Chapter 13 Patient and machine monitoring and assessment
What are dialysis treatment outcome standards?
The National Kidney Foundation (NKF) Kidney Disease Outcomes Quality Initiative (KDOQI) provides guidelines with indicators for outcomes. Four different clinical practices guidelines—hemodialysis adequacy, peritoneal dialysis adequacy, treatment of anemia, and vascular access—are used to assess and improve the outcome of each dialysis. Other guidelines have been developed, including nutrition, dyslipidemia, bone disease, and hypertension. Additional guidelines for pediatrics have also been developed. (See Appendix A for additional information on NKF KDOQI.)
General assessment parameters
What is meant by the patient’s dry weight?
Dry weight is the ideal postdialysis weight after the removal of all or most excess body fluid. Patients who are at dry weight are usually normotensive. If the postdialysis weight suggests that volume status is too high, the patient may be on the borderline for fluid overload and may be hypertensive. If postdialysis weight is too low, the patient may be hypovolemic and at risk for hypotension and clotting of the vascular access.
How much weight gain is permissible between dialysis treatments?
Weight gained between dialysis procedures is due to fluid retention. Most dialysis units encourage patients to limit their weight gain to 0.5 kg (or 1 lb) per day. (Refer to Chapter 14 for further discussion and calculation of fluid restrictions.)
Why are temperature, pulse, and respiration monitored?
Temperature, pulse, and respiration (TPR) observations serve as a baseline at the start of dialysis. Temperature elevation suggests infection or complicating illness. An elevated temperature is often a sign of vascular access infection. Fever during dialysis may be caused by high dialysate temperature or by a pyrogen reaction. A rapid pulse may result from anemia or fluid overload. Irregular heart rate (arrhythmia) may indicate cardiac complications, including those associated with serum potassium levels. An increase in pulse rate during dialysis may be associated with falling blood volume (from UF) and may occur just before a drop in BP. Increased respiratory rate may indicate excessive fluid gain. Any unexpected findings should be reported to the physician.
First hemodialysis assessment
What procedures take place before the first hemodialysis?
The physician evaluates and prescribes the dialysis orders for the new patient. The nurse reviews the orders and, after the fluid composition and machine settings are programmed, starts predialysis assessment. Before the first meeting with the patient, medical records should be reviewed. This information will be helpful during the physical assessment. After introductions, a brief tour around the facility should be conducted. The first visit should be as simple and as pleasant as possible. Remember that instructions will have to be repeated many times.
Predialysis assessment
What is included in the patient’s predialysis assessment?
Predialysis assessment includes the following:
• Fluid status (respiratory rate and effort, JVD, heart sounds, breath sounds, presence of edema)
• TPR, including apical and peripheral pulse evaluation
• Skin color, temperature, turgor, and integrity
• Vascular access patency and freedom from bleeding and infection
• Interpretation of physical assessment and laboratory data for appropriate intervention and medication administration
What other checks should be done on the dialysis machine before patient use?
It is necessary to ensure that machine functions have been checked and that they work correctly. All extracorporeal alarms should be tested to ensure that they respond appropriately. Arterial pressure, venous pressure, and air detector alarms should all cause the blood pump to stop and the venous line clamp to close. In addition, conductivity and temperature of the dialysate should be tested to ensure that they are within the proper range. These alarms must be working at all times so that, if any problems arise, the dialysate will be diverted from the dialyzer and a major complication will be avoided. Finally, there should be an adequate amount of dialysate concentrate to complete the patient’s treatment.
What is included in machine preassessment?
Machine preassessment includes the following:
• Dialyzer membrane check for patency and integrity
• Blood tubing intact without leaks
• Appropriate prescribed dialyzer
• Dialysate fluid composition as ordered and within safe limits (12.8 to 14.8 mho) as read by a Myron-L meter
• Appropriate prescribed dialysate potassium and calcium
• Temperature within limits (35°C to 37°C)
• Correlation of machine conductivity with an external meter reading of dialysate (Myron-L or pHoenix)
• Dialysate delivery system free of sterilant or disinfectant agents
• Extracorporeal blood circuit free of air
• Blood pump properly occluded
• Dialyzer bloodline tubing free of kinks or crimps
• Blood pump segment of tubing properly seated in the pump segment
• Physician’s orders reviewed to ensure adherence to dialysis prescription
• All alarms programmed and set within limits
• Dialysis quality water evaluated for chlorine and chloramines
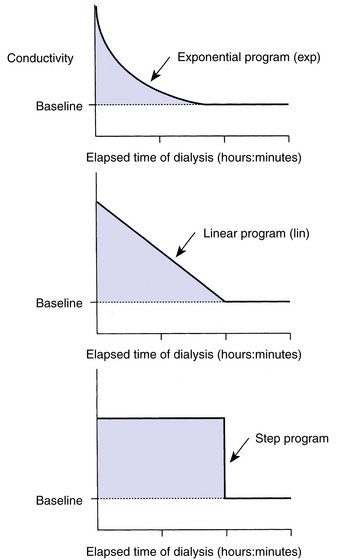
What is sodium modeling or sodium variation, and when is it applicable?
Sodium variations allow the dialysis treatment to be modified by increasing the concentrate-to-water ratio slightly, resulting in a rise in dialysate sodium. This feature allows the dialysis staff to initiate hemodialysis with a high-dialysate sodium concentration and use progressively lower sodium-containing dialysate, decreasing to the original baseline level in a programmed time and profile. These maneuvers are intended to reduce the incidence of hypotension and cramping. By varying the level of sodium in the dialysate, the drop in osmolality of the patient’s serum is more gradual. The fluid that is in the interstitial spaces in the tissues does not transfer into the vascular spaces as fast as the dialysis machine is able to remove it. The result of this is fluid depletion of the vascular space and the resultant side effects of hypotension. The sodium variation system keeps the vascular space filled enough to prevent this fluid depletion from occurring. There are several machines available to perform this treatment function. The Fresenius 2008H has three sodium variation system profiles: step decrease, linear decrease, and exponential decrease. Fig. 13-1 illustrates these system profiles. The baseline is determined by the basic setting of the mechanical acid/acetate and bicarbonate concentrate pumps. With this method of sodium modeling there is a significant variation in the dialysate potassium level. If the dialysate sodium is increased from 140 to 160 mEq/L (about 14%), the dialysate potassium concentration will also increase by 14%. If the baseline concentrate has 3 mEq/L of potassium and is increased by 14%, the new potassium concentrate would be 3.4 mEq/L. If there is a decrease in the dialysate sodium to 120 mEq/L (decrease of 14%), the new potassium concentrate will be 2.6 mEq/L. Increasing sodium in the dialysate has assisted many patients in the prevention of hypotension, cramping, and disequilibrium syndrome during dialysis. The physician writes the orders for the sodium modeling for each patient.
Why is it necessary to do such a thorough assessment of the patient and the machine before initiation of the dialysis treatment?
What is ultrafiltration?
UF is the removal of fluid during dialysis. It is the result of hydrostatic force across the dialysis membrane. The difference in hydrostatic pressure, blood to fluid, is the TMP. The rate of UF is the sum total of positive and negative pressures plus the filtration factor, known as the UF coefficient (kUF), of each individual dialyzer. The kUF ranges from 0.5 to 80.0 mL/h/mm Hg, depending on specific dialyzer characteristics (see Chapter 6).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree