Chapter 25 Physical Problems and Complications in the Puerperium
Immediate untoward events for the mother following the birth of the baby
Postpartum haemorrhage
 Immediate (primary) postpartum haemorrhage (PPH). This is the most immediate and potentially life-threatening event occurring at the point, or within 24 hours, of delivery of the placenta and membranes. It presents as a sudden and excessive vaginal blood loss of 500 ml or more. (See Ch. 19 for management.)
Immediate (primary) postpartum haemorrhage (PPH). This is the most immediate and potentially life-threatening event occurring at the point, or within 24 hours, of delivery of the placenta and membranes. It presents as a sudden and excessive vaginal blood loss of 500 ml or more. (See Ch. 19 for management.)
 Secondary or delayed PPH. This is where there is excessive or prolonged vaginal loss from 24 hours after delivery of the placenta and for up to 12 weeks postpartum. Unlike primary PPH, which includes a specified volume of blood loss as part of its definition, there is no such volume defined for secondary PPH.
Secondary or delayed PPH. This is where there is excessive or prolonged vaginal loss from 24 hours after delivery of the placenta and for up to 12 weeks postpartum. Unlike primary PPH, which includes a specified volume of blood loss as part of its definition, there is no such volume defined for secondary PPH.
Regardless of the timing of any haemorrhage, it is most frequently the placental site that is the source. Alternatively, a cervical or deep vaginal wall tear or trauma to the perineum might be the cause in women who have recently given birth. Retained placental fragments or other products of conception are likely to inhibit the process of involution, or reopen the placental wound. The diagnosis is likely to be determined by the woman’s condition and pattern of events and is also often complicated by the presence of infection (see Box 25.1).
Box 25.1 Secondary PPH
Treatment
• Reassure the woman and her support person(s)
• Rub up a contraction by massaging the uterus if it is still palpable
• Encourage the mother to empty her bladder
• Give an uterotonic drug, such as ergometrine maleate, by the intravenous or intramuscular route
• Keep all pads and linen to assess the volume of blood lost
• Antibiotics may be prescribed
• If retained products of conception are seen on an ultrasound scan, it may be appropriate to transfer the woman to hospital and prepare her for theatre
Postpartum complications and identifying deviations from the normal
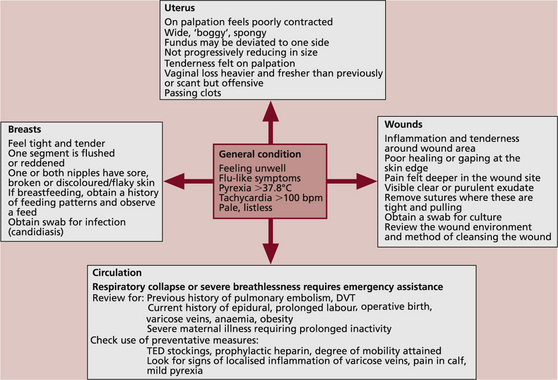
The midwife needs to establish whether there are any signs of possible morbidity and determine whether these might indicate the need for referral. Figure 25.1 suggests a model for linking together key observations that suggest potential risk of, or actual, morbidity.
 A rise in temperature above 37.8°C is usually considered to be of clinical significance. A mildly raised temperature may be related to normal physiological hormonal responses: e.g. the increasing production of breast milk.
A rise in temperature above 37.8°C is usually considered to be of clinical significance. A mildly raised temperature may be related to normal physiological hormonal responses: e.g. the increasing production of breast milk.
 A weak and rapid pulse rate in a woman who is in a state of collapse with signs of shock and a low blood pressure, but no evidence of vaginal haemorrhage, may indicate the formation of a haematoma. A rapid pulse rate in an otherwise well woman might suggest that she is anaemic but could also indicate increased thyroid or other dysfunctional hormonal activity.
A weak and rapid pulse rate in a woman who is in a state of collapse with signs of shock and a low blood pressure, but no evidence of vaginal haemorrhage, may indicate the formation of a haematoma. A rapid pulse rate in an otherwise well woman might suggest that she is anaemic but could also indicate increased thyroid or other dysfunctional hormonal activity.
 The midwife needs to be alert to any possible relationship between the observations overall and their potential cause, keeping common illnesses in mind – e.g. the woman may have a common cold.
The midwife needs to be alert to any possible relationship between the observations overall and their potential cause, keeping common illnesses in mind – e.g. the woman may have a common cold.
The uterus and vaginal loss following vaginal birth
Assessment of uterine involution is needed where the woman:
Morbidity might be suspected where the uterus:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree