23. Patients requiring orthopaedic surgery
Nicola L. Whiteing
CHAPTER CONTENTS
Introduction 503
The musculoskeletal system 504
Common orthopaedic disorders 506
Nursing assessment of the orthopaedic patient 508
Orthopaedic investigations and tests 509
Lower limb orthopaedic surgery 510
Upper limb orthopaedic surgery 522
Orthopaedic surgery of the spine 525
Fractures 526
General discharge planning and advice 530
Conclusion 531
Introduction
There are two types of orthopaedic surgery: trauma (emergency) and elective surgery. Trauma surgery is carried out on patients who require urgent surgery, such as following an accident. Elective orthopaedic surgery is for patients waiting planned orthopaedic procedures such as joint replacements for progressive osteoarthritis.
At the end of this chapter the reader should be able to:
• describe the structure and function of the musculoskeletal system
• classify bones according to their structure
• classify joints according to their structure and degree of movement
• discuss specific orthopaedic investigations
• discuss common orthopaedic conditions
• discuss the importance of preassessment and education in preparing the orthopaedic patient for their surgery
• demonstrate knowledge of the nursing care of patients requiring surgery to the hip, knee, foot, shoulder, forearm, hand and spine
• discuss the process of bone healing
• discuss types of fracture and how they are managed
• discuss the relevance of neurovascular observations in detecting compromise and the actions to be taken if detected
• discuss specific issues in planning a patient’s discharge
• discuss the importance of patient education in rehabilitation.
One change that has affected orthopaedic nursing is the reduced time a patient now spends in hospital. Many patients now have surgery as a day case admission, instead of remaining in hospital overnight or for several days. Innovations such as preoperative assessment clinics and early discharge schemes, where patients are cared for in their own home earlier, also significantly reduce the length of time a patient spends in hospital.
In the context of change, orthopaedic nurses must continue to promote healing, maximize independence within the individual’s capability and promote optimal rehabilitation.
This chapter will describe some of the more common disorders of the musculoskeletal system that are caused by disease and trauma, and will explain orthopaedic surgical procedures and the relevant nursing care.
The musculoskeletal system
Most of the body’s mass is made up of the musculoskeletal system. It comprises bones, joints, ligaments, muscles and cartilage. The musculoskeletal system performs and enables several essential functions (Biswas and Iqbal, 1998, Judge, 2007a, Knight et al., 2005 and Tortora and Derrickson, 2006):
• the maintenance of body shape
• the support and protection of soft tissue structures such as internal organs
• movement
• breathing
• the manufacture of red blood cells, white blood cells and platelets in the bone marrow
• the storage and main supply of reserve phosphate and calcium in bone.
Bone
Bones are classified by their shape and fall into five categories.
• Long bones: these bones are greater in length than width. Pulled by contracting muscles, they act as levers for body movement. Long bones include the femur, tibia, fibula, radius, ulna and humerus.
• Short bones: these bones measure approximately the same in length and width, and are irregular in shape. They are found where only limited movement is necessary, such as the carpal and tarsal bones.
• Flat bones: these bones are generally curved or thin. They have a protective function and facilitate muscle attachment. Flat bones include the ribs, sternum, scapulae and bones of the cranium.
• Sesamoid bones: these small bones are found where tendons pass over the joint of a long bone. Their key role is protection, such as the patella bone of the knee joint.
• Irregular bones: these bones do not fit neatly in to any of the other categories. The facial bones and the vertebrae are examples of irregular bones.
Anatomy of a long bone
A typical long bone consists of the following parts.
• Diaphysis – the shaft or long part of the bone.
• Epiphysis – a proximal and distal epiphysis can be found at opposite ends of the bone.
• Metaphysis – separates the diaphysis from the epiphysis at either end of the bone. It is made up of the adjacent trabeculae of spongy bone.
• Medullary cavity – contains fatty yellow marrow and can be found within the diaphysis.
• Endosteum – the membrane that lines the internal cavities of bone.
• Articular cartilage – the layer of hyaline cartilage which covers the epiphysis and allows a joint to function more effectively by reducing friction.
• Periosteum – the fibrous membrane that covers the outer surface of bone that has not been covered by articular cartilage. It contains nerves, capillaries and lymphatic vessels and is essential for bone nutrition, growth and repair.
Bone tissue
Bone tissue comprises cells embedded in a matrix of ground substance, collagenous fibres and inorganic salts. The salts harden the bone, whereas the ground substance and collagenous fibres provide flexibility and strength.
Cancellous bone
• Cancellous bone consists of thin plates of bone tissue called trabeculae, and is also known as spongy bone because of its lattice-like appearance.
• Red marrow fills the spaces between the trabeculae, and within the trabeculae lie lacunae, which store osteocytes. The osteocytes are nourished through the marrow cavities from circulating blood.
• Cancellous bone stores some red and yellow marrow, and its main function is support.
Compact bone
• Compact bone is hard and contains cylinders of calcified bone known as osteons or Haversian systems. These systems are surrounded by calcified intercellular rings called lamellae.
• Centrally within the Haversian systems are Haversian canals, which contain nerves, blood vessels and lymphatic vessels. Haversian canals are longitudinal channels which generally branch into perforating canals called Volkmann’s canals. The Volkmann’s canals extend the vessels and nerves inward to the endosteum and outwards to the periosteum.
• Spaces called lacunae, which store osteocytes, can be found between the lamellae, and radiating from the lacunae are tiny canaliculi, which transport waste and nutrients into and out of blood vessels in the Haversian canals.
• Compact bone lies over cancellous bone and its main functions are support and protection.
Bone cells
Bone tissue contains four types of cell.
• Osteogenic cells – found in the periosteum, endosteum and the Haversian and Volkmann’s canals. They can be transformed into osteoblasts or osteoclasts during the healing process or at stressful times, e.g. following trauma.
• Osteoblasts – found in the growing parts of bones and the periosteum. They secrete some of the organic components and mineral salts involved in bone formation, and their main function is bone building.
• Osteocytes – the main cells of bone tissue. They derive from osteoblasts that have deposited bone tissue around themselves. Osteocytes keep the matrix healthy and help maintain homeostasis by assisting in the release of calcium into the blood.
• Osteoclasts – giant multinuclear cells found around bone surfaces, which do exactly the opposite of osteoblasts. Their main function is in resorption (dissolved and assimilated), which is essential in bone development, growth, maintenance and repair.
Bone ossification
Bones develop through a process known as ossification (osteogenesis). This process begins during the sixth week of embryonic life.
There are two types of ossification:
• intramembranous ossification, when bone is formed by mesenchymal tissue (embryonic connective tissue cells)
• endochondral ossification, when bone develops by replacing a cartilage model.
The primary ossification centre of a long bone is in the diaphysis. As a result of cartilage degeneration, cavities merge, forming the marrow cavity, and osteoblasts lay down bone. Ossification then occurs in the epiphyses but not for the epiphyseal plate.
Homeostasis
Bone assists homeostasis (a state of inner balance and stability) by the storage and release of minerals and calcium, as required in the blood and tissues to maintain appropriate levels. Normal bone growth depends on calcium and phosphorus, and adequate levels of vitamins A, C and D are essential for bone growth and maintenance.
Effects of hormones on bone
Bones have an effect on hormone secretion and several hormones have an effect on bones. The parathyroid hormone assists in osteoclast production, increasing bone remodelling, whereas calcitonin (a hormone released by the thyroid gland) reduces the calcium level in the blood and reduces bone resorption. Other hormones such as thyroxine, growth hormone, the sex hormones from the gonads and vitamins A, C and D are significantly involved in bone maturation, with thyroxine and the growth hormones stimulating endochondral ossification.
Effects of ageing on bone
The ageing process affects bone in two key ways.
1. The loss of calcium from bone starts in females at around 30 years of age and this loss increases as oestrogen levels decrease in the early 40s. By the age of 70, as much as 30% of the calcium in bone is lost; however, in the male, calcium loss does not generally start until over 60 years of age (Tortora and Grabowski, 2003).
2. There is a decrease in protein formation, which results in a decreased ability to produce the organic part of the bone matrix. This leads to osteoporotic bones in the elderly and an increased risk of fractures (Villareal et al, 2001).
Cartilage
Cartilage is a tough, avascular, flexible connective tissue which assists with the support systems of the body.
There are three types of cartilage.
• Hyaline cartilage is firm and smooth, and is found on the articulating surfaces of synovial joints.
• Fibrocartilage is tough, flexible and tension-resistant, and is found between the intervertebral discs.
• Elastic cartilage retains its strength while stretched, as it has more elastic fibres, and is found in the epiglottis and external ear.
Joints
A joint is the site at which two or more bones are united. A joint provides the mechanism that allows body movement. Based on the structure or type of tissue that connects the bones, joints are classified into three major groups: fibrous, cartilaginous and synovial.
Fibrous joints
The bones are united by fibrous connective tissue and allow very minimal movement, e.g. sutures between the bones of the skull.
Cartilaginous joints
The bones are united by a plate of hyaline cartilage (primary cartilaginous) or fibrocartilage (secondary cartilaginous), and will allow slight movement, e.g. the pubic symphysis or between the bodies of the vertebrae.
Synovial joints
Synovial joints contain a synovial (joint) cavity, articular capsule, synovial membrane and synovial fluid.
A synovial (joint) cavity is the space between two articulating bones. Articular cartilage covers the surfaces of the articulating bones but does not hold the bones together. Synovial joints are surrounded by an articular capsule, and the inner lining of the capsule is called the synovial membrane. The synovial membrane secretes synovial fluid to lubricate the joint and provides nourishment for the articular cartilage.
An extensive range of movement is possible with this type of joint. Based on the shape of the articulating surfaces and the range of movements possible, there are several different types of synovial joint: e.g. the ball and socket joint of the hip and shoulder, and the hinge joint of the knee.
Common orthopaedic disorders
Rheumatoid arthritis
Rheumatoid arthritis is the commonest chronic inflammatory disease of joints and affects 3% of women and 1% of men (Dandy and Edwards, 2003). The cause is unknown but the inflammation is the result of an abnormality of both cellular and humoral immunity with environmental and genetic factors involved (Coote and Haslam, 2004, Crawford Adams and Hamblen, 2001 and Dandy and Edwards, 2003). As it is a systemic disease, unlike osteoarthritis, rheumatoid arthritis affects structures all over the body.
Pathophysiology
The target for this disease is the synovium. In the early stages of the disease the synovial membrane is affected and the joints become warm, swollen and tender, and range of movement is reduced. This disease generally presents in the small peripheral joints, usually of the hands and feet (Dandy and Edwards, 2003), with the wrists and knees also being susceptible. Unlike osteoarthritis it nearly always affects several joints at the same time (Crawford Adams and Hamblen, 2001). The affected synovium contains plasma cells and lymphocytes, a reflection of the autoimmune nature of the disease, and, left untreated, the inflammatory reaction affects the neighbouring structures. As the disease progresses, there is joint cartilage, capsule and ligament destruction, leading to joint instability, subluxation and deformity (Solomon et al, 2001).
Although rheumatoid arthritis is mainly treated by rheumatologists, it does involve orthopaedic surgeons when conservative treatments have proved to be unsuccessful. Orthopaedic surgeons are involved when joints and ligaments require stabilization or reconstruction.
Osteoarthritis
Osteoarthritis is a degenerative ‘wear and tear’ process occurring in joints that are impaired by congenital defect, vascular insufficiency or previous disease or injury. It is by far the commonest variety of arthritis (Crawford Adams and Hamblen, 2001), affecting up to 85% of the population at some time in their lives (Coote and Haslam, 2004).
Osteoarthritis is defined as primary or secondary.
• Primary osteoarthritis has no obvious cause (Apley and Solomon, 2001), is most common in white females during their 50s and 60s and affects several joints (Dandy and Edwards, 2003).
• Secondary osteoarthritis has many causes and follows a demonstrable abnormality of which the commonest are obesity, malunited fractures, joint instability, genetic or developmental abnormalities, metabolic or endocrine disease, inflammatory diseases, osteonecrosis and neuropathies (Apley and Solomon, 2001, Crawford Adams and Hamblen, 2001, Dandy and Edwards, 2003 and McRae, 2006).
Pain, limited mobility and a decrease in functional ability are the main clinical features. X-ray or imaging is undertaken to confirm the diagnosis of osteoarthritis (Judge, 2007a and Temple, 2006).
Pathophysiology
In osteoarthritis the articular cartilage is slowly worn away, resulting in the exposure of underlying bone. The subchondral bone becomes hard and glossy (eburnated), and bone at the margins of the joint forms protruding ridges and spurs known as osteophytes. These spurs can break off, causing further restriction of movement and additional pain. It is the pain, stiffness and often deformity that force the patient to seek treatment.
Treatment of rheumatoid arthritis and osteoarthritis
Treatment can be conservative or operative. Orthopaedic surgery should not be recommended until all conservative measures have been considered.
Conservative treatment
• Weight reduction: if obese, the patient is encouraged to reduce weight, so that less weight is forced on to the joint. The patient needs to be informed of the problems caused by excess weight and understand that, by reducing their weight, they will assist in reducing their level of pain. This may be difficult for the patient, owing to the nature of the disease. It is therefore important to set small achievable targets and offer praise and encouragement as they achieve satisfactory weight loss.
• Physiotherapy: passive and active exercises can assist the range of joint movement, prevent contractures and improve coordination or balance. Heat therapy can often produce relief from pain.
• Hydrotherapy: the warmth and buoyancy of the water allows the patient active, pain-free movement and relieves muscle spasm.
• The use of a walking stick: the patient is encouraged to use the walking stick correctly, holding it in the opposite hand to the affected hip/knee.
• Aids and appliances: these can help the patient with activities of daily living: e.g. a helping hand to pick up dropped articles or an aid to assist with putting shoes and socks on.
• A shoe raise: application of a shoe raise to the shorter limb can correct the apparent shortening, relieving strain on the lumbar spine and opposite hip.
• Drug therapy: simple analgesics such as paracetamol or dihydrocodeine can be effective in reducing the pain caused by raw bone rubbing on bone; however, they are not useful in reducing the sinusitis of osteoarthritis. Non-steroidal anti-inflammatory drugs (NSAIDs) reduce the inflammatory response and many people find them useful before physical activity or at night. Disease-modifying anti-rheumatic drugs, corticosteroids and immunosuppressive drugs may be used for patients with rheumatoid arthritis.
• Intra-articular therapy: local injection of hydrocortisone into the joint may help to restore comfort and mobility.
Operative treatment
All patients need to be carefully assessed before a decision to undertake surgery is made, because some patients will benefit from surgery more than others, according to their physical, mental and social circumstances. Only when conservative treatments have failed, should operative treatment be considered.
The following criteria are often used to decide on the need for surgery:
• pain
• radiological changes
• joint stability
• loss of function
• immobility.
The most common surgical procedures for patients with osteoarthritis and rheumatoid arthritis are synovectomy, osteotomy, arthrodesis and arthroplasty.
• Synovectomy involves excision of diseased synovial membrane and is performed more frequently for the patient with rheumatoid arthritis.
• Osteotomy involves surgically cutting across the bone. It is used to correct bone deformity or to relieve joint pain.
• Arthrodesis is carried out to surgically fuse a joint. It is used to stabilize a joint, or for pain relief in a joint severely damaged or diseased.
• Arthroplasty is replacement of the joint by an artificial component and one of the most successful operations in orthopaedic surgery (Dandy and Edwards, 2003).
Nursing assessment of the orthopaedic patient
When assessing orthopaedic patients, it is important to first establish what their normal functional abilities were and then to see how their presenting complaint is decreasing this functional ability. A thorough nursing assessment is required to obtain essential information from patients about the physical, psychological, sociocultural, environmental and politico-economic factors affecting their activities of daily living and how they cope with these problems. Once the patients’ problems have been identified, the nurse can set goals, take nursing action and evaluate any subsequent care. The Roper, Logan and Tierney model of nursing (Roper et al, 1996) is one example of a model used in the nursing management of an orthopaedic patient and an example of this can be seen in Table 23.1.
| Assessment/usual routine | Patient’s problem | Goal | Nursing action | Evaluation |
|---|---|---|---|---|
| Maintaining a safe environment | ||||
| Uncemented hip prosthesis in correct position following anterior approach on return from operating theatre | Potential risk of dislocation of hip prosthesis | To prevent hip dislocation | Ensure Louise has a copy of the do’s and don’ts on how not to dislocate her hip Reinforce the information at regular intervals Place affected leg in a gutter splint Ensure Louise does not flex the hip to an angle of 90° or more Ensure Louise uses a high toilet seat on the ward and at home for 3 months | Louise’s hip prosthesis did not dislocate |
| Louise’s skin is healthy and intact | Potential wound infection or haematoma following surgery | To prevent wound infection and haematoma | Administer prophylactic antibiotics as prescribed Observe the wound for bleeding, swelling and excessive drainage Use aseptic technique when dealing with dressings and drains Record temperature ½–1 hourly initially, then 2–4 hourly for a 24 hour period | Louise remained apyrexial and the wound healed with no sign of infection |
Check drainage patency and maintenance of the vacuum drain every ¼ hour for 1 hour, then, if satisfactory, hourly for 24 hours Remove staples on the 10th postoperative day | The drain remained patent, the loss was minimal and the drain was removed 24 hours postoperatively | |||
| Potential risk of pressure ulcers as her mobility is reduced | To prevent pressure ulcers | Raise for pressure relief 2 hourly Encourage Louise to use the overhead bar on the bed Ensure her heels are kept free of the bed Use a gutter splint, ensuring heel is hanging over the edge Assess pressure ulcer risk using Waterlow score and use appropriate mattress if indicated Encourage mobilization on day 1 | Louise’s pressure areas remained intact | |
| Louise’s temperature was normal, 37.1°C, on admission to hospital | On return to the ward Louise’s temperature was 35°C | To assist body temperature back to normal limits | Place a Bair hugger next to Louise’s body and apply extra bed linen Record Louise’s temperature at regular intervals until it has returned to within normal limits | Within 2 hours Louise’s temperature had risen to 36.2°C and the Bair hugger was removed Louise’s temperature remained above 36.2°C and below 37.5°C |
| Mobilization | ||||
| Louise’s mobilization and distance she could walk without pain prior to surgery was approximately 300 yards | Postoperatively, Louise had lack of confidence mobilizing, but her pain was under control | Louise to regain confidence mobilizing | Give explanations and reassurance prior to and when mobilizing Observe for signs of dislocation On day 1 begin mobilizing Louise with the aid of a physiotherapist, starting with transfers from bed to chair, learning the correct way to sit in a chair and progressing on to how to use the sticks safely to avoid dislocation Louise will need to mobilize partial weight-bearing on the operated leg for 6 weeks | Louise can safely mobilize and transfer from bed to chair and bed to toilet with confidence |
| Work and play | ||||
Louise works as a part-time secretary for a small local firm The firm is having some financial problems and there have been some redundancies | Louise is warned she may lose her job due to her sick leave She likes to get out and does not wish to retire | To return to work as soon as she is able | Encourage Louise to express her fears Refer to a social worker | The surgeon wrote a supportive letter to her employer, who was very sympathetic and supportive |
| Louise is a keen gardener | Louise is concerned that she will not be able to return to her hobby of gardening, although she admits that she has been unable to do any gardening during the 6 months prior to surgery | For Louise to return to light gardening activities | Refer Louise to the physiotherapist for advice on safe movement while gardening | As yet, Louise has not returned to gardening but looks forward to doing so She has learnt what she can do safely and accepts this |
| Expressing sexuality | ||||
| Louise and her husband have been married for 32 years and still enjoy a sexual relationship. This has been affected by pain in recent months, and Louise confided that her husband had offered to sleep in the spare room to give her more room and to prevent her dislocating her hip when she got home | Fear of dislocating hip during sexual relations | Louise to return to sexual relations with her husband without dislocating her hip | Give Louise advice and reassurance that she can resume sexual intercourse in the passive role at approximately 6 weeks Give Louise details of the association to aid the sexual and personal relationships of people with a disability (SPOD) and provide a leaflet on positions postoperatively | Louise has yet to resume sexual intercourse but feels she knows how not to dislocate the hip |
Every patient is a unique individual and the nursing assessment should be tailored to address these individual needs. The following points, however, are often discussed and assessed in an orthopaedic nursing assessment (Judge, 2004).
• Mobility
– Is movement restricted, and, if so, how restricted is the movement?
– Is the range of movement limited?
– Is active range of movement less than passive?
– Does mobility improve throughout the day?
– What is the condition of the patient’s musculoskeletal system?
– What is the neurological status of the affected limb?
– Does the patient require aids to assist mobility?
• Pain
– Where is the maximal site of pain?
– Does the pain radiate away from the site of injury?
– Does the pain change during the course of the day?
– How would the pain be described?
– Is there swelling or deformity?
• Sleep
– Is sleep affected by pain?
• Sexuality
– Has a limp, limb-shortening or a deformity altered the patient’s body image?
– Has the patient had surgery that is affecting their sexual relationship?
• Mental state
– Is the patient anxious or depressed?
– Does the patient suffer from dementia or poor attention span?
• Breathing
– Does the patient smoke?
– Does the patient have a history of cardiovascular problems?
– Does the patient have any sort of curvature of the spine that is affecting their respiratory system?
• Working and playing
– Has the problem affected the patient’s work and/or social activities?
– Does the patient require assistance for household activities?
The main aim of the orthopaedic nursing assessment and subsequent care that is planned is to assist the patient to be as independent as is realistically possible.
Orthopaedic investigations and tests
Standard X-rays
Standard X-rays assist in the diagnosis and confirmation of the injury or disease, e.g. fractures, loss of joint space in osteoarthritis. Usually, no specific preparation is required.
Computerized axial tomography
A computerized axial tomography (CAT or CT) scan combines X-rays with computer technology to show cross-sectional views (tomograms) of internal body structures. The patient is intravenously injected with a low-level radioactive tracer and lies on a table slowly passing through a circular tunnel in the scanner, where rotation of a low-intensity X-ray beam across the width of the body takes place. Detectors opposite the X-ray beam record the degree to which the X-ray is absorbed by various body tissues and convert the modified beams into electronic signals that are fed into the computer. Changes in the X-ray beams are then analysed by the computer, and high-resolution images are shown on a monitor. These images are kept on film and examined one section at a time. This investigation is particularly useful in the diagnosis of spinal and skull disorders.
Magnetic resonance imaging
Magnetic resonance imaging (MRI) is a non-invasive investigation of the body’s deep structures. The patient is required to lie on a non-magnetic stretcher and is passed into a scanner where the body is exposed to a strong magnetic field. This magnetic field causes the body’s protons to line upright in rows parallel to the field. The patient’s body is then exposed to radiofrequency waves, which cause the protons to fall out of line. When the radiofrequency waves are stopped, the protons return to their previous position. Images of this movement are taken and visually displaced. MRI is particularly useful to show changes in the vascularity of bone following trauma, and degenerative changes in the ligaments and intervertebral discs (Dandy and Edwards, 2003).
Many patients who undergo an MRI scan experience anxiety or panic attacks and nurses should therefore help reduce stress by maintaining verbal contact.
Thermography
Thermograms create a pictorial representation of warm areas around a joint, which provides an indication of the blood supply and areas of inflammation or vascular disease (Dandy and Edwards, 2003). They are particularly useful to assess the progress of rheumatoid arthritis and its response to treatment.
Radioisotope bone scan
The patient is given an intravenous injection of radioisotope substance, which is taken up in the bone. The amount of uptake reflects the bone turnover and is of value in the early detection of tumour invasion, bone death and repair.
Bone densitometry
This technique is carried out to measure bone mineral density in patients with metabolic bone disease and may be required for the whole of the patient’s body or an identified area. This measurement assists the clinician to make an informed opinion on the most appropriate treatment for the patient.
Arthroscopy
Arthroscopy is an invasive procedure which involves the introduction of an instrument called an arthroscope into a joint, under local or general anaesthetic. Arthroscopy enables inspection of the interior of the joint with and without joint movement and allows manipulation of individual structures with a probe or hook.
Lower limb orthopaedic surgery
The hip
Total hip replacement (arthroplasty)
Total hip replacement (arthroplasty) is the most popular operation for osteoarthritis of the hip (Dandy and Edwards, 2003). In a total hip replacement, the worn acetabulum and femoral head are removed and replaced with artificial components, which can be either cemented or uncemented (Fig. 23.1).
• Cemented: this involves the use of a dense cup, usually polyethylene, and a metal or metal alloy femoral component. Each of these parts is secured by the compound methylmethacrylate, which has properties resembling bone. A disadvantage of the cemented prostheses is the potential bone destruction caused if the prosthesis becomes loose.
• Uncemented: where cement would have been placed, more cortical bone is preserved. This allows younger patients to have total hip replacement surgery with increased choice for revision surgery in the future.
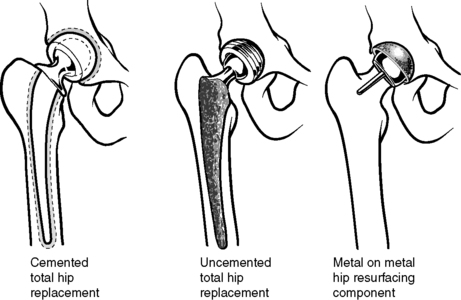 |
| Figure 23.1 • Total hip arthroplasty. (From Dandy and Edwards, 2003, with permission.) |
Metal on metal hip resurfacing
Over the last 10 years, hip resurfacing has gained popularity as an alternative to a total hip replacement in younger, active patients with joint disease (Adams and Quigley, 2005). The resurfacing component does not use a long stem, and both the femoral and the acetabular components are metal, which decreases the amount of wear debris within the hip capsule (Dandy and Edwards, 2003).
Minimally invasive hip replacement
Minimally invasive hip (MIH) surgery involves the insertion of the prostheses via one or two incisions, each less than 10 cm, compared with a traditional incision of 20–30 cm (Lucas, 2006). While appealing to patients, when MIH is compared with traditional-incision total hip replacement surgery there is yet a lack of large-scale long-term robust clinical trials on its success (Lucas, 2006).
Preoperative assessment and care
It is recommended that patients undergoing total hip replacement attend the preoperative assessment clinic and education classes 2–3 weeks prior to surgery.
Preoperative assessment enables the multidisciplinary team to ensure that the patient is as medically fit as is possible, in order that they are not cancelled because of medical problems when admitted to hospital. This allows effective use of resources such as theatre time and hospital beds and avoids patient disappointment when their surgery is cancelled (Oakley, 2005 and Smith and Rudd, 1998).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access

