7 Placement learning pathways
• To explore the cancer and palliative care placement
• To understand how each team/specialty works in the practice placement
• To understand the health and safety requirements in the departments that may be visited from the hub placement
• How to plan insight visits and opportunities as part of the practice placement
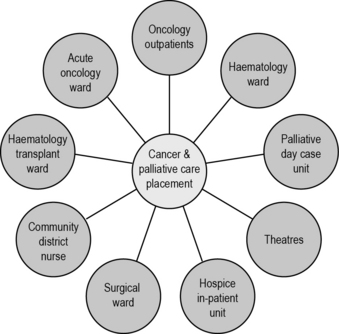
The cancer and palliative care placement
The ‘hub and spoke’ model in Figure 7.1 is supported by the NMC. It gives you the opportunity to be allocated to one clinical area for a period of time while also having the opportunity to be allocated to a spoke area and short insight visits.
The length of the placement may depend on the year of study as well as local arrangements between the university and clinical areas. Box 7.1 outlines a theoretical example of what a first year nursing student’s 18-week (‘year-long’) placement might look like. This sample placement demonstrates a wide range of learning opportunities that can stem from a core hub placement. It is important to remember that a cancer patient can be nursed in any clinical environment. Some placements will be much shorter than this, most ranging between 8 and 12 weeks. This is dependent on the school of nursing and your stage of training.
Box 7.1 A theoretical example of a first year nursing student’s 18-week placement
Weeks 6–7: Spoke – oncology outpatients
Initial patient consultation, treatment decision making, follow-up clinics.
Insight visits: oncologist, site-specific nurse specialist, radiology investigations.
Weeks 11–13: Spoke – palliative day care
Insight visits: pharmacist, end of life coordinator, pain specialist team.
How each team/specialty works in the practice placement
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree