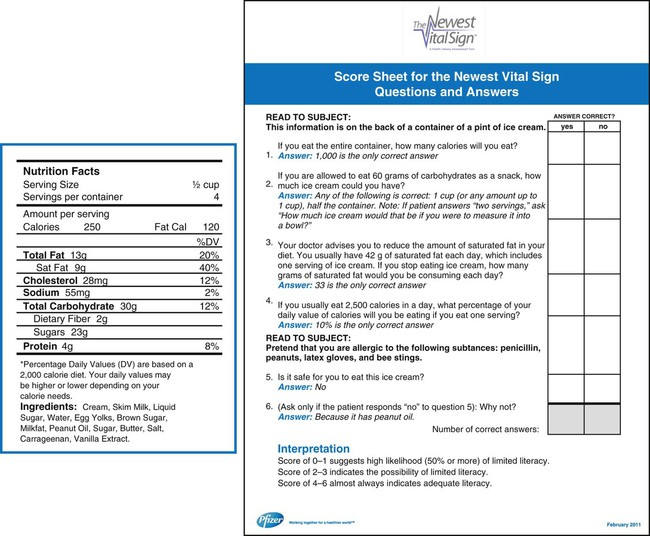
When alterations in health arise in daily life, people use all available resources to discover information to help them cope and adapt to the new experience. This type of consumerism has developed a populace that is more educated in health matters than ever before. It is our duty as health professionals to assist patients and families with information gathering and self-care management skills so they can lead lives of the best quality possible. According to The Joint Commission, patients must receive “sufficient information to make decisions and to take responsibility for self-management activities related to their needs.”1 The goals of patient and family education are to improve health outcomes by promoting healthy behavior and involvement in care and care decisions.1 Admission to a critical care unit usually is an unexpected event in anyone’s life. The seriousness of the situation and unfamiliarity of the hospital or unit environment evokes a stress response in patients and their families. Nursing care is focused on improving the patient’s physiologic stability and promoting end-organ tissue perfusion. Promoting the most basic human physiologic survival need for cellular oxygenation is the priority. Alterations in normal functioning related to disease-process progression, sedation, assist devices, or mechanical ventilation contribute to the possibility of mental alterations in the patient. Sleep deprivation and sensory overload add to the complexity of the issues that affect the patient’s ability to receive and understand medical information. Mental alterations may limit the effectiveness of the teaching-learning encounter. These physical and cognitive limitations prevent patients from receiving or understanding information related to their care and impair their ability to make an informed decision.2 At these times, critical life-or-death care decisions are transferred to a proxy, usually an immediate family member. The designated proxy has the responsibility to make informed treatment decisions for the patient. These types of situations present the nurse with special challenges in the education of patients and families. Critical illness disrupts the normal patterns of daily life. Stress and crisis can develop within the family unit and stretch its members’ coping resources.3 These many emotional factors build barriers to the teaching-learning process and can become frustrating for the learner and the nurse. Amid the chaos, how do bedside nurses effectively provide patient and family education that can optimize outcomes and deliver quality, cost-effective care? It is the nurse’s responsibility to educate himself or herself about concepts that provide insight into the framework for patient and family education. Adult educational concepts such as adult learning principles, types of educational needs, barriers to learning, stress and coping strategies, and evidence-based interventions must be used to develop an individualized education plan to meet the identified learning needs of the patient and family. Patient education is a process that includes the purposeful delivery of health-related information to promote changes in behavior that will optimize health practices and assist the individual in attaining new skills for living.4,5 This concept can be overwhelming in the fast-paced, technology-rich setting of the critical care environment. The bedside nurse must incorporate the abundant educational needs of the patient or family into the education plan and be aware of the requirements of regulatory agencies and the legalities of documenting the teaching-learning encounter. Studies have documented that quality education shortens hospital length of stay, reduces readmission rates, and improves self-care management skills.4–6 Complications associated with the physiologic stress response may be prevented if the patient or family perceives the education encounter as positive. Positive encounters decrease the stress response, relieve anxiety, promote individual growth and development, and increase patient and family satisfaction.4–6 The following are examples of positive outcomes associated with a structured teaching-learning process.7,8 • Clarification of patients’ understanding and perceptions of their chronic illness and care decisions • Improved health outcomes relative to self-management techniques, such as symptom management • Promotion of informed decision making and control over the situation • Diminished emotional stress associated with an unfamiliar environment and unknown prognosis • Improved adaptation to stressful situations • Improved satisfaction with the care received • Improved relationship with the health care team The education process follows the same framework as the nursing process: assessment, diagnosis, goals or outcomes, interventions, and evaluation.4 Although this chapter discusses these steps individually, in practice, they may occur simultaneously and repetitively. The teaching-learning process is a dynamic, continuous activity that occurs throughout the entire hospitalization and may continue after the patient has been discharged. This process is often envisioned by the nurse as a time-consuming task that requires knowledge and skills to accomplish. Whereas knowledge and skills can be obtained, time in the critical care unit is a scarce commodity. Many nurses believe they cannot educate unless formal blocks of education time are planned during the shift. Although this type of education encounter is optimal, it is not realistic for contemporary nursing. The nurse must recognize that teaching occurs during every moment of a nurse-patient encounter.9 Instructions for how to use to the call bell or explanations of events and sensations to expect during a bed bath can be considered an education session. It is the nurse’s role to recognize that education, no matter how brief or extensive, affects the daily lives of each person with whom he or she comes in contact. By following the nursing process, the physical assessment and education assessment can occur simultaneously. According to The Joint Commission, education provided should be appropriate to the patient’s condition and should address the patient’s identified learning needs.1 The assessment is an important first step to providing need-targeted patient and family education. It begins on admission and continues until the patient is discharged. A formal, comprehensive, initial education assessment produces valuable information; however, it can take the nurse hours to complete. The nurse must focus the initial and subsequent education assessments on identifying gaps in knowledge related to the patient’s current health-altering situation. Learning needs can be defined as gaps between what the learner knows and what the learner needs to know, such as survival skills, coping skills, and ability to make a care decision. Identification of actual and perceived learning needs directs the health care team to provide need-targeted education. Need-targeted or need-to-know education is directed at helping the learner to become familiar with the current situation. Educational needs of the patient and family can be categorized as 1) information only (environment, visitation hours, get questions answered); 2) informed decision making (treatment plan, informed consent); or 3) self-management (recognition of problems and how to respond).5,10 Patient education to be included in the education plan should address the plan of care, health practices and safety, safe and effective use of medications, nutrition interventions, safe and effective use of medical equipment or supplies, pain, and habilitation or rehabilitation needs.1 Learning needs may change from day to day, shift to shift, or minute to minute. Educational needs are influenced by how the patient or the family perceives or interprets the critical illness.11 Perceptions of experiences vary from person to person, even if two people are involved in the same event. This intense internal feeling affects the desire to learn and understanding of the current situation. Satisfaction with the learning encounter is often judged to be positive if the nurse meets the expected learning needs of the patient and family. Congruency between nurse-identified needs and patient-identified needs brings about more positive learning experiences and encourages the learner to seek further information. The nurse must actively listen, maintain eye contact, seek clarification, and pay attention to verbal and nonverbal cues from the patient and the family to gather relevant information concerning perceived learning needs. The nurse should seek to first understand the learning need from the patient’s point of view and then seek to be understood. Strategic questioning provides an avenue for the nurse to determine whether the patient or family has any misconceptions about the environment, their illness, self-management skills, or the medication schedule. Health care providers use the term noncompliant to describe a patient or family members who do not modify behaviors to the meet the demands of the prescribed treatment regimen, such as following the rules of a low-fat diet or medication dosing. However, the problem behind noncompliance may not be a conscious desire to defy the treatment plan but instead be a misunderstanding of the importance of the medication or how to take the medication. The technique of asking open-ended questions (“Can you tell me what you know about your medication?”) can elicit more information about the patient’s knowledge base than asking closed-ended questions (“You know this is your water pill, right?”). Open-ended questions provide the nurse an opportunity to assess actual knowledge gaps rather than assume knowledge by obtaining a yes-or-no response. These types of questions also assist the patient and family to tell their story of the illness and communicate their perceptions of the experience,5 allowing the adult learner to feel respected and involved in the treatment process. Questions that elicit a yes-or-no response close off communication and do not provide an interactive teaching-learning session. Box 5-1 contains sample questions the nurse can use in an assessment to obtain needed information. Generally, with practice and effort, it can be determined what educational information is needed in a brief period without much disruption in the routine care of the patient. Patients and families are multidimensional. Even with good questioning skills, the nurse cannot assess many aspects of the learner during the initial contact or even during the hospital stay. Identifying learner characteristics benefits the nurse and results in optimal communication and the patient’s understanding of information. Certain factors can affect the education process. Culture or ethnicity, age, and adult learning principles influence the manner in which information is presented and concepts are understood.5,12 A family can be defined as a group of individuals who are bonded by biologic, legal, and social relationships.3 The modern family is diverse in ethnic backgrounds, sexual orientation, age, gender, work experience, physical or mental challenges, communication skills, educational backgrounds, work experience, geographic location, lived experiences, and religious beliefs.13–15 A picture of the modern family would resemble that of a large patchwork quilt. Patches of different sizes, ethnicities, religions, cultures, attitudes, stages of development, and lived experiences would overlap and occupy their own individual spaces within the quilt framework. Bedside practitioners are expected to provide culturally competent care to each individual in the critical care setting. Culturally competent care is the delivery of sensitive, meaningful care to patients and families from diverse backgrounds.15 This implies that the practitioner must value diversity and become knowledgeable concerning the cultural strengths and abilities of those for whom they care.16 Communication and understanding impact the education process. Provision of language-appropriate literature and translation services and recognition of cultural or religious differences in the perception of illness and treatment influence the education encounter.15 The critical care patient population differs culturally and by age and stages of human development. Older adult patients may have more difficulty reading patient educational materials or the label on the bottle of prescription medication than younger adults. Printed materials with larger fonts may be needed for these patients. Older adults were not exposed to technology during their youth and may find it difficult to navigate the fragmented maze of modern health care. Because of advanced age, this population of adults may have prescriptions for multiple drug therapies. Education to prevent adverse drug reactions may be required because of the prevalence of multiple drug therapies.17 Older adults may also be coping with end-of-life issues and are in need of information to make informed decisions. Young adults may struggle with the issue of how to incorporate intimacy into their lives without feeling isolated from the mainstream social scene. The need for privacy and peer support may be required to assist the young adult in coping with the current situation. The practitioner must recognize these age-specific issues and incorporate them into the education plan.1 Adults learn in large part through lived experiences. The motivation to learn is internal and problem-oriented, focusing on life events. Malcolm Knowles described these principles of adult learning in a model known as andragogy. Adult learning theory stresses concepts of individualism, self-assessment, self-direction, motivation, experience, and autonomy. Adults tend to have a strong sense of self-concept, are goal-oriented learners, and like to make their own decisions.18 They take responsibility and accountability for their own learning and want to be respected as individuals, as well as recognized for accomplished life experiences. Adults have individualized learning styles and often lack confidence in their ability to learn. Education is resisted when the information given is perceived to be in conflict with the individual’s self-image. The learning process generally involves altering some part of current behavior to produce changes in lifestyle, incorporating the new or chronic illness into daily living. Coping mechanisms such as anger, disbelief, and denial affect the willingness of the patient or family to learn. The unwillingness to change behavior to manage health needs adds to the complexity of the critical care teaching-learning encounter. The nurse must provide need-to-know information in easy, understandable terms and in short bursts. Positive feedback and repetition of information may also be required before health education is incorporated into the patient’s or family’s bank of experiences.18 Adults are sensitive about making mistakes and tend to view mistakes as failures. Learning situations that the patient and family interpret as belittling or embarrassing or that are perceived as insurmountable will be avoided or disregarded. The nurse should act more as a coach or facilitator of information instead of a didactic instructor.12 The teacher can only show the learner to the door; the learner must decide to walk through that door. Learning is an active process that occurs internally over time and cannot be forced. Bedside nurses are obliged to be proactive and to have a good understanding of adult learning theory and to incorporate its concepts into the assessment of learning needs, development of an education plan, implementation of the plan, and evaluation of the outcomes of the education encounter. Information must also be gathered on factors that affect the education process and impair the ability of the patient or family to respond. These factors include 1) desire and motivation; 2) physical or cognitive limitations; 3) cultural and religious views of illness or health; 4) emotional barriers; and 5) barriers to effective communication.1 For teaching to be successful and learning to be achieved the patient or family must be ready, willing, and able to learn. The ability to learn is the capacity of the learner to understand, pay attention, and comprehend the material being taught. Willingness to learn describes the learner’s openness to new ideas and concepts. Readiness to learn is the motivation to try out new concepts and behaviors.5 Even if the inventive teaching methods, well-considered education materials, and amounts of time are unlimited, learning cannot take place if the patient or family is not ready, willing, and able to learn.19 Several factors affect the ability, willingness, and readiness to learn, as well as the ability to cope and adapt to the current situation. These factors include physiologic, psychologic, sociocultural, financial, and environmental aspects.5,12 Physiologic alterations in heart rate and blood pressure can be measured and taken into consideration during the teaching-learning encounter.3 Sources of physiologic stress in the critically ill include medications, pain, hypoxia, decreased cerebral and peripheral perfusion, hypotension, fluid and electrolyte imbalances, infection, sensory alterations, fever, and neurologic deficits.12 Experiencing one or more of these stressors may completely consume all the patient’s available energy and thoughts, affecting his or her ability to interact, comprehend, and respond to teaching. Patients and families may be ready and willing to learn but lack the ability to comprehend and act upon the information presented to them. In its report Health Literacy: A Prescription to End Confusion the Institute of Medicine (IOM) states that nearly half of adult Americans struggle to understand and follow the health information they are provided. The IOM defines health literacy as “the degree to which individuals have the capacity to obtain, process and understand basic health information and services needed to make appropriate health decisions.” However, health literacy goes beyond the individual. Practitioners must develop the ability to present information and instructions in a way that patients and families can best understand.20 Assessing health literacy is not an easy task, but knowing what to look for can make it easier. Several tools are available to assist health care professionals to screen for low literary skills. Generally, these tools fall into four categories: 1) word recognition; 2) reading comprehension; 3) functional health literacy; and 4) informal methods.21,22 Each tool has both positive and negative aspects to its use. Functional health literacy tests assess the individual’s level of comprehension and ability to put into action what they have learned. Examples of these tests include the Test of Functional Health Literacy in Adults (TOFHLA)4 and the Newest Vital Sign (NVS).21–22 The TOFHLA requires the individual to complete missing sections of written statements to assess the ability to read and comprehend directions for taking medications, monitoring blood glucose, and keeping appointments.23 The tool takes 20-30 minutes to administer and score, making it undesirable for use in the critical care setting. An abbreviated version, the S-TOFHLA, is now available. It takes approximately 10-12 minutes to complete and score. Figure 5-1 shows the NVS tool and scoring sheet. Shame has been cited as one of the most common emotions associated with low health literacy.24 Behaviors such as handing a form to a family member to complete, claiming to be too tired, or “forgetting” their glasses are a few behaviors that may be used by individuals to hide their limitations. Other behaviors that may also provide clues to a patient’s health literacy are listed in Box 5-2. Variables such as culture, ethnicity, values, beliefs, lifestyle, and family role influence the way an individual perceives illness, pain, and healing.15 Culturally sensitive educational strategies should be developed to communicate specific needs to other members of the health care team and achieve optimal learning outcomes.1 When confronted with life-altering situations such as admission to a critical care unit, patients and families may experience anxiety and emotional stress. Anxiety and fear disrupt the normalcy of daily life. Sources of emotional stress include fear of death, uncertain prognosis, role change, self-image change, social isolation, disruption in daily routine, financial concerns, and unfamiliar critical care environment.3,20 These intense emotions can lead to a crisis situation and alter the ability of the patient and family to cope.25,26 During the critical illness, an individual’s ability to process or retain information and ability to participate in the treatment plan could be altered.2 If the disease process or physiologic stressors impair the patient’s ability to make decisions, the burden of decision making will transfer to the family. Gender differences affect a patient’s reaction to stress. For example, women who have experienced a myocardial infarction report higher anxiety levels than men at all points during the hospital stay.27 Physiologic alterations caused by anxiety negatively impact the recovery process and the long-term prognosis.27 In critical situations, the nurse may find it necessary to repeat information or limit teaching sessions to short bursts rather than one long encounter. Medical jargon should be limited and replaced by terms that are easy to understand. Provision of honest and accurate disease state information may decrease the effects of stressors and alleviate anxiety and fear. Coping refers to the way a person manages stressful events that are straining or exceeding personal resources.5,28 The stressful event is appraised according to the level of threat to the individual and is managed by focusing on the problem at hand or the emotions felt at the moment.29 Critical illness disrupts the normalcy of daily routines. Coping strategies are used by the patient and family to help maintain control over the situation and encourage hope and stability in life. Disbelief and denial may be present any time during the hospitalization. Phrases such as “Why me” and “I can’t believe this is happening” are common in the critical care setting. Other coping mechanisms, such as denial and anger, hamper the ability of the patient or family to problem solve and cope with the situation. All are barriers to the ability of the patient to receive information and incorporate it into the self-concept. Adults must be physically ready and emotionally willing to learn. Teaching new skills or self-management techniques to the adult learner therefore presents a special challenge to the nurse in critical care. For example, until the patient accepts the diagnosis of heart failure as part of who he or she is, he or she will not make appropriate changes in lifestyle to avoid an exacerbation of the disease. A stressor can be any condition, situation, or perception that requires an individual to adapt.30 All situations in a critical care facility may well be considered stressful. The capacity of an individual to adapt is paramount in breaking down emotional barriers that affect willingness and readiness for learning. Culture, beliefs, attitudes, and ability to mobilize resources affect a person’s ability to respond to a crisis situation.28 General characteristics of the stages of adaptation to illness are outlined in Table 5-1 with corresponding applications for the teaching-learning process. Patients and families move through these stages on an individual timeline and at a variable pace. A person may move back and forth between stages and may skip one altogether. The patient and each member of the family may be experiencing different stages in the adaptation process at the same time. The education encounter may need to be modified to meet the needs of the patient and family. TABLE 5-1 TEACHING-LEARNING PROCESS IN ADAPTATION TO ILLNESS The critical care environment can be considered a source of stress to the learner. Although sounds, people, and state-of-the-art equipment are familiar and mundane for the nurse, this environment may appear foreign and intimidating to the patient and family. Prior exposure to a critical care unit is a double-edged sword. Depending on whether the outcome of the experience was positive or negative, it may help alleviate or heighten anxiety. The nurse must pay attention to the perceptions of the environment by the patient and family and alter the teaching-learning encounter accordingly. Sleep cycle alterations caused by sleep deprivation or sensory overload related to continuous noise from machines or people affect the patient’s ability to concentrate and comprehend information. Allowing frequent uninterrupted rest periods assists the patient in obtaining structured sleep.30 For patients and families to value education, they must believe the information source is reliable. The bedside nurse is the most available source of information in the critical care unit. It is important for him or her to develop a rapport and establish a sense of trust within the nurse-patient relationship. These positive characteristics are recommended for a supportive learning environment. Assignment of multiple caregivers may negatively affect the ability of the patient and family to form a trusting relationship with the nursing staff. Arranging consistency in the assigned caregivers can help promote rapport and trust, as well as decrease anxiety and enhance comfort level with the environment.5,28 Education must be ongoing, interactive, and consistent with the patient’s plan of care and education level.1 The nurse must analyze information gathered from the assessment to prioritize the educational needs of the patient and family. The nursing diagnosis for deficient knowledge and accompanying interventions can be applied to any situation. The nurse must also consider the patient’s physical and emotional status when setting education priorities. Ability, willingness, and readiness to learn are factors that impair acceptance of new information and add to the complexity of teaching-learning encounter. These factors should be recognized by the nurse before implementation of teaching. The written teaching plan should identify the learning need, goals or expected outcome of the teaching-learning encounter, interventions to meet that outcome, and appropriate teaching strategies. It can be difficult to prioritize the multitude of learning needs that practitioners are required to address during a period in critical care. Learning needs in the critical care unit, the progressive care, or the telemetry setting can be separated into four different categories to help set teaching priorities in each phase of the hospitalization (Table 5-2). Learning needs during the initial contact or first hours of hospitalization can be predicted. Education during this time frame should be directed toward the reduction of immediate stress, anxiety, and fear rather than future lifestyle alterations or rehabilitation needs. Interventions are targeted to promote comfort and familiarity with the environment and surroundings.31 The plan should focus on survival skills, orientation to the environment and equipment, communication of prognosis, procedure explanations, and the immediate plan of care. TABLE 5-2 CATEGORIES OF EDUCATIONAL NEEDS IN CRITICAL CARE
Patient and Family Education
Challenges of Patient and Family Education
Education
Definition
Benefits
The Education Process
Step 1: Assessment
Learner Identification
Family
Age-Specific Considerations
Adult Learners
Factors Affecting the Learning Process
Readiness, Willingness, Ability
Physiologic Factors
Health Literacy
Sociocultural Factors
Psychologic Factors
Coping
Adaptation
STAGE OF ADAPTATION
CHARACTERISTIC PATIENT RESPONSE
IMPLICATIONS FOR TEACHING-LEARNING PROCESS
Disbelief
Denial
Orient teaching to present.
Teach during other nursing activities.
Reassure patient about safety.
Explain all procedures and activities clearly and concisely.
Developing awareness
Anger
Continue to orient teaching to present.
Avoid long lists of facts.
Continue to foster development of trust and rapport through good physical care.
Reorganization
Acceptance of sick role
Orient teaching to meet patient.
Teach whatever patient wants to learn.
Provide necessary self-care information; reinforce with written material.
Resolution
Identification with others with same problem; recognition of loss
Use group instruction.
Use patient support groups and visits by recovered patients with same problem.
Identifying change
Definition of self as one who has undergone change and is now different
Answer the patient’s questions as they arise.
Recognize that as basic needs are met, more mature needs will arise.
Environmental Factors
Step 2: Education Plan Development
Determining What to Teach
PHASE
EDUCATIONAL NEEDS
Initial contact or first visit, with a focus on immediate needs
Preparation for the visit: patient representatives or nurses can prepare the family and patient for the first visit
What to expect in the environment
How long the visit will last
What the patient may look like (e.g., tubes, IV lines)
Orientation to the unit or environment: call light, bed controls, waiting rooms, unit contact numbers
Orientation to unit policies and hospital policies
HIPAA, advanced directives, visitation policies
Equipment orientation: monitors, IV pumps, pulse oximetry, pacemakers, ventilators
Medications: rationale, effects, side effects
What to do during the visit: talk to the patient, hold the patient’s hand, monitor length of visits (if applicable)
Patient status: stable or unstable and what that terminology means
What treatments and interventions are being done for the patient
Upcoming procedures
When the doctor visited or is expected to visit
Disciplines involved in care and the services they provide
Immediate plan of care (next 24 hours)
Mobilization of resources for crisis intervention
Continuous care
Day-to-day routine: meals, laboratory visits, doctor visits, frequency of monitoring (VS), nursing assessments, daily weights, and shift routines
Explanation of any procedures: expected sensations or discomforts (e.g., chest tube removal, arterial sheath removal)
Plan of care: treatments, progress, patient accomplishments (e.g., extubation)
Medications: name, why the patient is receiving them, side effects to report to the nurse or health care team
Disease process: what it is and how it will affect life, symptoms to report to health care team
How to mobilize resources to assist the patient and family in coping with stress and crisis: pastoral care, social workers, case managers, victim assistance, domestic violence counseling
Gifts: When a loved one is ill, it is traditional to send flowers, balloons, or cards. If your unit has restrictions on gifts, make the family aware.
Begin teaching self-management skills, and discuss aftercare information.
Transfer to a different level of care
Sending Unit
Acknowledge positive move out of critical care
When the transfer will occur
Why the transfer is occurring
What to expect in the different unit
Name of the new caregiver
Availability of care provider
Visiting hours
Directions for how to get there; the new room number and phone number
Receiving Unit
Orientation to environment, visitation policies, visitors
Unit routine, meals shift changes, doctor visits
Expectations about patient self-care; ADLs
Medication and diagnostic testing routine times
Planning for aftercare, discharge planning
Self-care management: symptom management, medication administration, diet, activity, durable medical equipment, tasks or procedures
What to do for an emergency
What constitutes an emergency or when to call the physician
How to care for incisions or procedure sites
Completed throughout the hospital stay
Return appointment: name of physician practice, practice phone numbers and contacts
Obtaining medications: prescriptions, pharmacy, special medication ordering information
Required lifestyle changes: mobility and safety issues for the paraplegic or stroke victim, activities of daily living issues relative to medications or symptoms
Potential risk modifications: smoking cessation, diet modifications, exercise
Resources: cardiac rehabilitation, support groups, home care agencies
End-of-life care
End-of-life care: participation in care, services available, mobilizing resources
Palliative care
Hospice ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Patient and Family Education
Get Clinical Tree app for offline access