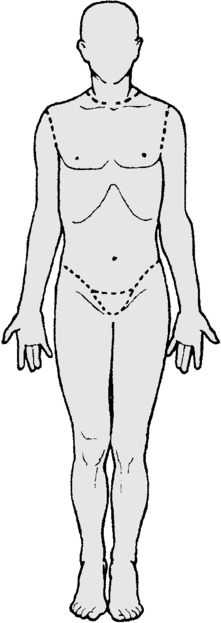
1. As you perform your initial assessment, you note superficial partial-thickness burns on A.N.’s right anterior leg, left anterior and posterior leg, and anterior torso. Shade the affected areas, then using the “rule of nines,” calculate the extent of A.N.’s burn injury. 2. Because you are concerned about possible smoke inhalation, what signs will you monitor A.N. for? 3. Interpret A.N.’s laboratory results. 4. A.N. is undergoing burn fluid resuscitation using the standard Baxter (Parkland) formula. She was admitted at 0400. She weighs 110 pounds. Calculate her fluid requirements, specify the fluids used in the Baxter (Parkland) formula, specify how much will be given, and indicate what time intervals will be used. 5. A.N. is in severe pain. What is the drug of choice for pain relief following burn injury, and how should it be given? 6. Because of her significant burn injury, A.N. is at high risk for infection. What measures will you institute to prevent this? 7. A.N.’s burns are to be treated by the open method with topical application of silver sulfadiazine (Silvadene). When caring for A.N., which interventions will you perform? (Select all that apply.) a. Maintain the room temperature at 85° F (29.4° C). b. Use clean technique when changing A.N.’s dressings. c. Monitor CBC frequently, particularly the white blood cells. d. Do not allow her to bathe for the initial 72 hours following injury. e. Apply a 8. A.N. has one area of circumferential burns on her right lower leg. What complication is she in danger of developing, and how will you monitor for it? 9. What interventions will facilitate maintaining A.N.’s peripheral tissue perfusion? 10. A special burn diet is ordered for A.N. She has always gained weight easily and is concerned about the size of the portions. What diet-related teaching will you provide? 11. Describe interventions that you could use to assist in meeting A.N.’s nutrition goals. 12. What do you suspect is occurring, and why does this concern you? 13. What treatment do you anticipate? 14. The physician orders a new set of lab work. Compare A.N.’s current lab results with those from admission. 15. Tissues under and around A.N.’s burns are severely swollen. She looks at you with tears in her eyes and asks, “Will they stay this way?” What is your answer? 16. A.N. is concerned about visible scars. What will you tell her to allay her fears? 1. Admitting has assigned J.L. to a semiprivate room. Her roommate is on day 4 of IV antibiotic treatment for pneumonia and now has a near normal WBC count. Is this assignment appropriate? 2. Fever is a sign of two major complications of organ transplantation. What are they? 3. What is the purpose of tacrolimus (Prograf), and what role does that play in your assessment? 4. Compare and contrast the signs and symptoms of organ rejection and sepsis that you need to assess for in J.L. 7. What other information do you need to know before you begin the vancomycin (Vancocin)? 8. What interventions do you need to implement to safely administer vancomycin? (Select all that apply.) a. Obtain a trough level 6 hours after each infusion b. Administer each infusion over a minimum of 1 hour c. Hold the infusion if J.L. complains of tinnitus d. Assess for the onset of hypertension during the infusion e. Monitor urine output, BUN, and creatinine levels
Patients with Multiple Disorders
Scenario
Case Study Progress
 -inch film of medication, covering entire burn.
-inch film of medication, covering entire burn.
Case Study Progress
Scenario
Case Study Progress
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Patients with Multiple Disorders
Get Clinical Tree app for offline access
