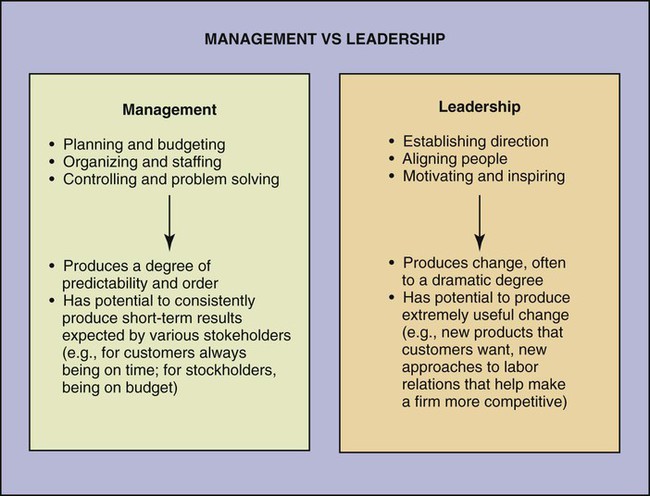
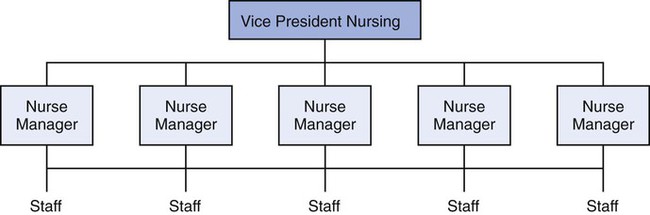
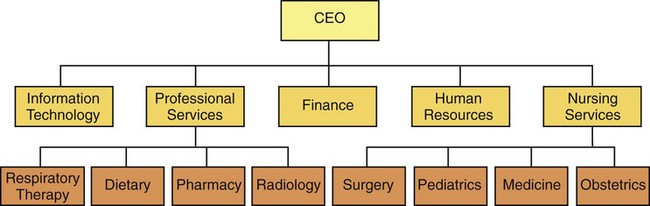
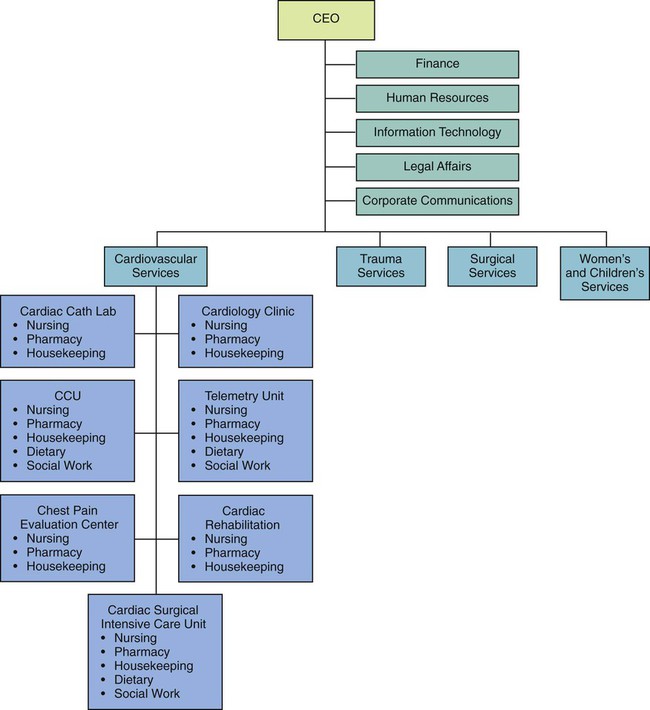
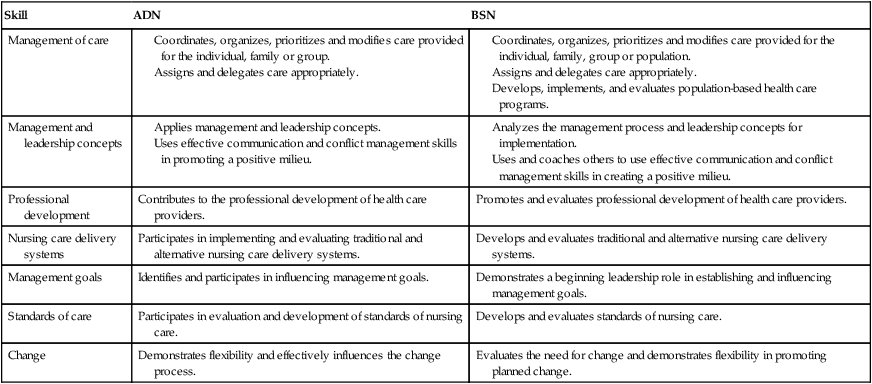
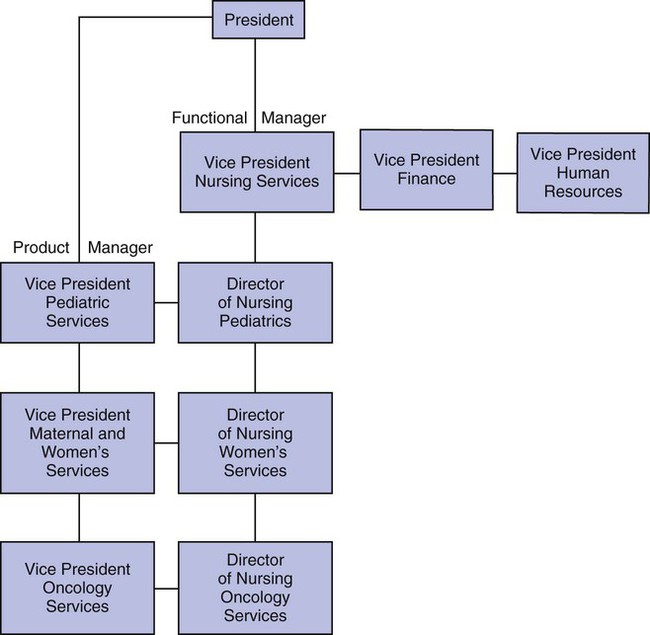
1. Differentiate between leadership and management. 2. Identify the management structures of patient care. 3. Describe the various modes of patient care delivery systems. 4. Discuss the pros and cons of each of the delivery systems. 5. Determine the responsibility of the nurse in the various care delivery systems. 6. Identify outcome measures of patient care management. 7. Relate a clinical scenario to each of the delivery models. Just because someone is in a leadership position, it does not automatically follow that this person is a leader. Some people have false assumptions about leaders and leadership. Many people believe that the position and title are the same as true leadership. Having the title of chief nurse does not necessarily mean that the person in that position is a leader, while being a staff nurse does not mean that person is not a leader. New nurse managers often make the mistake of believing that along with the new title comes the mantle of leadership. Leadership takes a tremendous amount of effort, time, and energy. Leadership can be defined as the use of individual traits and personal power to influence and guide strategy development. Leaders need to “do the right thing,” be future oriented, be visionary, focus on purposes, and empower others to set and achieve organizational goals. Management is the act of planning, organizing, staffing, directing, and controlling for the present. Management can be taught, whereas leadership is usually a reflection of personal experience. As shown in Figure 1-1, leaders show the way, while managers labor to produce the day-to-day outcomes. Leaders focus on effectiveness, and managers deal with efficiencies. A further review of leadership and management focuses on the major themes of each role (Table 1-1). The nurse, as manager, works collaboratively to achieve the desired outcomes of quality care, fiscal responsibility, and customer satisfaction by coordinating the care of individuals, families, groups, or populations through the effective use of technology, resources, information, and systems. Some health care agencies will differentiate between the level of academic preparation of the nurse and the expected competency of the manager (Table 1-2). Table 1-1 COMPARISON OF LEADERSHIP AND MANAGEMENT Bennis, W., & Nanus, B. (1997). Leaders: the strategies for taking charge. New York: Harper and Row. Table 1-2 COMPETENCIES OF ADN AND BSN NURSES ADN, Associate degree in nursing; BSN, Bachelor of Science in Nursing. Copyright 2000, by the Colorado Council on Nursing Education. There are numerous theories of leadership. How the leader approaches leadership is often very dependent on his or her personal experiences. Leadership also relies on the organizational structure and culture of the health care facility. Two leadership theories prevalent within health care today are transactional leadership and transformational leadership. In transactional leadership, there is an exchange between the leader and the employee. The needs of the employees are identified, and the leader provides rewards to meet those needs in exchange for performance. This type of leadership usually takes place in a hierarchal organization. A hierarchal organization is one where decision making occurs at the top of the structure and is communicated to the employees. Transformational leadership is more consultative and collaborative. Kouzes and Posner (2002) identify five basic practices in transformational leadership: 1. Challenging the process, questioning the ways that things have always been done, and creatively thinking of new ways of doing things 2. Motivating and inspiring shared vision or bringing everyone together, moving toward the shared goal One form of governance often used by transformational leaders is shared governance. This is a democratic, dynamic process resulting from shared decision making and accountability (Porter-O’Grady, 2001). In shared governance, there is the creation of organizational structures that allow nursing staff autonomy to govern their practice (Batson, 2004). Functional structures arrange services and departments according to their function (Figure 1-3). Departments providing similar functions would all report to a common manager or vice president. This type of structure supports professional expertise but can result in the “silo” effect, where departments become separate silos with little interaction. In product line structures, the functions necessary to produce a specific service are brought together into an integrated unit under the control of a single manager (Figure 1-4). For example, the orthopedic service line at a hospital would include all personnel providing services to the orthopedic service population. This might include the orthopedic ambulatory care service, the orthopedic operating rooms, the orthopedic trauma center of the emergency department, and the orthopedic rehabilitation center. Benefits of this model include coordination of all services within the specialty and a similarity of focus. A limitation would be increased expense due to duplication of services. Matrix structures combine both function and service line in an integrated service structure (Figure 1-5). In a matrix organization, the manager of a unit responsible for a service reports both to a functional manager (vice president for nursing) and a service manager (directors of the services: cardiovascular services, trauma services, surgical services, or women’s and children’s services). Such a structure requires a collaborative relationship between the service line and functional manager. The nurse is responsible to the nurse manager and vice president of nursing for nursing care and to the program director when working within the matrix. A patient care delivery model is the method used to deliver care to patients. There are multiple care delivery models, and the choice of a model within an organization is dependent on many factors: financial, staffing capabilities, patient population, and organizational mission and philosophy. The fundamental element of any patient care delivery system (Manthey, 1990) is a combination of the following: The following are the models associated with hospital practice: Total patient care is the oldest method of providing care to a patient. It is sometimes called case method (not to be confused with case management). It was the primary care delivery model until the 1930s, and it had a resurgence in the 1990s. In this model, one nurse assumes accountability for the complete care of a group of patients. It has been described as a type of primary nursing (Reverby, 1987), but in total patient care the accountability for coordination of care does not extend beyond the assigned shift. This is the type of care seen in private duty nursing and some intensive care units and was the model of care used by Florence Nightingale. Advantages of total patient care: • Quality of care—all care is delivered by a registered nurse • Continuity of care for a given shift • Decreases communication time between staff • Reduces the need for supervision Disadvantages of total patient care: • May not be cost effective because of the number of registered nurses needed to provide care • Some nurses dislike this model because they believe that some of the patient care activities could be done by others with less skill An example of a patient care assignment using the total patient care model is shown in Table 1-3. Table 1-3 PATIENT CARE ASSIGNMENT USING THE TOTAL CARE MODEL
Patient Care Management
LEADERSHIP VERSUS MANAGEMENT
COMPARISON OF LEADERSHIP AND MANAGEMENT
Leadership
Management
Motto
Do the right thing
Do things right
Challenge
Change
Continuity
Focus
Purposes
Structures and procedures
Time frame
Future
Present
Methods
Strategy
Schedule
Questions
Why?
Who, what, when, where, how?
Outcomes
Journeys
Destinations
Human
Potential
Performance
Skill
ADN
BSN
Management of care
Management and leadership concepts
Professional development
Contributes to the professional development of health care providers.
Promotes and evaluates professional development of health care providers.
Nursing care delivery systems
Participates in implementing and evaluating traditional and alternative nursing care delivery systems.
Develops and evaluates traditional and alternative nursing care delivery systems.
Management goals
Identifies and participates in influencing management goals.
Demonstrates a beginning leadership role in establishing and influencing management goals.
Standards of care
Participates in evaluation and development of standards of nursing care.
Develops and evaluates standards of nursing care.
Change
Demonstrates flexibility and effectively influences the change process.
Evaluates the need for change and demonstrates flexibility in promoting planned change.
THEORIES OF LEADERSHIP
LEADERSHIP STRUCTURE IN HEALTH CARE
FUNCTIONAL STRUCTURES
PRODUCT LINE STRUCTURES
MATRIX STRUCTURES
MAJOR TYPES OF CARE DELIVERY SYSTEMS
TOTAL PATIENT CARE
Hester B., RN, MSN
Patient Care Manager 4 West
Joseph Z., RN, BSN
Full patient care, documentation, orders, admissions, discharges—rooms 410-414
Maria C., RN
Full patient care, documentation, orders, admissions, discharges—rooms 415-417
Joy T., RN, BSN
Full patient care, documentation, orders, admissions, discharges—rooms 418-420
Michael Y., RN
Full patient care, documentation, orders, admissions, discharges—rooms 421 and 422
Clarisa T., RN
Full patient care, documentation, orders, admissions, discharges—rooms 423-425 ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Patient Care Management
Get Clinical Tree app for offline access