55. Principles of cardiopulmonary resuscitation
maternal resuscitation
CHAPTER CONTENTS
Considerations for child bearing 384
Equipment 385
Role and responsibilities of the midwife 390
Summary 390
Self-assessment exercises 390
References 390
LEARNING OUTCOMES
Having read this chapter the reader should be able to:
• discuss in detail the role and responsibilities of the midwife when resuscitating a pregnant woman
• describe the equipment and how it is used
• demonstrate/simulate a maternal resuscitation technique.
Maternal collapse is fortunately a rare but potentially catastrophic and fatal emergency. This chapter considers effective cardiopulmonary resuscitation for a childbearing woman. The reader is encouraged to read this chapter in conjunction with Chapter 56 (neonatal resuscitation) to compare and contrast the resuscitation skills.
Resuscitation is the means by which life is supported in the event of sudden apnoea or cardiac arrest; cardiac is the most likely cause of arrest in the adult. In the absence of asphyxia, the level of oxygen within the blood is high and it is essential that the circulation is restored quickly and takes precedence over ventilation (Handley 2005). It is now recognised that resuscitation can be effective when high quality cardiac compressions are maintained with minimal delay or interruptions, even when respiratory assistance is not given, thus if the midwife is unable or unwilling to give rescue/ventilation breaths resuscitation can still be successful and cardiac compressions should be commenced as soon as possible.
In a maternity setting where women are healthy and undergoing a physiological process, collapse is both rare and unexpected. The potential for complications does exist, some of which can be life threatening or fatal (CEMD 2004); Lewis (2007) highlights the importance for all staff to have regular audited training to enable them to recognise and manage impending maternal collapse and improve their basic, immediate and advanced life support skills, as poor resuscitation skills were noted to be a feature in a high number of maternal deaths. There are two implications for the midwife:
• the skills of managing maternal cardiopulmonary resuscitation are rarely used
• the need to maintain these skills for use at a moment’s notice remains a priority, wherever the arrest may occur (Nolan 1998).
Considerations for child bearing
Whilst resuscitation techniques are modified for the childbearing woman to accommodate the physiological body changes (Table 55.1) the principles are the same as for any other resuscitation. The crucial difference is that the fetus is also compromised, but the presence of the fetus with its additional circulation may further compromise the mother and make resuscitation more difficult. Successful resuscitation of the mother becomes the priority, such that an emergency caesarean section may be carried out swiftly in order to improve the success of the resuscitation, whatever the gestation of pregnancy (Mitchell 1995).
| Physiological difference | Resuscitation modification |
|---|---|
| Gravid uterus: potential for massive internal concealed haemorrhage | Observations to detect haemorrhage. Prompt infusion using at least two wide bore cannulae, rapid request for cross-matched blood, stat. infusion I.V. fluid up to 2 L, but with careful fluid balance. Use of CVP monitoring |
| Additional circulation (maternal and fetal) causing increased cardiac workload | Caesarean section within 5 minutes if resuscitation not successful. Replace blood loss immediately |
| Aortocaval occlusion when supine | Wedge firmly to the left and manual displacement of the uterus |
| Splinting of diaphragm | May be harder to ventilate the lungs, requiring higher ventilatory pressures |
| Relaxation of cardiac sphincter of the stomach, silent regurgitation and aspiration of stomach contents a possibility | Application of cricoid pressure, use cuffed ET tube when intubated |
| Oedema of glottis, neck obesity, larger breasts | More difficult to intubate, call a skilled anaesthetist who is likely to be successful on the first attempt |
| Increased oxygen requirements | Begin resuscitation quickly using 100% oxygen |
A fewer number of modifications will be required for a newly delivered woman, but some of the physiological changes will remain. Silent regurgitation of the stomach contents is still a possibility until progesterone levels have returned to their prepregnant state. Cricoid pressure (gentle downward pressure on the cricoid cartilage to occlude the oesophagus) or intubation is a valuable means of preventing regurgitation of the stomach contents and should be considered for a childbearing woman from the moment of collapse (Fig. 55.1).
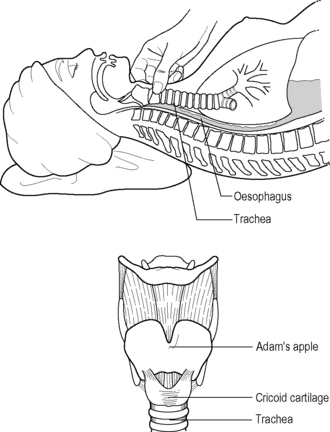 |
| Figure 55.1 • Application of cricoid pressure (Adapted from Fraser & Cooper 2003) |
Anticipation and recognition of collapse
This is not an exhaustive list. Arrest can sometimes be averted by administering 100% oxygen, repositioning into a left lateral position, giving a bolus of intravenous (I.V.) fluid and then calling medical assistance.
Recognition of collapse
In the event of collapse, the midwife will make an assessment initially based on colour, movement, breathing and heart rate. There may be some variations according to the cause of the arrest, but generally the following features will be noted:
• colour: pale, cyanosed (heavily so if amniotic fluid embolism), clammy
• movement: no response to stimulation; midwife may have observed seizure or twitching immediately prior to arrest; woman will be slumped as if fainted
• breathing: absent, no rise and fall of the chest, no breath sounds heard or felt
• heart rate: absent (use major pulse, e.g. carotid (see p 38)).
Equipment
While some basic equipment is desirable, it is possible to complete a successful resuscitation without any equipment; however, the midwife usually has access to some equipment. Wherever the setting, protection from contact with body fluids is indicated by using facemasks rather than undertaking mouth-to-mouth resuscitation. Equipment should be checked regularly to ensure that it is present and working effectively. Cleaning and maintaining equipment is indicated according to manufacturers’ instructions. A wedge is required for the pregnant woman; this should be firm enough to permit effective chest compression. Adaptations may be made in the home using books, files or other appropriate items.
Standard equipment includes:
• oxygen
• suction apparatus
• bag and facemask for ventilation (with oxygen reservoir) or pocket mask
• wedge
• Guedel airways, sizes 2 and 3
• resuscitation drugs
• stethoscope
• laryngoscope
• cuffed endotracheal (ET) tubes size 7–9 mm and 10 mL syringe
• introducer
• laryngeal mask airway
• connectors and bag for ventilator
• CVP line
• cannulae, I.V. lines and blood bottles
• defibrillator and cardiac monitor.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


