Chapter 1 Prescriptions, labels and SI units
The prescription
Prescribers, whether they are doctors, pharmacists or nurses, are legally bound to follow standard practice in prescribing and administration (Medicines Act 1968).
A prescription (now defined as a health prescription) means “a prescription issued by a doctor, a dentist, a supplementary prescriber, a nurse independent prescriber or a pharmacist independent prescriber” under or by virtue of the appropriate Acts and Orders (RPSGB 2009, p. 5).
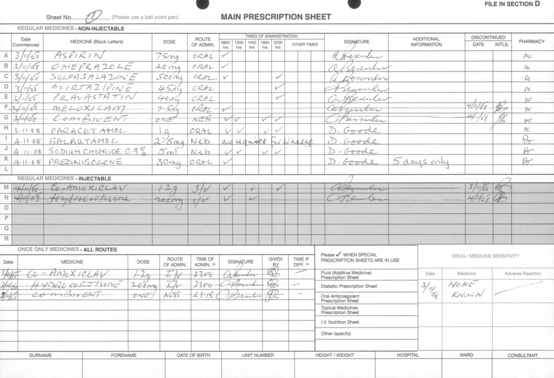
Hospital medicine administration may be more complex than medicine administration in the community. It is based on prescriptions written on forms specially designed for the purpose (Fig. 1.1). Whatever form the prescription takes or however it is generated, as well as the patient’s biographical details, it is always necessary to include the following information:
The patient’s height and weight should also appear on the prescription sheet, especially where the dose is dependent on body weight or body surface area (see pp. 50–54).
The form used will have a facility to record the individual doses administered.
Electronic prescribing
Most drug administration is based on the interpretation of a prescription, which may be handwritten or computer-generated. Electronic prescribing, linked with automated drug selection is being increasingly developed in the UK. The advantages claimed for such systems include a reduction in medication error rate and a reduction in medicine supply turnaround times (Goundrey-Smith 2006).
Contents of a prescription
Dose
The dose of a drug is influenced by many factors. In the first place, the inherent properties of the drug or medicine (e.g. solubility, duration of action, bioavailability, activity, and formulation) must be taken into account. Having considered the properties of the drug and formulation, account must be taken of a whole range of issues relating to the patient and his/her condition before a dose is determined. In many cases, the standard dose will be applicable but careful consideration must be given to the age of the patient, the patient’s ability to excrete or metabolise the drug, and the presence of co-existing conditions. In some situations, it may be necessary for the prescriber to deviate from standard doses and calculate the dose to be given to the patient based on physiological and other parameters. These calculations are based on factors such as blood levels and creatinine clearance. Having determined the dose to be given, a good outcome for the patient can only be achieved if the administration is accurate in all respects.
Route
Many of these factors are interrelated but thanks to modern drug formulation and delivery systems it is generally possible to use a route of administration that best suits the patient’s need (see Box 1.1).
Nurses’ responsibilities regarding prescriptions
The standards set for registered nurses and midwives (NMC 2008) in relation to prescriptions include: