Chapter 28 Physiological changes during the postnatal period
Learning outcomes for this chapter are:
1. To describe the change in maternal hormone levels following the birth of the baby
2. To describe the processes of involution and of healing at the placental site
3. To provide a physiological rationale for blood and fluid loss during the puerperium
4. To describe the changes which occur in the cervix, vagina and vulva in the puerperium
5. To compare physiological changes in the maternal body systems during pregnancy and during the postnatal period, particularly the renal, haematological and cardiovascular changes
6. To identify physiological vulnerability during the puerperium
7. To outline the hormonal control of lactation during pregnancy and the puerperium.
decidua, deep vein thrombosis (DVT)
fibrin degradation products (FDPs)
follicle-stimulating hormone (FSH)
gonadotrophin-releasing hormone (GnRH)
human chorionic gonadotrophin (hCG)
human placental lactogen (hPL)
partial pressure of arterial carbon dioxide (PaCO2)
This chapter focuses on the physiological processes associated with the postnatal period or puerperium. The puerperium refers to the 6–8 weeks following birth when the reproductive organs return towards a non-pregnant state, and lactation begins. Many of the physiological, anatomical and endocrine changes in this period occur in the first 10–14 days as hormone levels adjust following birth of the placenta. While the reproductive organs heal and regain a shape and structure similar to before pregnancy, other systems of the body that changed to support pregnancy now also return to their former function. These processes are the focus of this chapter. An understanding of the physiology underpinning these changes should help a midwife assess the wellbeing of the woman and baby. Further readings are provided at the end of the chapter for a more in-depth exploration of specific topics.
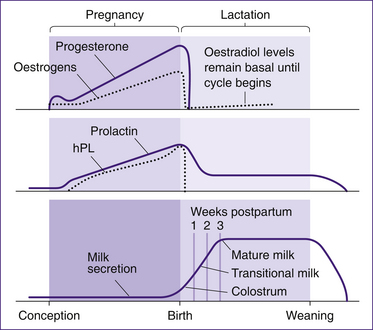
HORMONAL CHANGES
The placental hormones human placental lactogen (hPL), human chorionic gonadotrophin (hCG), the oestrogens and progesterone control maternal physiology in pregnancy to provide an optimal environment for fetal development. The return of the body systems to a non-pregnant state is largely governed by the removal of the placental hormones. Following birth of the placenta, metabolism of circulating hormones and hormone stores results in a rapid drop in placental hormone levels. These changes are illustrated in Figure 28.1. Human placental lactogen is absent from the plasma within 1–2 days; hCG is not detected in the urine by 7–10 days; and oestrogens and progesterone reach basal levels by 7 days (Blackburn 2007). After birth, prolactin levels also drop significantly but are maintained above normal for 3–4 weeks even in the absence of suckling (Johnson 2007).
INVOLUTION OF THE UTERUS
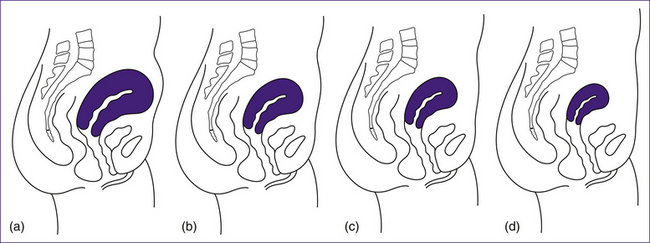
The uterus reduces in size immediately following birth, due to myometrial contractions, and then continues to reduce in size over the next few days and weeks, until it returns to being a pelvic organ. This process is termed involution. During this time the height of the fundus usually decreases by about 1 cm/day, and by 10 days the fundus cannot be palpated abdominally as the uterus has descended into the pelvis (Blackburn 2007).
Oxytocin continues to be released from the posterior pituitary after the birth of the placenta and membranes. It stimulates strong intermittent contractions of the uterus, leading to collapse of the uterine cavity, which no longer contains the fetus, and thus to realignment of the uterine walls in apposition to each other (Blackburn 2007). This aids the process of haemostasis (stoppage of bleeding) and also reduces the size of the uterus immediately following birth.
The uterus decreases from 1 kg to about 350 g in the first two weeks following birth and then decreases more slowly over the next six weeks to approximately 60–80 g (Blackburn 2007). This process involves a reduction in the thickness of the myometrium, a shedding of the decidua and regeneration of the endometrium. Although the exact mechanisms involved are unclear, the rapid withdrawal of the placental hormones appears to facilitate the changes (Stables & Rankin 2005). Retained placental fragments or pelvic infection can slow involution.
Changes to the myometrium
Changes in the collagen and elastin content of the cells, along with water and protein loss, aid the process of involution (Stables & Rankin 2005). Withdrawal of oestrogen reduces protein synthesis in the muscle fibres. Blood flow is reduced to the myometrium as the uterus contracts and compresses the uterine blood vessels. The resulting ischaemia aids in destruction of myometrial cells. Proteolytic enzymes digest superfluous actin and myosin protein in the muscle cells by a process termed autolysis. The size of the muscle cells is reduced, rather than the number of cells (Blackburn 2007). The products of autolysis, as well as excess fibrous and elastic tissue, are engulfed by macrophages—a process called phagocytosis. A proportion of fibrous and elastic tissue remains within the uterus and increasing amounts may remain following further pregnancies; thus the uterus never returns fully to the pre-pregnant state (Stables & Rankin 2005).
Regeneration of the endometrium
In the first 2–3 days following the birth, the epithelial lining differentiates into two layers: a superficial layer and a basal layer. A cellular barrier to infection is formed by the superficial layer of granulation tissue and by the invasion of leucocytes (macrophages and lymphocytes) that enter the
area to clean up the debris and microbes. This layer breaks down and necroses, and is shed as lochia over the next 4–6 weeks. Regeneration of the decidual layer surrounding the placental site takes 2–3 weeks, and by 16 days this layer is similar to the non-pregnant endometrium in the proliferative phase of the menstrual cycle (Blackburn 2007). The placental site heals gradually over 6–7 weeks (Stables & Rankin 2005). Large blood vessels that supplied the intervillous spaces are blocked by invading fibroblasts. Healing occurs by exfoliation without the formation of scar tissue. Endometrial tissue heals inwards from the edges of the placental site and upwards from the endometrial glands.
Afterpains
Contraction of the uterine muscles is felt as ‘afterpains’ for 4–7 days and is strongest 12–24 hours postpartum, especially in multiparous women. These contractions facilitate the process of involution. Afterpains may occur in association with breastfeeding, due to the release of oxytocin and uterine contractions, or they may occur independently of breastfeeding. For some women these contractions are very intense and may be similar to the severity of labour pains (Marchant et al 2000). Women may require analgesics. There is little research on the subject, but one study showed that high-frequency transcutaneous electric nerve stimulation (TENS) was successful in reducing pain and discomfort of postpartum uterine contractions (Olsen et al 2007).
LOCHIA
Lochia refers to the discharge from the vagina that continues over the 3–6 weeks following birth. Lochia changes in appearance over time, and between 150 mL and 400 mL of lochia can be lost in total (Blackburn 2007).
Red lochia (lochia rubra) is described as red or dark brown with a fleshy smell and is discharged for the first few days, up to a week. This lochia contains mainly blood and pieces of chorionic villi from the placental site, shreds of amnion and chorion, leucocytes, epithelial cells, vernix, lanugo and meconium. During the second and third weeks the discharge tends to change to a pinkish-brown colour, and this is known as pink lochia (lochia serosa). Pink lochia contains blood, mucus, erythrocytes, leucocytes, microorganisms and superficial decidual cells. Following this, white lochia (lochia alba), a whitish-yellow discharge, continues until 3–6 weeks postpartum. It is similar in composition to pink lochia but does not contain erythrocytes (Blackburn 2007).
However, the description of the changes in lochia as reported above are not supported by a recent prospective survey of 524 women in the United Kingdom who self-reported considerably more variation in the duration, amount and colour of their lochia. The median duration of vaginal loss was 21 days among these women, and the colour of the fluid was most consistently reported as red/brown in colour (Marchant et al 1999). Further discussion of lochia can be found in Chapter 29.
Critical thinking exercise
In a UK study, Marchant et al (1999) collected data from 524 women, using structured diaries, concerning postnatal vaginal loss on days 2–10, days 14, 21 and 28 and again at 3 months. Forty-nine of the 161 primiparous women reported being either surprised or shocked at the amount of blood loss they experienced. Twenty-two per cent of the women reported that they had been worried about their vaginal blood loss during the period 28 days to 3 months (Marchant et al 2000).
Lochia is sterile until it reaches the vagina. However, it is an excellent medium for the growth of bacteria. Puerperial infection may result from the invasion of endogenous organisms, those that are normally present in the woman’s body, or from exogenous organisms, introduced to the woman’s body from elsewhere (e.g. from another person). The woman is particularly vulnerable to infections during the puerperium due to the open wound at the placental site, the tissue trauma associated with labour and the excellent culture medium provided by the decidua and lochia (Stables & Rankin 2005).