10. Patients requiring neurosurgery
Christine Eberhardie
CHAPTER CONTENTS
Overview of the anatomy and physiology of the nervous system137
Specialist investigations139
Neurosurgery141
Preoperative assessment of the patient undergoing cerebral surgery142
Planning care for the neurosurgical patient148
The principles of postoperative care of a patient following a craniotomy158
Conclusion160
At the end of the chapter the reader should be able to:
• give a brief overview of the anatomy and physiology of the central nervous system
• discuss the specialist investigations the patient may undergo
• describe the reasons for carrying out neurosurgery
• discuss the mechanisms and consequences of raised intracranial pressure and its treatment
• discuss the need to undertake a detailed neurological assessment of patients
• describe in detail the holistic nursing care of a patient undergoing a craniotomy
• develop an increased awareness of the long-term consequences of neurosurgery and the need for the patient, carer and society to be well informed.
Introduction
The specialty of neurosurgery involves surgery to the brain and spinal cord. There is, however, an overlap between all the head and neck disciplines. For example, in severe traumatic brain injury, neurosurgeons, ophthalmic, maxillofacial and dental surgeons frequently work together to reconstruct damaged tissues; vascular surgeons have also developed a technique for removing atheromatous tissue from the carotid arteries supplying the brain, called carotid endarterectomy; and spinal surgery is carried out by orthopaedic surgeons too.
Surgery to the brain and spinal cord can be life saving but it can leave the patient with serious disability. Part of the initial care is carried out in intensive care/high dependency units, and some patients will be treated in specialist neurosurgical units and then transferred back to a general hospital.
An increasing number of interventions which were once dealt with by neurosurgery are now carried out by neuro-radiologists; for instance, detachable coil embolization.
Overview of the anatomy and physiology of the nervous system
The skull
The brain is protected by the rigid bony structure of the skull or cranium. The brain, its blood supply and a regulated amount of cerebrospinal fluid fill the cranium and are usually referred to as the intracranial contents (see Box 10.1 and section on raised intracranial pressure, p. 142).
 Box 10.1
Box 10.1 Intracranial contents (% volume)
Brain 80%
Blood 10%
Cerebrospinal fluid 10%
The brain
The brain consists of the cerebrum and the cerebellum, which are separated by a double fold of dura mater known as the tentorium. The area above the tentorium is known as the supratentorial space, and the area below it is the infratentorial space.
The cerebrum is further divided into two cerebral hemispheres by the falx cerebri, which is a double fold of dura mater with a venous sinus, the superior sagittal sinus, in between the two layers of dura mater. The two hemispheres are joined by the corpus callosum. The cerebral cortex, which makes up the outer layer of the brain, comprises neural cell bodies (grey matter). This layer of grey matter plays a most important role in the higher functions of the brain. The cerebral cortex of each hemisphere has four lobes which are not separated physically and are named after the bones that lie above them: i.e. frontal, parietal, temporal and occipital.
The nerve fibres carrying sensory and motor information to and from the cortex and other islands of grey matter, such as the basal ganglia, are known as white matter. The white appearance is caused by the presence of myelin surrounding the neural axons making up the fibres. The myelin provides a protective insulating sheath around the axon.
The meninges and cerebrospinal pathways
The brain and spinal cord are covered by the meninges, which are made up of an outer tough layer called the dura mater; a middle layer, the arachnoid mater; and a layer which lies next to the brain and spinal cord, called the pia mater. The arachnoid mater is so-called because its cells have a spider-like appearance. Between the arachnoid mater and pia mater lies the subarachnoid space. The arteries of the brain, known as the circle of Willis, lie in the subarachnoid space of the brain, and cerebrospinal fluid circulates around the brain in the subarachnoid space. It is formed in the choroid plexus in all four ventricles. From the lateral ventricles it flows through the interventricular foramina (foramina of Monro) to the third ventricle. From there it flows through the central aqueduct to the fourth ventricle. The cerebrospinal fluid flows from the fourth ventricle into the subarachnoid space via the foramen of Magendie and the foramina of Luschka. There are also large collections of cerebrospinal fluid to be found in the cisterna magna at the base of the brain.
Cerebrospinal fluid
Cerebrospinal fluid consists of water, glucose, protein and electrolytes. It protects and nourishes the brain, by absorbing a certain amount of shock, bringing nutrients such as glucose to the cells and providing some immunity to infection.
Basal ganglia and thalamus
The basal ganglia are masses of grey matter deep in the brain and contain the putamen, caudate nucleus, globus pallidus, subthalamic nucleus and substantia nigra. They are interconnected with the thalamus. The function of the basal ganglia is to coordinate voluntary muscle movement and to maintain the tone of the muscles. Disorders of the basal ganglia result in movement disorders such as chorea, athetosis, hemiballismus, and the increased tone and tremor seen in Parkinson’s disease.
The hypothalamus
The hypothalamus lies above the pituitary gland and is connected by the pituitary stalk. This area of the brain controls the autonomic nervous system and has links with the limbic system and the pituitary gland. The limbic system is a network of interlinking pathways which are responsible for the emotions, motivation and behaviour. This activity results in the monitoring and control of temperature, appetite and satiety; water regulation and thirst; physical experiences of emotion such as fear, pain, pleasure and rage; and the control of the neuroendocrine system by the production of releasing factors.
The pituitary gland
The pituitary gland consists of two parts. One is the neurohypophysis (posterior pituitary gland), which receives hormones secreted by the hypothalamus and releases them into the capillary blood supply. The two hormones secreted by the neurohypophysis are antidiuretic hormone and oxytocin by way of the hypothalamo-hypophyseal tract. The other part of the pituitary gland is the adenohypophysis (anterior pituitary gland), which synthesizes and releases hormones into the blood when stimulated by the hypothalamic releasing factors.
The cerebellum
The cerebellum lies in the posterior fossa. It is made up of two hemispheres separated from the cerebrum above by the tentorium, i.e. a tent-shaped fold of dura mater. Each hemisphere is separated by the vermis. The function of the cerebellum is to coordinate muscle movement and to maintain posture and balance.
The brainstem
The brainstem consists of the midbrain, pons varolii and medulla oblongata. The midbrain is the part of the brainstem nearest to the hypothalamus. The pons varolii lies between the midbrain above and the medulla oblongata below. The medulla oblongata has an oblong shape and extends to form the spinal cord.
One function of the brainstem is to control sleeping and waking. It monitors the environment during sleep in order to arouse the sleeper when necessary. Essential motor and sensory fibres pass through the brainstem, to and from the cerebral cortex. Without such information the body cannot become aware of its surroundings. It contains many of the body’s vital centres such as the cardiac, respiratory and vomiting centres, and is also the source of most of the cranial nerves which play a role in specialized sensory input such as hearing, balance and taste, as well as motor functions such as chewing, swallowing and shrugging the shoulders.
The blood supply to the brain
The arterial supply to the brain is known as the circle of Willis, which is supplied by the carotid arteries. The circle provides a collateral supply to the whole brain. If any one of the arteries is compromised, the others can take over the supply.
Specialist investigations
A number of specific investigations may be undertaken as part of the clinical investigations of a patient (Box 10.2).
 Box 10.2
Box 10.2 Specialist investigations
Magnetic resonance imaging
Angiography
Electroencephalography
Video telemetry
Lumbar puncture
Skull X-rays
Computerized axial tomography
Positron emission tomography
Digital subtraction angiography
Magnetic resonance angiography
Cortical mapping
Sensory evoked potentials
Myelography
Transcranial Doppler
Computerized axial tomography
Computerized axial tomography (CT) is an X-ray technique which enables the brain to be X-rayed in the coronal or sagittal planes in a series of slices 2–10 mm wide. The computer then processes the information, and the end result is a series of films showing the structure of the brain or spine at various levels. It depicts the structures of the brain and spinal cord at the time the scan was taken, but it cannot demonstrate physiological activity over a period of time.
Positron emission tomography
Positron emission tomography (PET) scanning is a relatively new technique which has been developed in order to demonstrate the functional activity of the brain over a period of time (anything from 20 minutes to 2 hours, depending on the substance used). It involves the production of isotopes that emit positrons, which are then used to label substances which the target organ needs. In the case of the brain, oxygen and glucose are labelled. The resulting scan shows areas of increased local uptake and activity (McCulloch, 1986). It has been used in the study of dementia, schizophrenia and many other neurological and psychiatric disorders; however, it is not used in routine clinical investigations.
Angiography
Cerebral angiography is useful when it is necessary to demonstrate the state of cerebral arteries and diagnose abnormalities of the blood vessels, such as atheroma, aneurysms and arteriovenous malformations. It is also helpful in the diagnosis of brain tumours, and it is used in the newly developing techniques of embolization of vessels in the treatment of aneurysms.
Digital subtraction angiography (CT angiography)
Digital subtraction angiography is a combination of angiography and computer technology in which the computer can subtract information from the image and expose the vessels of interest more clearly.
Magnetic resonance angiography (MR angiography)
Magnetic resonance angiography is used to evaluate blood vessels and detect abnormalities of the lumen of blood vessels (Clifton, 2000).
Electroencephalogram
An electroencephalogram (EEG) is a recording of the electrical activity of the brain and is used in the diagnosis of various neurological conditions, especially epilepsy. It is also useful in the investigation of sleep disorders.
Cortical mapping
Cortical mapping is carried out during awake craniotomies for patients suffering from lesions that are near vital areas such as the speech and language areas. In this way, patients can tell the surgeon what they are experiencing and enable the surgeon to be more precise and selective in the amount of tissue that is removed (Reinhardt et al, 1996).
Video telemetry
Video telemetry is a form of electroencephalography which is linked to a video camera. Patients suffering from epileptic or non-epileptic seizures have video telemetry to enable the medical staff to see clearly the clinical manifestations of the seizure and have the EEG recording during it.
Sensory evoked potentials
Some diagnoses can be made by stimulating specific sensory pathways and recording the electrical activity of the appropriate area of cerebral cortex and/or brainstem. Visual evoked potentials are useful in the diagnosis of multiple sclerosis. Auditory evoked potentials are useful in the diagnosis of acoustic neuroma and brainstem death.
Lumbar puncture
Lumbar puncture is a procedure carried out by a doctor, during which a spinal needle is inserted into the subarachnoid space between the third and fourth lumbar vertebrae. Cerebrospinal fluid is withdrawn for the following reasons:
• to confirm a diagnosis, e.g. meningitis
• to instil dyes, e.g. as in myelography; or drugs, e.g. intrathecal antibiotics.
It should not be used in patients with raised intracranial pressure, as it can provoke tentorial herniation (see p. 143).
Myelography
A myelogram is a specialized X-ray of the spine. A water-soluble dye is inserted into the subarachnoid space through a lumbar puncture, and lesions of the spine are highlighted if the cerebrospinal fluid pathway around the spinal cord is impeded in any way by a disc protrusion, tumour or arteriovenous malformation.
Skull X-ray
Anterior–posterior and lateral radiographs of the skull are usually taken in order to diagnose skull fractures, meningiomas and other bony injuries of the skull. In cases of head injury, the radiograph should include the neck down to and including the seventh and eighth cervical vertebrae, to exclude cervical fracture/dislocation.
Transcranial Doppler
Transcranial Doppler studies rely on ultrasound technology. A very low frequency ultrasound wave is passed through the skull and is useful in assessing cerebral blood flow and vasospasm in disorders such as carotid stenosis.
Neurosurgery
Reasons for neurosurgery
Neurosurgery is performed for two reasons:
• the removal or repair of brain tissue in order to prevent further harm
• to give palliative relief of distressing symptoms when the cause cannot be removed.
Box 10.3 gives a brief résumé of the reasons for neurosurgery.
 Box 10.3
Box 10.3 Reasons for neurosurgery
• Trauma: e.g. fractured skull, spinal injuries, traumatic brain injury
• Infections: e.g. cerebral and spinal abscesses
• Vascular disorders: e.g. cerebral aneurysm, haematoma, arteriovenous malformation
• Spinal disorders: e.g. tumours of the spine, prolapsed intervertebral disc
• Congenital abnormalities: e.g. hydrocephalus, craniostenosis
• Cerebral and spinal tumours: e.g. glioma, meningioma
• Degenerative disorders: e.g. carpal tunnel syndrome, arthritic changes in the spine
The approaches used by the surgeon
Burr holes
Burr holes are holes drilled into the skull with an air drill and are used for:
• insertion of brain needles to remove tissue for biopsy, or removal of a subdural haematoma
• to insert Gigli’s saw to create a bone flap in a craniotomy.
Craniotomy
A craniotomy is an opening of the cranium, as shown in Figure 10.1. It is performed when a surgeon requires direct access to a cerebral hemisphere. At the end of the operation, the bone flap is usually replaced. Pioneering surgery is being carried out in the treatment of brain tumours and epilepsy. The patient is woken after the skull is opened, so that by assessing the patient while mapping the cortex and dissecting the tumour the surgeon can remove more of the tumour than ever before (Sarang and Dinsmore, 2003). The patient is anaesthetized again during the closure of the skull. This procedure is also used in some forms of epilepsy surgery.
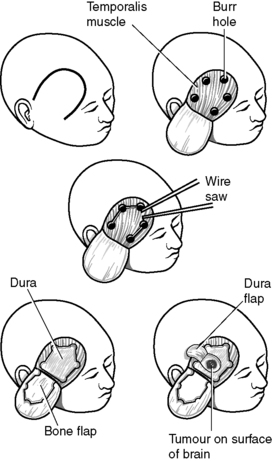 |
| Figure 10.1 • Stages of a craniotomy. (From Purchese 1977, with permission.) |
Craniectomy
A craniectomy is also an opening into the cranium, but it is smaller and the bone is usually chipped away and not replaced. This is commonly used in posterior fossa surgery.
Hypophysectomy
Hypophysectomy is the name of the operation for the removal of pituitary (hypophysis) tumours. This surgery can be done by a transsphenoidal approach through the nose, or transoral approach through the mouth, or through a craniotomy (see Fig. 10.1).
Laminectomy
Laminectomy is the term used for surgery of the spine in which the laminae have been opened to gain access to more than one level of the spinal cord.
Microdiscectomy
Microdiscectomy is a technique used increasingly by neurosurgeons to remove prolapsed intervertebral discs with the minimum of surgery. There is no bony involvement, and patients can be mobilized within 48 hours.
The long-term consequences of neurosurgery
The rehabilitative process begins with the nurse’s preoperative assessment and care planning. The prevention of common perioperative and postoperative complications is shared with the other disciplines discussed in this book, e.g. wound infection, deep vein thrombosis, haemorrhage and anaesthetic complications. The consequences of raised intracranial pressure (RICP) or ischaemia need to be considered, as outlined later in this chapter.
In addition, however, the results of focal damage to a particular area of the brain must be considered. As we will see with John, who underwent partial removal of a frontoparietal glioma, there were focal problems that resulted from removal of part of the frontal and parietal lobes.
Preoperative assessment of the patient undergoing cerebral surgery
A detailed history, functional and neurological assessment/observations can assist the nurse and other members of the critical care team to plan and monitor care. In neurosurgery, a patient’s condition can deteriorate very quickly, with fatal consequences. One of the important skills of the neuroscience nurse is the ability to make detailed observations and act upon them promptly. The main cause of rapid deterioration in neurosurgery is raised intracranial pressure.
Raised intracranial pressure
The adult brain is protected by a closed skull. The only openings in the skull are the foramen magnum, the small foramina by which the cranial nerves enter or leave the skull, e.g. optic or auditory nerves, and the sinuses. The contents of the skull are such that there is little room for anything that takes up extra space. The normal intracranial pressure (ICP) is 0–10 mmHg. However, a higher upper limit of 15 mmHg is the more usual level recognized in neurosurgical practice (Garner and Amin, 2007). This margin of 0–15 mmHg enables such activities as coughing, straining and bending to take place without the individual being harmed. If there is a space-occupying lesion in the brain, such as a haematoma, hydrocephalus or a tumour, the brain will compensate until it reaches a point where it cannot do so any longer. This period of autoregulation is known as Cushing’s response, and during this phase the autonomic nervous system responds by slowing the pulse rate and widening the systolic and diastolic blood pressure. This is nature’s attempt to overcome the pressure on the cerebral arteries and ensure cerebral blood flow. If the lesion is supratentorial, the pressure above the tentorium will be greater than that below.
In this way the pressure is funnelled toward the weakest point in the tentorium, causing tentorial herniation of the uncus of the temporal lobe. This funnel-shaped pressure wave is like an ice cream cone and gives rise to the term ‘coning’. At this point there is pressure on the brainstem and the third cranial nerve (oculomotor nerve) on the affected side. This results in a change in the size and reaction of the pupil to light on the same side as the lesion.
If left untreated, the third cranial nerve on the other side becomes compromised and both pupils will become dilated and eventually cease to react to light. A Cheyne–Stokes respiratory pattern will follow, and the continuing pressure on the brainstem will disrupt the stability of the blood pressure and pulse rate, and death will follow. Neurological assessment and observations are essential to detect early signs of rising intracranial pressure and to treat them. The first sign of rising intracranial pressure may be headaches, lethargy or increased drowsiness, depending on the speed at which the intracranial pressure is increasing. Nursing measures to treat raised intracranial pressure will be discussed in the section on postoperative care.
The neurological assessment and observations
The major difference between neurological assessment and neurological observations is that a neurological assessment is more holistic and covers all the nervous system activity, including cognition, perception and behaviour, when it is possible to assess these aspects of the patient. It also includes neurological observations.
A full neurological assessment is taken on admission to the neurosurgical ward and will provide a baseline for planning care. A further full assessment needs to be carried out at regular intervals during the patient’s stay in the unit, in order to fully evaluate care and to plan for the patient’s discharge or transfer to a general hospital.
The nurse should look closely at the findings made by the doctor in their history and clinical examination at the time of admission, in order to compare the patient’s perception of their problems with the nurse’s own findings. Sometimes, patients and their carers give information to nurses because they believe the information to be of little importance to the doctor, or because they forgot to mention it, or may have been too embarrassed or frightened to talk about it.
An assessment of neurological function should include the following:
• conscious level, by using the Glasgow Coma Scale (Teasdale and Jennett, 1974)
• vital signs – temperature, pulse, respirations and blood pressure
• posture and gait (if able to walk)
• signs of infection
• pressure ulcer risk assessment (Waterlow, 1985)
• behaviour
• perceptual problems
• pain
• vision
• sensory pathways
• cognitive function
• communication
• use of drugs, e.g. alcohol, over-the-counter drugs, prescribed and illegal drugs
• urinary continence (Woodward, 1995).
Conscious level by using the Glasgow Coma Scale
Teasdale and Jennett (1974) developed the Glasgow Coma Scale, which is a simple scale for measuring the patient’s level of arousal and awareness, and, by so doing, enabling clinicians to determine the patient’s progress by means of a reliable and valid tool. It has since been brought into use by most neurosurgical units throughout the world, although it has been modified. There are three parts to the Glasgow Coma Scale: eye opening, best motor function in the arms and best verbal response. Each of the items on the scale is given a score. The sum of all the scores gives a maximum of 15 and the lowest possible score is 3. Figure 10.2 shows a chart for recording scores on the scale.
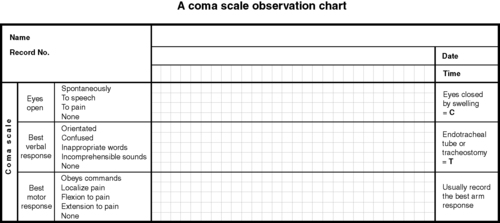 |
| Figure 10.2 • A coma scale observation chart. (From Montague et al, 2005: 124.) |
Many neurosurgeons do not use the total score as a reliable guide to the patient’s state but tend to note the scores for each of the three modalities separately. The advantage of the Glasgow Coma Scale over any other is that it has been shown to have good interobserver reliability (Juarez and Lyons, 1995) among trained, experienced staff (Fairley and Cosgrove, 1999). The Glasgow Coma Scale cannot be used in isolation. When used with the other observations such as vital signs, speech and language, and cognitive and perceptual behaviours, the nurse obtains a more complete assessment of the patient’s neurological state. The frequency of these recordings will depend on the severity of the patient’s condition and the likelihood of sudden deterioration, e.g. following a craniotomy when the patient may suffer from a haemorrhage or cerebral oedema.
Vital signs: temperature, pulse, respirations and blood pressure
The patient’s temperature, pulse, respirations and blood pressure should be recorded regularly. In raised intracranial pressure, the patient’s temperature is likely to rise as pressure on the hypothalamus and brainstem increase. Having excluded infection, the patient should be kept cool by modifying the temperature of the room and by removing all but enough clothing to preserve the patient’s dignity. Drugs such as paracetamol may be required to keep the temperature under control. Fanning is not used as it can induce shivering, which increases the metabolic rate. This is undesirable in the hypermetabolic postoperative patient and also increases the risk of hospital-acquired infections (Iggulden, 2006).
The nurse should observe not only the rate and quality of the pulse but also its rhythm. In raised intracranial pressure, the pulse will be strong and bounding. After subarachnoid haemorrhage, the pulse is often irregular because of disturbances of the catecholamines (Kocan, 1988).
Respiration needs to be monitored very closely as neurosurgical patients are more likely to undergo a respiratory rather than a cardiac arrest. In raised intracranial pressure, respiratory function is compromised when the pressure is so great that tentorial herniation occurs, causing torsion and pressure on the brainstem, which in turn causes pressure on the respiratory centre. The problem is not only mechanical but also biochemical. The increased pressure inside the skull causes the cerebral perfusion pressure to fall. This results in tissue hypoxia, and the level of carbon dioxide rises, which in turn leads to vasodilatation and a further increase in intracranial pressure (Fig. 10.3).
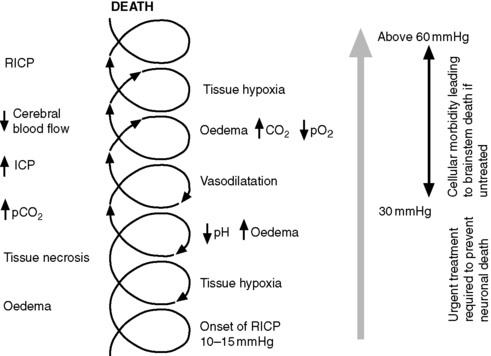 |
| Figure 10.3 • Untreated raised intracranial pressure (RICP) and its consequences. |
It is therefore important to monitor the patient’s oxygen saturation levels. In intensive care units this is done by frequent arterial blood gas analysis to observe more accurately the patient’s arterial oxygen, carbon dioxide and sodium bicarbonate levels, as well as monitoring any acidosis or alkalosis that may be developing (Brenner and Welliver, 1990). In other wards and departments, extra vigilance is required to ensure that the patient’s mucous membranes are pink and well perfused. Pulse oximetry can be used to measure oxygen saturation if arterial blood gas monitoring is not possible (Tremper and Barker, 1989).
Blood pressure monitoring provides another good indicator of raised intracranial pressure because, as the Cushing’s response takes effect, the gap between the systolic and diastolic pressure widens and the systolic pressure rises significantly, as shown in Figure 10.4. In subarachnoid haemorrhage, the blood pressure should be maintained at a constant high level, since rapid rises or falls can provoke rebleeding or vasospasm (Mestecky, 2005 and Rusy, 1996).
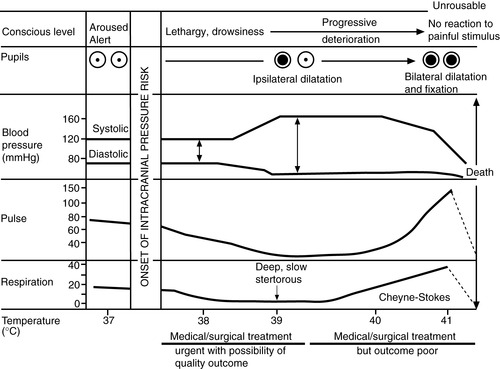 |
| Figure 10.4 • Chart showing progress of raised intracranial pressure. |
Mobility, posture and gait
The patient’s ability to walk should be examined unless their condition precludes it. Among the group of patients on whom one would not be able to carry this out are those who have had a severe traumatic brain injury, a brain haemorrhage or where the level of consciousness is impaired. It is necessary to establish how far the patient can walk and whether walking aids or assistance is required. The patient should walk down the ward, with help if needed, and their posture and gait observed. Patients with ataxia tend to fall backwards or to one side. Those with lower motor neuron lesions may walk with a drop foot and have signs of increased wear on the toes of their shoes on the affected side. If there are perceptual problems, the patient may appear clumsy and knock into objects, and may also be labelled confused. When proprioception is lost, the patient may walk with a high-stepping gait and will tend to fall if in a darkened room.
Nutritional status
It is important to assess the nutritional status of the patient on admission. Height, weight and body mass index should be recorded, along with brief details of appetite, eating habits and food preferences, intolerance or allergies. A physical examination will identify any problems with dentition, mobility, chewing and swallowing. A social history will help to identify problems such as distance from the shops for those who have mobility problems, as well as issues related to safety and competence to prepare and cook food.
Nutritional assessment is a team activity and the nurse’s role is to ensure that the appropriate members of the nutrition team, i.e. dietitian, speech and language therapist, occupational therapist, social worker, pharmacist and doctor – are informed of any problems.
Neurosurgery causes a massive stress response, which results in hypermetabolism, hypercatabolism and glucose intolerance. Cortisol levels rise and the patient will start to break down muscle, develop ketosis and lose weight rapidly (Mestecky, 2006 and Ott and Young, 1991). To try to prevent this from happening, the patient should be fed a well-balanced diet high in protein as soon as possible after admission, and starved preoperatively for as short a time as is compatible with safe anaesthesia. Commercially prepared feeds can also be prescribed. They contain all the essential amino acids required to enable neurotransmitters to be formed and to prevent the breakdown of muscle. They usually contain 1–1.5 kcal/mL of feed, which enables the nurse to feed the patient adequately even when there is raised intracranial pressure, and an optimal fluid intake is important in neurosurgical care (Cook, 2005).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access

