Principles of drug administration
Injection technique
Learning outcomes
Having read this chapter, the reader should be able to:
Preparations are administered via an injection if they cannot be absorbed, or are absorbed too slowly, when given via other routes. In this chapter the safe administration of drugs via intramuscular (I.M.), subcutaneous (S.C.) and intradermal (I.D.) injection will be reviewed. Intravenous injection is reviewed in Chapter 23. Suitable injection sites in the adult and baby are highlighted and there is discussion about appropriate equipment to use. It is important that this chapter is read in conjunction with Chapter 18.
Indications
The midwife administers drugs by injection on a number of occasions; the following is an indicative, but not exhaustive list:
• uterotonic agent, e.g. active third stage of labour, postpartum haemorrhage
• analgesia or antidote, e.g. pethidine, morphine
• subcutaneous heparin (thromboembolic prophylaxis)
• steroids (fetal lung maturity prior to preterm birth)
As for all medications, the midwife should be competent to identify and manage any unforeseen emergencies, e.g. anaphylaxis or cardiac arrest. Medication given via an injectable route cannot be withdrawn.
Many people are uncomfortable with the idea of having an injection. The midwife has a responsibility to ensure that the woman is ‘put at ease’ and is aware of what is being administered, why and how. She also needs to be assured that the equipment chosen and technique used will promote both safety and comfort. For the client with significant needle phobia, alternative strategies may be needed and assistance from a colleague should be sought.
Safety considerations
Giving an injection exposes midwives to potential needlestick injury. Used needles must never be resheathed and sharps must be disposed of immediately into a sharps box at the point of care. However, in many situations a needle safety device is already fitted; these should be used on every occasion. Needle safety devices are all different in appearance but in principle work so that as soon as the needle is withdrawn from the tissue it is covered and protected. It can appear as a type of trough for the needle to sit into. Often the practitioner initiates the shield by flicking it over using the same hand as injecting with. Filter/filtered needles are used to draw solutions up into the syringe, these prevent shards of glass or shavings of rubber from entering the syringe.
Hands should be decontaminated; the World Health Organization (WHO 2010) suggest that gloves are not necessary. Skin cleansing remains an unresolved issue, Public Health England (Public Health England (PHE) 2013) suggest that none is necessary for immunizations while Ansell & Dougherty (2011) advocate its use as per the Aseptic Non Touch Technique (ANTT) (Rowley & Clare 2011) approach (see p. 89). This involves at least 30 seconds of up and down, right to left skin cleansing that creates friction, using a locally agreed alcohol-based product, then the skin dries for at least 30 seconds. ANTT themselves are in the process of producing guidelines for skin preparation prior to injection (personal communication), the reader is encouraged to be alert to this and in the meantime to practice according to locally agreed protocols. Visibly unclean skin is always cleansed prior to injection. Whether the skin is cleansed or not, the injection should be prepared and administered using ANTT.
Intramuscular injection (I.M.)
Choice of site in the adult
As suggested, intramuscular (I.M.) is injection into muscle. It can be painful and absorption can be unreliable (Jordan 2010) but the response is often seen quickly, e.g. the use of oxytocin in the third stage of labour. The choice of site is important. It may depend upon:
• the number of millilitres to be injected (although this is questionable)
• the speed of administration. Malkin (2008) suggests that it should be 10 seconds/mL
• the mobility of the woman and accessibility of the site
• the anatomical relation of other structures (nerves, bones, blood vessels)
Recommended sites (adults)
There are five recommended sites for I.M. injection (Workman 1999). However, despite Rodger & King’s recommendations (based on a literature search of all available evidence) in 2000 to use the ventrogluteal site for preference (Hall 2015 agrees), it is still rarely seen in UK practice. It remains the preferred/recommended site of choice. The chosen site is often the gluteus maximus but this is the only site that has close proximity to significant vessels and nerves and so should be avoided (Malkin 2008). These are the five sites:
• Deltoid muscle of upper arm (maximum 1 mL) (Fig. 20.1A): the site is approximately 2.5 cm below the acromial process on the lateral surface of the arm, extending to the level of the axilla (an inverted triangle in shape). Often the choice of site for vaccinations, often easily accessible.
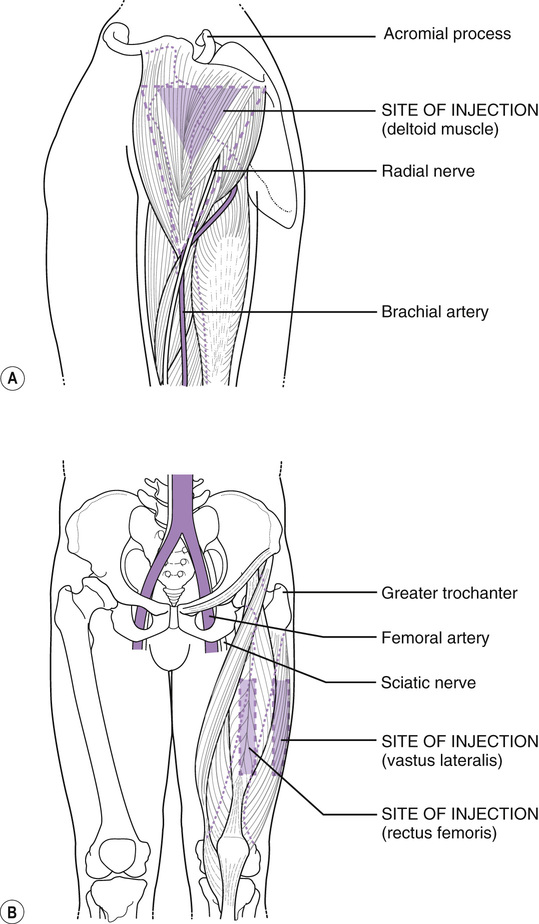
• Quadriceps muscle (vastus lateralis, maximum 5 mL): this is found on the thigh by measuring a hand’s breadth down from the greater trochanter, and one up from the knee, this middle third of the lateral aspect of the thigh is the correct muscle (Fig. 20.1B). The rectus femoris is adjacent on the anterior aspect of the thigh; it is used less and is not appropriate in children (Fig. 20.1B).
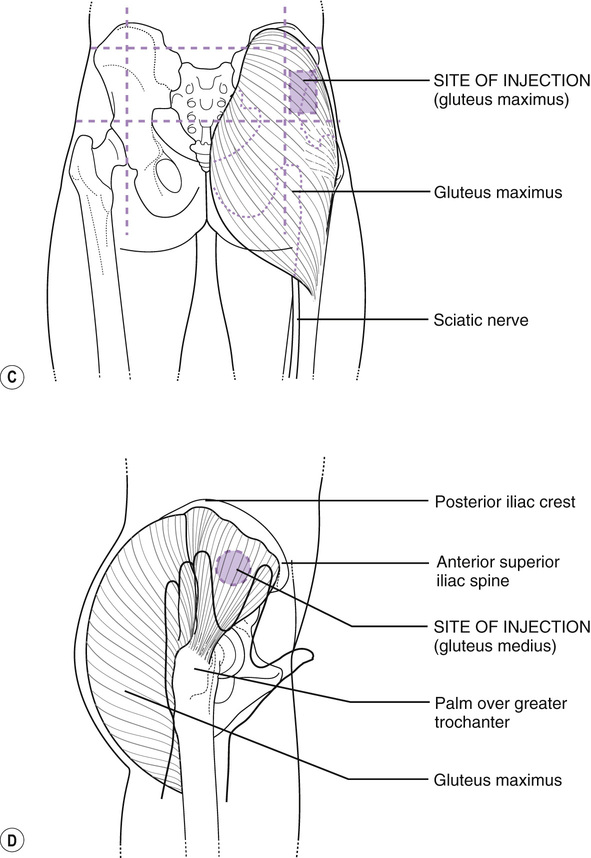
• Gluteus maximus muscle (dorsogluteal) (maximum 4 mL): found on the upper outer quadrant of the buttock (Fig. 20.1C). As suggested above, this should be avoided. Ansell & Dougherty (2011) point out that without correct assessment of the muscle position and an appropriately long needle, many medications are placed into gluteal fat. Zaybak et al (2007) agree, suggesting that the deltoid, rectus femoris or vastus lateralis should all be considered as sites of preference for an obese woman, there being less fat and subcutaneous tissue on these sites than on the buttocks.
• Ventrogluteal site (maximum 2.5 mL), the site of choice: the palm of the midwife’s right hand is placed on the greater trochanter of the woman’s left hip (or vice versa). The index finger is extended to touch the anterior superior iliac crest while the middle finger stretches as far along the iliac crest as possible. The site is in the ‘V’ between the index and middle fingers (Fig. 20.1D).
PHE (2013) recommend the thigh or upper arm as their preferred injection sites for vaccinations, I.M. or S.C.
The volume of solution that the muscle can accommodate seems to be inconclusive (Malkin 2008), the figures suggested above are a guide. The Department of Health (PHE 2013) suggest in their immunization directives that if greater than 4 mL needs to be administered, the dose should be divided and given into different sites.
The muscle should be relaxed for minimal discomfort, the site may be supported by the non-injecting hand and some commentators recommend a slight stretching of the skin prior to needle insertion (Hunter 2008). ‘Bunching up’ the muscle in a thin woman may sometimes be necessary (Workman 1999).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


