The population screen shows each client’s name, risk score, gender, and counts of key events including: (1) Episodes – key risk areas, (2) Claims – total claims, (3) Office – office visits, (4) RX – prescriptions filled, (5) IP – inpatient admissions, (6) ER – outpatient emergency room visits, (7) LTC – long term care services, (8) Lab – laboratory, (9) Providers – unique number of providers, (10) AOD – alcohol and drug treatment, (11) MH – mental health services, (12) CARE – long-term care functional assessments, and (13) HRI – health risk indicators.
Once an individual patient is chosen, the PRISM tool organizes data much as a sophisticated electronic medical record would, with summary sheets on major topics, use of graphic displays for conveying dense information, the ability to sort all fields, and the ability to drill down (connect through hyperlinks) for more detailed information.
Table 20.1 Client-Specific PRISM Summaries
Source: Billings, Parikh, & Mijanovich (2000)
| Summary Topics by Tab | Data |
| Medical Risk Factors | By disease category, reports the most recent diagnosis and/or prescription, number of claims and relative contribution to the total risk score |
| Hospitalizations | Admission and discharge dates, total cost, primary diagnosis, whether admission was through the emergency department, length of stay, drill-down links to hospital and attending physician contact information, and access to the complete claim |
| Outpatient Emergency Department Visits | Date, primary diagnosis, paid amount, classification of whether the visit was avoidable (using the New York University algorithm (Billings, et al. 2000), name of hospital, with drill down to hospital contact information |
| Prescriptions Filled | Fill date, generic drug name, drug class, quantity, days supplied, reimbursement, pharmacy, prescriber, and refill sequence |
| Office Visits | Date, claims line number, drug indicator, primary diagnosis, procedure, revenue code, provider (including a link to contact information), line amount, paid amount and claim type |
| Lab Orders Filled | Date, procedure, revenue code description, provider, paid amount, referring provider |
| Substance Abuse Services | Admission date, discharge date, quantity, description of service |
| Mental Health Services | Service date, service code, quantity, unit, description of service |
| Long-Term Care | Service date, service code, quantity, unit, description of service |
| Long-Term Care Needs Assessment | By assessment identifier, type of assessment, whether it is current or historical, assessment date and detailed assessor’s notes. Sub-screens provide additional detail including activities of daily living (ADL) score, cognitive performance score, depression score, change in health status from last assessment, self-rated health status, detailed description of behavioral problems and functional limitations, fall risk, pain impacts on functioning, and identification of long-term care caseworker and primary care physician (including contact information) |
| Health Risk Indicators (For Clients Age 18 and Under) | Risk score; substance use disorder diagnosis subsequent to last treatment encounter, inpatient admissions in last 12 months, outpatient ER visits in last 12 months, failure to thrive diagnosis, treatment for injury diagnosis, nutrition problem diagnosis, crisis mental health encounter (past 12 months), mental health inpatient stay (past 12 months), outpatient ER with primary psychiatric diagnosis (past 12 months), child under age 6 receiving psych RX in past 12 months. |
| Providers | Most likely primary care providers based on an attribution model, name of billing and performing provider, last service date and number of claims with links to all visits with provider contact information |
| Eligibility | By year/month, patient’s living arrangement, placement status, whether they are dually eligible for Medicare, their Medicaid program coverage group and the type of managed care provider or care coordination coverage they have, with links to contact information |
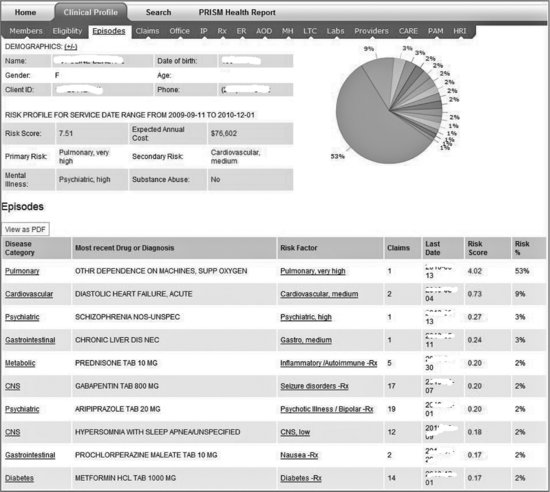
Each summary sheet can be printed out as a .pdf document. Client-specific summary sheets all share synopses of demographics (including name, age, gender, phone, current address, whether hearing impaired, the need for interpreter services) and a risk profile (risk score, expected annual cost, primary and secondary risk conditions and diagnoses, mental health and substance use indicators), with topic-specific detail, as illustrated in Table 20.1 A pie chart illustrates the relative contribution of each risk factor to the client’s total risk score. Full descriptions of each risk factor are viewed by hovering the cursor over each section of the pie chart.
The summary sheet of risk factors (Figure 20.2) is usually the first stop for a clinician reviewing a client for the first time.
In this example, the primary risk factor, pulmonary, is very high, making up 53% of the patient’s total risk score of 7.51. PRISM lists the most recent description of the drug or diagnosis for that risk factor, with links to all claims associated with the condition. By scanning the risk factor list, the clinician can discern which risk factors may respond to intervention. The risk factors don’t substitute for professional judgment; they act as supplements. The designers of PRISM chose to not load the risk factor page with multiple alerts based on single disease protocols, because prior experience showed that too many alerts diverted attention away from what might have been the root source of the patient’s dysfunction. Instead, the focus was on building an application that allowed the user’s attention to scan the breath of information on a client, looking for clues as to where care management may have an impact.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree