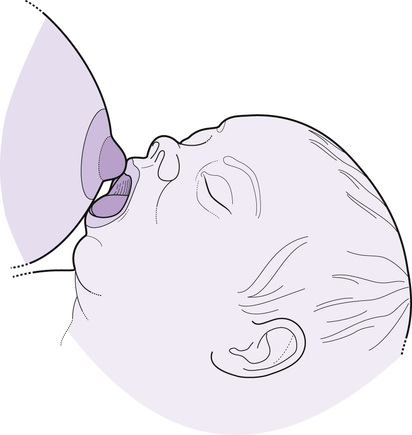
• With a wide mouth, the baby is brought swiftly to the breast, chin leading, aiming the nipple to the back of the baby’s mouth (Fig. 41.1).
Inch (2013) states that breastfeeding is a learnt skill. This means that the midwife’s role is both in educating parents (generally using a ‘hands off’ approach) and in enabling the mother to gain the skills and confidence for herself. Appreciating that the baby is appropriately positioned and attached at the breast allows for feeding to be relaxed and effective. These are some of the signs that the mother can look for:
• The baby has a large mouthful of breast tissue, with his lips curled out.
• The baby’s cheeks should be rounded and stay rounded as he feeds.
• Feeding is quiet, no sucks or clicks are heard, but audible swallowing may be heard.
• The parents should see adequate urine and stool output (see below).
• From about 2 weeks of age, regular weight gain is seen.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree