Chapter 18 Phototherapy
INTRODUCTION
Hyperbilirubinaemia, commonly referred to as jaundice, is a condition wherein the production of bilirubin is greater than its elimination (Boyd 2004). Management of this condition is dependent on the cause and can be either by phototherapy or in extreme cases, by exchange transfusion. This chapter will review the use of phototherapy which consists of the application of fluorescent light to reduce the serum bilirubin level of an infant. This light is normally a mixture of blue and white radiant light and is not in the ultraviolet range (Metherall 2003).
RATIONALE
The primary aim of phototherapy is to prevent kernicterus, i.e. severe, permanent neurodevelopmental handicap caused by persistent raised serum unconjugated bilirubin (Stokowski 2006, Boyd 2004).
FACTORS TO NOTE
Normal red blood cell life in the adult human is approximately 120 days. In the neonate this is reduced to a lifespan of between 40 and 70 days (Boyd 2004).
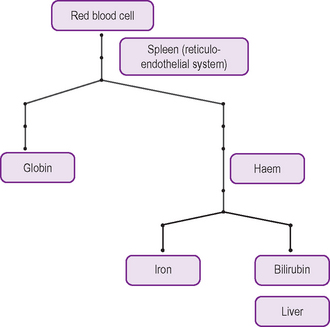
Red blood cells are broken down in the spleen (by the reticuloendothelial system) and to a lesser extent in the liver. Bilirubin is one of the end-products of red blood cell breakdown, being derived from the haem part of haemoglobin (Fig. 18.1). Bilirubin, unconjugated, is not water soluble and is toxic to the body at high levels. If not converted to the water-soluble (conjugated) bilirubin, the unconjugated bilirubin will be deposited in the brain cells, which will lead to a condition called kernicterus (Stokowski 2006).
Unconjugated bilirubin is transported in the bloodstream bound to albumin, a plasma protein, to the liver where, following a complex process of enzyme actions, it is converted to conjugated bilirubin (Stokowski 2006).
Conjugated bilirubin is water soluble and is excreted by the liver via the biliary system into the intestine (Stokowski 2006).
In the intestine the bilirubin is converted to urobilinogen, some of which is absorbed by the enterohepatic circulation and is eventually excreted in the urine. The majority of the urobilinogen is oxidised in the colon to a brown pigment, urobilin, which is excreted in the stool (Merenstein & Gardner 2006). An increase in serum bilirubin causes jaundice, a yellow/amber discoloration of the skin, also seen in the sclera of the eyes and mucous membranes (AAP 2004). This is seen when the serum bilirubin rises above 80 micromoles (μmol) per litre. Approximately 60% of normal newborns will be clinically jaundiced sometime during the first week of life (Maisels & McDonagh 2008). Often, the nurse who notices the infant’s jaundice initiates the checking of the serum bilirubin level (Truman 2003). In the majority of cases this is relatively benign; however, close monitoring of the serum bilirubin level is important because of the risk of kernicterus (Maisels & McDonagh 2008).
An early high level of serum bilirubin, normally within the first 24 h of life, may indicate ABO or Rhesus incompatibility. Persistent jaundice after the first week of life must be fully investigated to determine the cause. Biliary atresia is one condition where the prognosis is improved with an early diagnosis (Merenstein & Gardner 2006, Kelly & Davenport 2007).
Breast milk jaundice is a benign condition, which may persist up to 3 months after birth and is thought to be caused by a factor within the breast milk which inhibits bilirubin conjugation (Percival 2003, Alex & Gallant 2008).
Estimations can be made using a transcutaneous bilirubin monitor; however, the serum level should always be obtained before phototherapy is commenced (Truman, 2003). Phototherapy is ineffective before the infant is jaundiced; hence it cannot be used prophylactically. However, early use in infants with known haemolytic disease is indicated as a means of control of the serum bilirubin level. Initiation of therapy is dependent not only on the serum bilirubin, but also the gestational age at birth of the infant (Percival 2003). Pre-term and sick infants are more prone to the complications of jaundice; hence phototherapy is initiated at lower serum bilirubin levels.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree