25. Principles of drug administration
epidural analgesia
CHAPTER CONTENTS
Epidural analgesia173
Spinal analgesia174
Combined spinal epidural analgesia174
Drugs174
Side effects of epidural and spinal analgesia175
Checking the level of the block178
Postnatal care180
Role and responsibilities of the midwife180
Summary180
Self-assessment exercises180
References181
LEARNING OUTCOMES
Having read this chapter the reader should be able to:
• discuss the differences between epidural, spinal and combined spinal epidural analgesia
• list the indications, contraindications and possible side effects from epidural analgesia
• describe how an epidural is sited and a top-up administered
• discuss the role and responsibilities of the midwife throughout the procedures
• describe how to remove an epidural catheter.
Epidural analgesia generally provides effective analgesia for women in labour compared to other forms of analgesia or no analgesia (Amin-Somuah et al 2005). A 24-hour epidural service is offered in most consultant delivery units using skilled obstetric anaesthetists and midwives who are competent in epidural management (OAA & AAGBI 2005). The epidural rate in the UK is around 25%, although Odibo (2007) suggests the demand is closer to 70–90%; rates in the USA are much higher than the UK at 58% (Simmons et al 2007). This chapter clarifies the terminology and details the procedures for epidural insertion, top-up and removal. The indications, contraindications, side effects and midwife’s role and responsibilities are all highlighted. The reader is encouraged to be aware that the debates surrounding epidural use and normal birth are greater than this text can examine.
Epidural analgesia
Epidural analgesia involves the introduction of a local anaesthetic, often combined with an opioid, into the epidural space (Fig. 25.1). The drugs are able to cross the dura and arachnoid membrane and enter the cerebrospinal fluid (CSF). This allows some of the drug to pass into the spinal cord and bind with opioid receptors, some passes into the systemic circulation whilst the rest attaches to epidural fat (with no analgesic effect) (Chapman 2008).
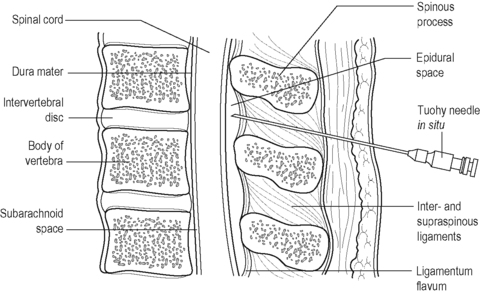 |
| Figure 25.1 • Sagittal section of the lumbar spine with Tuohy needle in the epidural space |
To achieve this, a Tuohy needle is inserted through the lumbar intervertebral space (between L1 and L4) into the epidural space; a fine catheter is threaded through into the epidural space where it is secured in place to allow administration of the drug either as bolus/intermittent doses or as a continuous infusion.
Spinal analgesia
Spinal analgesia is achieved by injecting the drug through the epidural space, dura and arachnoid membrane, into the intrathecal (subarachnoid) space. Lower doses of the drug can be used as it is placed directly into the CSF where the entire drug can bind to the opioid receptor sites in the spinal cord and it is considered to be 10 times more potent than when placed in the epidural space (Chapman 2008). Onset of analgesia is rapid but not as long lasting as an epidural; it is often the analgesia/anaesthesia of choice for emergency caesarean section where rapid anaesthesia is required or for an elective caesarean section.
Combined spinal epidural analgesia
Combined spinal epidural (CSE) analgesia involves injection of the drug into the intrathecal space immediately before or after the placement of the epidural catheter. Often, it is achieved by using the epidural needle to locate the epidural space at the level of L3 then passing a smaller-diameter long spinal needle through the epidural needle lumen to pierce the dura and arachnoid membrane. The drug can then be injected into the CSF and the spinal needle removed to allow the epidural catheter to be inserted into the epidural space and drugs injected into there (Simmons et al 2007). Amin-Somuah & Smyth (2005) suggest CSE combines the advantages of the faster onset and more reliable analgesia achieved with the spinal with the continuing pain relief of the epidural whilst allowing the woman to remain alert.
Drugs
Local anaesthetics (e.g. bupivacaine, ropivacaine) cross the dura and arachnoid membranes, where they are in contact with the nerve roots and spinal cord. Once there, they inhibit nerve conduction by blocking the sodium ion channels that pass the impulses along the nerve fibres, stopping transmission of the painful impulses to the higher centres. The drug dosage determines which nerve fibres are affected; low doses exert a concentration specific effect and can partially selectively block nerve fibres with the smallest diameter (pain) without blocking the larger motor fibres, reducing the amount of leg weakness and immobility experienced (Amin-Somuah et al., 2005 and Chapman, 2008). CSE is able to achieve a good level of analgesia with lower doses of local anaesthesia.
High doses of local anaesthetics result in numbness from the waist down associated with limited/no mobility. There has traditionally been more difficulty with giving birth with an increased risk of instrumental delivery, increased perineal bruising and pain and postpartum incontinence (Simmons et al 2007). As a consequence low dose local anaesthetics are now combined with opioids to limit these effects. Combining lower doses of local anaesthetics with opioids produces better analgesia than higher doses of the individual drugs (Chapman 2008); the risk of instrumental deliveries has decreased and the woman is more likely to have increased mobility during labour (Simmons et al 2007).
Opioid drugs (e.g. fentanyl, diamorphine) combine with the opioid receptor sites to produce an analgesic effect. Fentanyl is lipid soluble and so passes more readily into the CSF, thus is faster acting compared to diamorphine. However, it has a shorter duration (1–4 hours) compared with diamorphine (6–12 hours) (Chapman 2008).
Indications for epidural analgesia
• Pain relief/maternal request.
• Useful where there is likelihood of instrumental or operative delivery, e.g. malposition, malpresentation, multiple pregnancy, prolonged labour.
• Hypertension, where the potential side effects of hypotension can be helpful.
• Preterm labour, where there may be an early desire to push.
• Postoperative analgesia.
Contraindications
There are contraindications for epidural/spinal analgesia, some of which are absolute whilst others are relative:
• coagulation defects due to the increased risk of haematoma formation
• local sepsis
• some neurological disorders, e.g. multiple sclerosis
• known allergy to drugs used
• raised intracranial pressure
• unavailability of appropriately trained staff in setting up and ongoing care of epidurals
• insufficient midwifery staff to provide 1 : 1 care for duration of epidural
• spinal deformity.
Whilst an increased BMI is not a contraindication, it is recognised that there is a higher failure rate when the woman’s BMI is >30 requiring resiting of the epidural (Dresner et al 2006).
Side effects of epidural and spinal analgesia
The side effects associated with epidural and spinal analgesia result from the effects of the drugs used or complications from the procedure itself:
• Opioid side effects: respiration depression (can occur early, within the first 2 hours of administration or later (6–12 hours) and are more likely to occur with diamorphine than fentanyl); sedation; nausea and vomiting; pruritus (itching); urinary retention.
• Local anaesthetic side effects vary depending on the drug and dosage used: peripheral vasodilatation and resulting hypotension (if severe will also cause loss of consciousness); leg weakness; urinary retention; temperature changes (particularly with the vasodilatory effect of bupivacaine which can cause the woman’s feet to be warm, her temperature to rise but her body to shiver).
• Drug toxicity: restlessness, dizziness, tinnitus, metallic taste, drowsiness.
• Anaphylactic drug reaction (see Chapter 18).
• Partial block (‘breakthrough’ pain): contractions are still felt over one area of the abdomen due to non-uniform spread of local anaesthetic (Amin-Somuah & Smyth 2005).
• Dural puncture: the epidural needle or catheter accidentally punctures the dura mater resulting in reduced intracranial pressure with potential severe headache in the following few days (postdural puncture headache, PDPH).
• Catheter migration: extremely rare complication where the catheter migrates into the CSF (can paralyse the respiratory muscles resulting in apnoea, profound hypotension and respiratory arrest) or a blood vessel (resulting in sedation from excess opioids or local anaesthetic toxicity noticed by tingling, numbness, twitching, convulsions, apnoea, loss of consciousness).
• Abscess formation which manifests as back pain and tenderness, erythema, purulent discharge from insertion site.
• Haematoma due to trauma to the epidural blood vessels during catheter insertion or removal which presents with back pain and tenderness accompanied by sensory and/or motor weakness.
• Meningitis: an extremely rare complication manifesting as fever, headache, neck stiffness, photophobia, nausea and vomiting.
There is little consensus as to the incidence of risks occurring in practice as many of the studies are too small to be reliable (Middle & Wee 2009) although the majority of risks are rare. However, Ruppen et al (2006)




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access
