Infant—prenatal and postnatal history, nutrition, development.
Toddler—home environment, safety issues, development, parent’s response.
School-age—school, friends, reaction to previous hospitalizations.
Adolescent—alcohol, drugs, friends, sexual history, relationships with parents, identity.
Date and time.
Health care provider’s name and telephone number, if known.
Insurance data.
Patient’s name, address, telephone number, birth date.
Referring health care source (eg, school, other health care provider, clinic).
Identify the care person in charge of the patient by name and relationship to the patient; obtain a relative’s or care person’s address and home and work telephone numbers, if different from those of the patient.
To make the informant feel more at ease, the questions should begin in a friendly, nonthreatening manner. Questions addressed to the parent should be phrased appropriately.
Casual, friendly responses or remarks on the part of the interviewer may also help break the ice, such as:
“Whoever takes care of this baby certainly does a good job.”
“That is a lovely outfit the baby is wearing.” (Remember that families will usually put good clothes on a baby for a visit to a health care agency.)
Sometimes repeat the information to verify data. This will give you a better judgment of the care person’s cooperation and reliability.
If age appropriate, get some data directly from the child.
Write an exact description of the complaint.
Use quotation marks to clearly indicate that the informant’s words are being used. It is helpful to explain:
“I will write it down so there will be no mistake.”
“Let me read this back to you to make sure it is correct.”
Quotation of the care person’s exact words may give an indication of how he feels about the symptoms; it may reflect fear, guilt, defensiveness.
Begin with a helpful, open-ended question. That is the first overture made to this patient:
“How have things been going?”
“Please tell me the reason for your coming here today.”
“Do you have any particular worries or concerns about the baby?”
Then proceed to more specific questions.
The information obtained may indicate the natural history of the disease, if one is present, and its gradual evolution. Pursue the information with a series of probing questions.
“How long has the baby (child) had this problem?”
If the informant cannot remember, try another route: “When did he (or she) last act well?”; “Do you remember last Christmas? Did the baby have the trouble then?”
Write down the responses; try to assess, as more questions are asked, how accurate the informant’s answers may be.
Body location—of pain, itching, weakness.
Quality and quantity of complaint—both type (a burning pain) and severity (knifelike, comes and goes).
Degree of symptom—(eg, pain, how severe; cough, day and night; eye drainage, amount).
Chronology—indicate time sequence and whether the problem is episodic (lasts for a while and then clears up completely).
Environment or setting—where and when the symptoms occur.
Aggravating and alleviating factors—what makes the pain worse or better.
Associated manifestations or symptoms—accompanied by vomiting, blurred vision.
Typically, a carefully written description of a symptom will be the source of a future diagnosis and will serve all who are involved in helping the patient.
Do not worry about how many notes you have to take at first.
You will be able to recheck this information when you do the review of systems.
Family members—mother’s age and state of health, father’s age and health, siblings—who is at home with you?
Family health history:
Eyes, ears, nose, throat—nosebleeds, sinus problems, glaucoma, cataracts, myopia, strabismus, other problems of eyes, ears, nose, throat.
Cardiorespiratory—tuberculosis, asthma, hay fever, hypertension, heart murmurs, heart attacks, strokes, rheumatic fever, pneumonia, emphysema, other problems.
Gastrointestinal—ulcers, colitis, vomiting, diarrhea, other problems.
Genitourinary—kidney infections, bladder problems, congenital abnormalities.
Musculoskeletal—congenital hip or foot problems, muscular dystrophy, arthritis, other problems.
Neurologic—seizures, epilepsy, nervous disorder, mental retardation, emotional problems, comas, headaches, others.
Chronic disease—diabetes, liver disease, cancer, tumors, anemia, thyroid problems, congenital disorder.
Special senses—anyone deaf or blind.
Miscellaneous—other medical problem not mentioned.
Family social history:
Residence—apartment or house and size. Yard, stairs, proximity to transportation, shopping, playground, school, safe neighborhood? City or well water?
Financial situation—who works, where employed, occupation, welfare, food stamps.
Primary care person—babysitters, day-care center.
Family interrelationships—happy, cooperative, antagonistic, chaotic, multiproblem, violent.
Pregnancy—planned or not; source of care; approximate date of seeking care; birth order of this pregnancy, including miscarriages. This area of the history may be one of great sensitivity. Try to make the questions gentle and supportive:
“Did you plan a baby around this time?”
“When did you manage to get your first checkup for the pregnancy?”
“Were there any unusual problems related to your pregnancy or delivery?”
Maternal health—includes illnesses and dates, abnormal symptoms (eg, fever, rash, vaginal bleeding, edema, hypertension, urine abnormalities, sexually transmitted disease). Avoid technical words, if possible.
“Were the doctors or nurses worried about your health?”
“Were your rings tight?”
“Do you know if your blood pressure went up?”
“Did you have trouble with your urine?”
Weight gain—validate by trying to get a figure for nonpregnant weight and weight at delivery.
Medications taken—eg, vitamins, iron, calcium, aspirin, cold preparations, tranquilizers (“nerve medicine”), antibiotics; use of ointments, hormones, injections during pregnancy; special or unusual diet; radiation exposure; sonography; and amniocentesis.
Quality of the fetal movements—when felt?
Use of alcohol, tobacco, or drugs during pregnancy.
Expected date of delivery and approximate duration of pregnancy.
Place of delivery and name of person who conducted the delivery.
Labor—spontaneous or induced, duration, and intensity.
Analgesia or anesthesia.
Type of delivery—vaginal (breech or vertex presentation); cesarean delivery; forceps delivery.
Complications (eg, need for blood transfusion or delay in delivery).
Condition of infant.
Color (if seen) at delivery.
Activity of infant.
Type of crying heard.
Breathing abnormality.
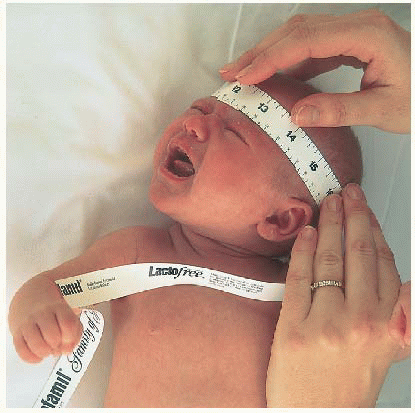
Birth weight and length.
Problems that occurred immediately at birth.
Duration of hospitalization of the mother and infant.
Problems with baby’s breathing or feeding.
Need of supportive care (eg, oxygen, incubator, special care nursery, isolation, medications).
Weight changes, weight at discharge, if known.
Color—cyanosis or jaundice.
Bowel movements—when.
Problems—seizures, deformities identified, consultation required.
Hearing—was a hearing screen conducted in the nursery? The United States Preventative Services Task Force recommends universal screening for all newborns using otoacoustic emissions and/or auditory brain stem response testing. The guideline is available online at www.guideline.gov/content. aspx?id=12640.
Mother’s contact with the baby and her first impression:
“What was it like when you first saw your baby?”
“What did the baby do when you were first together?”
Breast- or bottle-fed? What formula? How prepared?
Amounts offered and consumed.
Frequency of feeding—weight gain.
Addition of juice or solid foods.
Food preferences or allergies.
Feeding problems—variations in appetite.
Age of weaning.
Vitamins—type, amount, regularity.
Pattern of weight gain.
Current diet—frequency and content of meals.
Past weights and lengths, if available.
Milestones—sat alone unsupported; walked alone; used words, then sentences.
Teeth—eruption, difficulty, cavities, brushing, flossing.
Toilet training.
Current motor, social, and language skills.
Sexual development.
Infant—swollen breast tissue, vaginal discharge, hypertrophy of the labia.
Toddler or school-age child—early development of breasts or pubic hair.
Prepubertal or pubertal child—in girls, time of development of breasts and pubic hair and onset of menstruation. In boys, time of enlargement of testes and penis, development of pubic and facial hair, and voice changes.
Immunizations—rubella, rubeola, mumps, polio, diphtheria, pertussis, tetanus toxoid, varicella, pneumococcal, bacille Calmette-Guérin, influenza, Haemophilus influenzae type b, hepatitis A and B, meningococcal conjugate, human papillomavirus, and rotavirus. Indicate number and dates. Recommended immunization schedules are available online at www. cdc.gov/vaccines/recs/schedules/.
Screening procedures—hematocrit or hemoglobin level, urinalysis, tuberculin testing, visual and auditory acuity, color vision, lead testing, cholesterol screening, syphilis testing, HIV testing, gonorrhea and chlamydia screening.
Dental care—source and frequency of care, dental hygienist visits, fillings, extractions, last checkup.
Dates, hospital, health care provider.
Indications, diagnosis, procedures.
Complications.
Reactions to previous hospitalizations.
Emergency department visits—frequency and diagnosis.
Fractures—location and treatment.
Trauma, burns, bruises.
Ingestions.
Ask the parents about provision of a safe environment; for example, cleaning supplies out of reach, electrical outlets with appropriate covers, guns in the house unloaded and kept in a locked room or cabinet, water safety education. Ask about use of safety equipment, such as seat belts, bike helmets, childproof safety caps on medications.
For general use, such as vitamins, antihistamines, laxatives.
Special or fad diets.
Recent antibiotics.
Routine use of aspirin.
Hormonal contraceptives—types, dose, duration.
Drugs, opioids, marijuana, hallucinogens, mood elevators, tranquilizers, alcohol.
Determine when last dose of medication was taken; is the medication with the patient? How does the child take the medication?
Allergy to medication?
Present and past schooling, grade, and performance.
Favored and least-favored subjects.
School-related behavior—anxious to go, anxious to stay home.
General attitude toward school and career plans; attitude toward peer groups.
Gang dress or behavior.
Straightforward questions to a child (eg, “What grade are you in?”; “Who are your friends?”).
Three wishes offered to the child:
“If your birthday were here, what would you ask for?”
“If you could be anyone, who would it be?”
“What would be the best thing that could happen to you?”
“Who is your best friend?”
Questions to parents: “How does that seem to you?”
Adolescents—Interviews with older children and teens may start with the parents present but the child should also be provided with some private time away from the parents to discuss concerns. The parents should also be allowed a brief time away from their child to voice any concerns.
Emphasize the positive (eg, “What is your best subject?”)
Environment—rural, urban.
Housing—type, location, heating, sewage, water supply, family pets, other animal exposure.
Parents’ occupations (employment) and marital status.
Number of individuals living in home, sleeping arrangements.
Religious affiliations.
Previous utilization of social agencies.
Health insurance and usual source of care.
After assuring older children of the confidentiality of their answers, inquire about risk-taking behaviors, such as cigarette smoking, alcohol and drug use, drinking and driving, and sexual history.
“Can you tell me a little bit about your home?”
“I need to know more about how you live to help you with your child’s problem.”
Hygiene.
Exercise.
Sleep habits.
Elimination habits.
Activities, hobbies, special talents.
Friends, teacher relationships.
Sibling and parent relationships.
Expression of emotions.
Blows up easily.
Quiet.
Idiosyncratic behavior and habits (eg, thumb-sucking, nailbiting, temper tantrums, head-banging, pica, breath-holding, rituals, tics).
Emotional issues, such as school avoidance, somatic complaints.
General—activity, appetite, affect, sleep patterns, weight changes, edema, fever, behavior.
Allergy—eczema, hay fever, asthma, hives, food or drug allergy, sinus disorders.
Skin—rash or eruption, nodules, pigmentation or texture change, sweating or dryness, infection, hair growth, itching.
Head—headache, head trauma, dizziness.
Eyes—visual acuity, corrective lenses, strabismus, lacrimation, discharge, itching, redness, photophobia.
Ears—auditory acuity, earaches (frequency, ages, response to specific medications), infection, drainage.
Nose—colds and runny nose (frequency), infection, drainage.
Teeth—hygiene practices, frequency of brushing, general condition, cavities, malocclusions.
Throat—sore throat, tonsillitis, difficulty swallowing.
Speech—peculiarity of or change in voice, hoarseness, clarity, enunciation, stuttering, development of articulation, vocabulary, use of sentences.
Respiratory—difficulty breathing, shortness of breath, chest pain, cough, wheezing, croup, pneumonia, tuberculosis or exposure.
Cardiovascular—cyanosis, fainting, exercise intolerance, palpitations, murmurs.
Hematologic—pallor, anemia, tendency to bruise or bleed.
Gastrointestinal—appetite (amount, frequency, cravings), nausea, vomiting, abdominal pain, abnormal size, bowel habits and nature of stools, parasites, encopresis (incontinence of feces), colic.
Genitourinary—age of toilet training, frequency of urination, straining, dysuria, hematuria (or unusual color or odor of infant’s soiled diaper), previous urinary tract infection, enuresis (age of onset; day or nighttime), urethral or vaginal discharge. Girls and young women: age at menarche, last menses, cramps, changes in interval and duration.
Musculoskeletal—deformities, fractures, sprains, joint pains or swelling, limited motion, abnormality of nails.
Neurologic—weakness or clumsiness, coordination, balance, gait, dominance, fatigability, tone, tremor, seizures or paroxysmal behavior, personality changes.
Establish the order of all data collection according to the needs of the patient. For example:
An exhausted parent with a screaming baby will not give a careful, comprehensive history.
Alternative care may not be available for preschoolers when the neonate comes in for his or her first checkup.
If the parent has come in with more than one child, try to organize some supervision of the other children so that you can have a little time alone with the parent.
Remember that the safest place for a young child is on the parent’s knee. Privacy may not be possible when other children are present.
Attempt to develop rapport with the young patient from the moment you first see or meet him or her.
Explain to the school-age child or teenager what you are looking for as you proceed with the examination and provide feedback.
Offer the young child a choice of being examined on the parent’s lap or on your “special table.”
To evaluate the chest properly, you need to listen through 10 heartbeats when the child is not screaming; therefore, the chest is a good place to begin the examination.
The part to be examined should be completely exposed, but if an apprehensive child objects to having clothes removed, slip your stethoscope under the shirt.
After listening to the heart, begin with parts of the body that are already exposed.
Start with either the head or the toes and work thoroughly and systematically toward the other end.
Gradually remove the child’s clothes (may best be done by usual caregiver); look for asymmetry very carefully in the bodies of all children.
Develop a pattern appropriate to the patient’s age.
With infants it may be wise to leave the diaper area until last.
Adolescents and school-age children are usually embarrassed at the genital examination—you may want to leave this until last.
Using a cold stethoscope may result in a frightened and screaming child, so warm the stethoscope before bringing it into contact with the child.
Some children are less frightened if allowed to hold the examination equipment first.
Show the child the procedure by demonstrating on the parent first.
Many young children enjoy listening to their own hearts.
Toddlers and preschoolers enjoy blowing your otoscope light out.
Pediatric Physical Assessment | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Pediatric Physical Assessment (continued) | |||||
|---|---|---|---|---|---|
| |||||