25 Paediatric Considerations in Critical Care
After reading this chapter, you should be able to:
• consider and anticipate the specific needs of critically ill infants and children
• describe common conditions that lead to critical illness in infants and children
• discuss and apply the age-appropriate assessment, monitoring and management of critically ill infants and children
• identify age-appropriate parameters and care required by critically ill infants and children who require ventilation
• discuss psychological and emotional care required by critically ill infants and children, and their family
Introduction
In mid 2007 the Australian paediatric population was estimated to be 4.1 million children aged 0–14 years,1 with the New Zealand paediatric population 0–15 years reported at 894,400.2 Approximately 559,000 children were admitted to Australian public hospitals in 2007–20083 with over 8300 children in Australia and New Zealand requiring admission to intensive care units (ICUs) in 2008.4 During the same period, there were over 145,000 total admissions to Australian and New Zealand ICUs.5 Children represent 5.7% of all ICU admissions in Australia and New Zealand. Over half of these children required mechanical ventilation,4 compared with around 41% of adults in intensive care.5 While just over half (52.5%) of critically ill children were admitted to specialist paediatric ICUs, a significant number were managed in or retrieved from adult ICUs.4 Geographical distances and the centralised nature of paediatric services can influence whether a child is nursed in a general or paediatric ICU. In many circumstances, children will respond effectively to initial resuscitation, particularly support of breathing and fluid resuscitation, and may not require transfer to a specialist paediatric unit. Paediatric clinical advice, support and information are available from children’s hospitals and specialist paediatric retrieval services and should be sought as early as possible in the absence of paediatric trained staff, or when the need for transfer to a higher level of care becomes apparent.
The age distribution of children in ICUs has remained the same for a number of years, with the figures from 2008 showing that children under the age of five years represent just over 66% of admissions, with almost 59% of this age group under 12 months of age and 26% under four weeks of age. Boys make up 58% of children admitted to ICUs.4 The overall ICU mortality rate is 11% for Australia and 13% for New Zealand,4 however the paediatric mortality rate is 3%.5 Over the past 30 years, although length of stay and severity of illness to the PICUs have not essentially changed, mortality has halved while disability has increased.6
Anatomical and Physiological Considerations in Children
• Children have increased surface area to volume ratio compared with adults, which leads to increased heat loss and insensible fluid losses, placing infants and children at increased risk of developing hypothermia and dehydration. Providing an environment that maintains the infant and small child’s body temperature is essential. Avoid exposing infants and children more than necessary; use warming blankets, open care systems for all newborns and infants under 4 kg and overhead heaters when exposure is unavoidable. Temperature monitoring is required when using any heating devices to avoid iatrogenic thermal injury.
• Lower glycogen stores and increased metabolic rate predispose infants to hypoglycaemia. There are few standard doses in paediatric ICU; rather, medication doses and fluid requirements are calculated on age and kilograms of body weight. Weight of infants and children should therefore be estimated as accurately as possible. The Broselow tape measure is a colour-coded method to estimate weight and is particularly accurate in children ≤ 25 kg.7,8 Some differences may occur in estimated weight of children of different origin.7
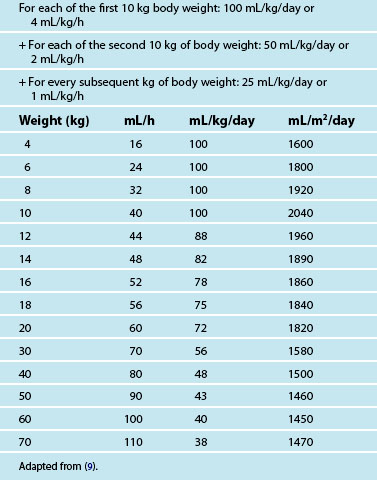
• Fluid requirements are based on body weight, and aim to ensure adequate hydration while preventing fluid overload. Maintenance intravenous (IV) fluids for infants and young children typically require the addition of glucose. Common IV maintenance fluids used are 0.45% sodium chloride with either 2.5% glucose or 5% glucose and 0.9% sodium chloride with 5% glucose.9 Isotonic sodium chloride is recommended as the first choice fluid bolus in paediatric resuscitation.10 Table 25.1 provides a guide for fluid maintenance requirements of children based on body weight.
• Excluding the newborn period, normal values for all blood gas and serum electrolyte levels are the same as adult levels. Creatinine and urea levels will vary with age.
• Methods of oxygen delivery (humidified if possible) for infants include via nasal prongs (maximum rate 2 L/min) or a head box. A head box can reliably deliver a required percentage of oxygen, but visualisation of the infant is often compromised and there is a sense of separation between the parents and the infant. Comforting, touching and regular nursing assessment are more easily achieved when nasal prongs are used. Hudson masks and partial non-rebreather masks are available in paediatric sizes.
Central Nervous System
Many central nervous system functions, such as locomotion and hand–eye coordination, will take from months to years, to fully develop. Functions of the cerebral cortex are particularly underdeveloped, with myelination of all major nerve tracts continuing throughout infancy.11 Consequently, assessment and management priorities will be dictated by the level of neurological maturity of the infant or child. As with adults, neurological dysfunction in infants and children may be primary or secondary. The plasticity inherent in the brain of the infant may compensate for injury more readily than older children and adults in some circumstances, with other areas of the infant’s brain taking over function. Because the eight cranial bones are not yet fused, infants’ skulls cope with both birth and ongoing growth, which is greatest in the first two years of life. In the first year, the cartilaginous sutures fuse at two points to form the posterolateral fontanelle. The larger anterior fontanelle closes during the second year as bone is laid down. By around five years of age, the sutures of the child’s skull are completely fused.12 However the thinner skull will provide less protection to underlying tissues than the adult skull.
A common misconception is that the Monro-Kellie doctrine (see Chapter 16) does not apply to young children and infants with a more compliant skull. While slow rises in intracranial volume may be accommodated over time in children under three years of age, they will usually be accompanied by growing head circumference, making routine measurement of head circumference in children under three years of age an important assessment. However, the less rigid skull of the older child will not compensate for acute rises in intracranial volume, and the child will display symptoms of neurological compromise.12 Normal ranges of intracranial pressure (ICP) and cerebral perfusion pressure (CPP) have not been formally studied in infants and children, but are presumed to be lower than in adults, reaching adult range by adolescence. Values that are commonly used to guide treatment are age-related and are displayed in Table 25.2.
TABLE 25.2 Target cerebral perfusion pressure (CPP) by age
| Age | Desirable minimum CPP |
|---|---|
| Infants under 1 year | 45–55 mmHg |
| Children 1–10 years | >55 mmHg |
| Children over 10 years | >65 mmHg |
Adapted from (9).
Cardiovascular System
In infants, approximately 70% of the haemoglobin is fetal haemoglobin (HbF), allowing greater amounts of oxygen to be carried for any given PaO2. Circulating blood volume per kilogram decreases with age; in the infant, circulating volume is approximately 85 mL/kg, with total body water accounting for 70% of body mass, adjusting to the adult values of 65 mL/kg and total body water of 60%.13 The apex beat is heard at the fourth intercostal space, mid-clavicle, and by around seven years of age the left ventricle has grown and the apex beat can be heard at the fifth intercostal space, as in adults. An infant’s cardiac output is approximately 500 mL/min, which, relative to body weight, is about twice that of an adult.14 Heart rate is a major determinant of cardiac output in infants and young children, as there is limited ability to increase stroke volume. Tachycardia is an early sign of distress, but bradycardia is an ominous sign in infants and young children, as they are more dependent on a high heart rate to maintain cardiac output. In infants, bradycardia requires resuscitation.13
Arterial blood pressure should be appropriate for age, weight and clinical condition. Mean arterial pressure is generally used. Monitoring blood pressure using correct cuff sizes is important because incorrect cuff size is a common cause of inaccurate blood pressure readings in children. Diastolic blood pressure is recorded at Korotkoff sound 5 (K5); age-related parameters for mean blood pressure are displayed in Table 25.3. Tachycardia in the absence of fever is a more reliable sign than hypotension, as up to 25% of the child’s circulating volume may be lost before hypotension occurs. Hypotension is thus a late sign in children and may indicate late decompensated shock, particularly following fluid delivery.14
TABLE 25.3 Age-related mean blood pressure
| Age | Mean BP (mmHg) |
|---|---|
| Term | 40–60 |
| 3 months | 45–75 |
| 6 months | 50–90 |
| 1 year | 50–90 |
| 3 years | 50–90 |
| 7 years | 60–90 |
| 10 years | 60–90 |
| 12 years | 65–95 |
| 14 years | 65–95 |
Adapted from (9).
Paediatric Considerations for Cardiovascular Assessment
Cardiovascular assessment in children includes clinical parameters that are similar to those observed in adults. The normal values are, however, age and weight dependent. Urine volume in infants should average 2 mL/kg/hr, with 1 mL/kg/hr in children and 0.5–1 mL/kg/hr in adolescents. Other indirect evidence of poor systemic perfusion in infants may include:15
Indirect evidence of poor systemic perfusion in children is irritability, then disorientation or lethargy. Clinical signs of reduced cardiac output, typically seen in shock, are similar to adults.16
Respiratory System
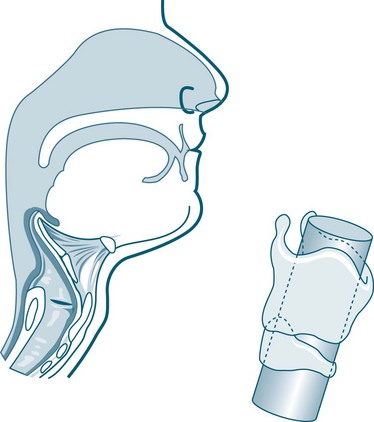
The newborn’s larynx is just one-third of the diameter of the adult larynx.17 Narrow nasal passages, in combination with being obligatory nose-breathers up to 5–6 months of age, means that infants may experience respiratory distress if nasal passages become oedematous or contain secretions such as mucus or blood. With the airway of an infant measuring around 6 mm in diameter at the level of the cricoid, obstruction is more likely. The paediatric airway is characterised and differentiated from an adult airway by the following features:13,17
• more acute angle of airway, particularly notable when attempting to visualise with a laryngoscope
• a more cephalad larynx that moves distally as the neck grows
• the cricoid ring is the narrowest portion of the airway
• smaller lower airways, less developed with fewer alveoli
• true alveoli not present until 2 months, with full complement developed by around eight years of age
• little smooth muscle present in airways
• little collateral ventilation in airways, as the pores of Kohn are not fully developed until about eight years of age (see Figures 25.1 and 25.2).
Paediatric Respiratory Assessment
Newborn infants have a respiratory rate of approximately 40 breaths/min, generating an average tidal volume of 16 mL/kg and minute volume of 0.64 L/min.18 The thoracic cavity of infants and children is characterised by a thin chest wall that is highly compliant, with poorly developed intercostal and accessory muscles. The diaphragm is the most important muscle for infants and children in respiration, with abdominal muscles also used. The compliant chest wall prevents generation of high intrathoracic pressures, meaning that infants and young children are unable to significantly increase tidal volume; rather, they increase minute volume by breathing faster. This means that tachypnoea is a normal response to illness in infants and children, and a slowing respiratory rate in children may indicate impending collapse rather than clinical improvement.18,19
Assessing airway patency is important. Talking and crying indicates that the infant or child is maintaining their own airway. Adventitious airway noises in children include wheeze, stridor and grunting. In infants, grunting may be heard and is an attempt by the baby to produce positive end-expiratory pressure (PEEP). Infants and children who are grunting, gasping or unconscious need urgent assessment for possible endotracheal intubation.19
Other observed signs of respiratory distress in infants and children up to about eight years old include head bobbing in infants, nasal flaring, and paradoxical chest movement observed in several locations on the chest and known as recessions. Recessions can be observed at the costal margin, or subcostal; between the ribs, or intercostal; at the sternum, or sternal; and at the trachea, called tracheal tug. Oral feeding is difficult for infants in moderate to severe respiratory distress due to limitations associated with sucking and breathing at the same time. In addition, tachypnoea greater than 60–80 breaths/min may lead to vomiting and aspiration.20 For these reasons, initial enteral feeding might not be possible or desirable, so nutrients should be given as parenteral nutrition (PN) until enteral feeding is tolerated.21
Gastrointestinal Tract
There are few differences between the child’s and adult’s gastrointestinal tract outside the neonatal period; although a palpable liver below the costal margin is a normal finding. It will be up to 3 cm below the costal margin in normal infants, decreasing to 1 cm by 4–5 years of age, and should no longer be palpable in adolescents. In the neonate, a relative pancreatic amylase deficiency means utilisation of starches is less effective. Fats are also absorbed less well; the reason why higher-fat milks such as cow’s milk are not ideal for infants. Protein synthesis and storage is however enhanced in the neonate.13
As the infant liver is not completely mature at birth, gluconeogenesis is deficient, causing low and unstable blood sugar level in the first weeks of life. The infant is therefore reliant on fat stores until normal feeding is established.13 Formation of plasma proteins and clotting factors are likely to be inadequate in the first weeks of life, thus all newborns in Australasia are given vitamin K shortly after birth to prevent bleeding. Blood glucose monitoring and provision of early nutrition are essential aspects of care, especially for infants. Children normally have increased metabolic demands to achieve growth but have fewer energy stores than adults.
Other Systems and Considerations
Genitourinary System
The small developing pelvic bones of infants and young children cause adult pelvic organs, such as the bladder, to be located in the lower abdominal cavity. Urine output in children is calculated in mL/kg bodyweight/hour. In infants with immature kidney function and limited ability to conserve water, urine output should be 1–2 mL/kg/h. In the first month of life, infants have the capacity to concentrate urine to only 1.5 times their plasma osmolality, while adults can concentrate their urine to 3–4 times their plasma osmolality. The higher metabolic rate of infants means that they produce twice the acid that an adult will, leading to a tendency to acidosis in critical illness.22 By six months of age, normal urine output should be 1 mL/kg/h, and by adolescence 0.5–1 mL/kg/h is considered normal. Catheterisation is generally required in critically ill infants and children for accurate hourly measurement of urine output. Where this is not possible, particularly where small sizes of indwelling catheters are not readily available, weighing nappies will provide an interim estimate of urine output. Inserting feeding tubes in place of a urinary catheter is not recommended.
Musculoskeletal System
Children have less developed musculature than adults, with less protection from external forces that collide with the child. Conversely, a child’s skeleton is more cartilaginous than adults and therefore more pliable. As a result, rib fractures rarely accompany chest trauma in children while lung contusions are common.23 The skeleton in children changes from less cartilaginous in nature at infancy to complete ossification and adult features during adolescence, so daily calcium requirements increase over childhood and adolescence.24
Integumentary System
Infants have a thinner epidermis, dermis and subcutaneous tissue that will continue to mature. This results in a greater susceptibility to absorption of chemicals, injury from adhesive tapes and any shearing force, and loss of water and heat, particularly in the newborn period.22 Critically ill children are more likely to develop pressure areas on the occiput, ear, sacrum, heel, or thigh; 50% of pressure ulcers in children are associated with equipment pressing or rubbing on the skin.25 A commonly used tool for assessing risk of development of pressure areas in children is the modified Braden Q scale. This shorter version includes three subscales (mobility, sensory perception, tissue perfusion/oxygenation) with a cutoff score of 7 and has comparable psychometric properties to the adult Braden scale26 (see Chapter 6). However, recent evidence suggests that the Glamorgan paediatric pressure ulcer risk assessment scale may perform better than the Braden Q scale.27,28 The Glamorgan scale includes ten subscales: anaemia, equipment pressing, mobility, poor peripheral perfusion, pyrexia, serum albumin, surgery in last 4 weeks, weight < 10th centile, continence, and nutrition.27
Developmental Considerations
Admission to ICU is very stressful for paediatric patients29 as well as for their family.30–33 The stressors, combined with the effects of critical illness, can lead to disturbances in normal child development and attachment. The psychological needs of children and families are not always met.34 Factors that affect the psychosocial wellbeing of a critically ill child include loss of usual routines and self-control; family presence and role; family and friends’ visits, comfort and the ICU environment.29,35–37
Knowledge and understanding of developmental psychology can help nurses assess and plan care for the critically ill child.38,39 Identification of internal strengths, external supports and environmental modification can facilitate coping and reduce stress in these children.40 Parental support is an important coping mechanism of infants and children during periods of stress.36 Strategies to facilitate coping in children of all ages include:
• facilitating parental presence at all times, including during invasive procedures and resuscitation41,42
• maintaining normal routines and rituals as much as possible, including story reading, bedtime routines and presence of favourite toys
• providing appropriate analgesia and sedation as well as non-pharmacological interventions
• providing opportunities for play and activities unrelated to treatment.
Erikson’s psychosocial theory is helpful for understanding childhood development.43 Erikson’s theory asserts that people experience eight ‘psychosocial crisis stages’ which significantly affect their development and personality. The first five stages are presented below.
Infants (Stage 1)
The first year of life is concerned with developing a sense of trust, which lays the foundation for all future relationships.38,43 More specifically, the affective exchanges between the infant and the primary caregiver provide a foundation for neurological development and lead to the creation of neural networks (particularly in the right hemisphere) that will influence the infant’s personality and relationships with others throughout life.44,45 Generally, up to the age of six months, infants are able to cope with limited separation from their mothers; however, changes to usual routine create anxiety and stress.43 From around 6–18 months of age separation is the major fear, with changes to usual routine and environment resulting in anxiety.43 Therefore, critically ill infants require parental presence and maintenance of normal routines, including breastfeeding, as much as is practicable.
Toddlers (Stage 2)
The toddler period, between 12 months and three years of age, is a time for establishing autonomy and independence. Control over bodily functions, increasing ability to communicate, ability to view the self as separate from others, and being able to tolerate brief separation from the mother are all developmental characteristics during this period.46 Toddlers tend to be egocentric in how they view the world, so illness, procedures and separation from parents may be perceived as punishment.43 Their thinking processes include transduction, animism and ritual.39 Transductive thinking allows a child to link unrelated objects or events, such as separation and endotracheal suction if suction occurs after the parent leaves the room. Animism attributes lifelike traits to inanimate objects, so the ventilator becomes a hissing monster, or monitoring leads may be trying to trap them. Many toddlers have varying levels of ritual or sameness, including always eating off the same plate, different foods that should not be touched, or a security toy or blanket. Regression, or loss of recently-acquired skills such as toileting, may also occur during critical illness, creating further distress. When caring for a critically ill toddler, encourage parental presence and maintain as many of the usual rituals and routines as possible to facilitate coping.47
Preschool Children (Stage 3)
Children from 3–5 years of age fall into the preschool period of development. This period is characterised by discovery, inventiveness, curiosity, and the development of culturally- and socially-acceptable behaviour.38,39,43 Preschoolers can generally verbalise their needs reasonably well.48 While thought processes become less ritualistic and negative, they are still egocentric and magical thinking emerges, thus ideas about causality and linking events may be faulty. Fears, both real and imagined, are prevalent during this period.39 For example, fears of monsters or being hurt may occur. They may also feel guilty as a result of illness.43 There is, however, greater understanding of the passage of time, so parents can leave the preschooler for defined short periods. Hospitalisation remains difficult, but preschoolers respond to anticipatory preparation and concrete explanations.38
School-Age Children (Stage 4)
Children between 6 and 11 years are usually referred to as being of school age. This period represents a widening of the sphere of influence from parents/family to include the school environment and peers.39 A transition from egocentric thinking to concrete operations occurs,38,39 with children becoming more independent and achievement-oriented for their sense of self-worth. In the ICU, school-age children may have a distorted or fantasy-laden view, and will need concrete explanations. Sicker children are less able to cope with the ICU environment and are more likely to regress, which can have a significant impact on their sense of self-worth. Modesty and privacy is imperative at this age.49 Preadolescence occurs between 10 and 11 years, and represents a time of turmoil and emotional upheaval.39
Adolescents (Stage 5)
Adolescence is considered a time of transition from childhood to adulthood. It is a developmental stage rather than an age group, but is typically represented by children aged 12–18 years, or teenagers. Internal changes relate to emotional upheaval, search for autonomy, and transition of thought process from concrete to abstract.43 External changes relate to physical changes, such as the emergence of secondary sex characteristics with a related preoccupation on bodily functions and image.38
A goal in adolescence is to develop an integrated sense of self, achieved through managing the conflicting demands of family and peers. Peer identity is essential to psychological growth and development, as is the gradual shift from family to peer orientation. The peer group provides a way for the adolescent to self-evaluate and to bolster self-esteem. Adolescents also target authority figures with retaliation and defiance. Conversely, adolescents will seek out non-parental adults, such as a teacher or relative, to obtain approval and acceptance.50 Slote has described a process associated with adolescent illness.50 The first is hopelessness and helplessness provoked by the equipment and environment. Adolescents often think they will not get better, and need to be given clear information about the expected course of the illness. They also need to be included as much as possible in decision making and encouraged to participate in their own care. Feeling helpless and defenceless is contrary to their normal feelings of invincibility and may result in antisocial behaviours. The adolescent must learn to accept that the quest for autonomy has been temporarily interrupted. Acknowledging his/her feelings and setting clear behavioural limits can help an adolescent cope.50 Adolescents will also experience fear and anxiety. This can be offset by clear explanations and acknowledgement of feeling through articulation and reflection. Concerns for body image is also paramount, particularly fear of mutilation and scarring. Physical appearance is important for acceptance into the peer group and for self-esteem.50 In summary, in addition to considering age-related physical characteristics, critical care nurses need to also consider the developmental level of the child when providing care.
Comfort Measures
Critically ill infants and children are particularly vulnerable to pain. If pain remains unrelieved it may cause short- and long-term physiological and psychological complications, such as increased risk of mortality and morbidity.51–53 The assessment of pain in children is particularly challenging,51 but the use of valid pain and sedation assessment tools may be useful for the management of pain in critically ill children.54,55 Prevention of procedural pain is important not only to avoid pain-related complications and emotional trauma, but also to facilitate the procedure.56 Target sedation level according to the child’s clinical status may help maintain comfort without compromising haemodynamic and respiratory status,57 as well as minimising other undesirable effects of analgesics and sedatives.
Pain and Sedation Assessment
Recent advances in pain and sedation assessment show that they remain problematic in paediatric critical care and highlight the need for routine assessment, documentation and effective communication of the pain and sedation scores. Numerous pain assessment instruments have been developed, but few have been validated for the paediatric critical care population. These latter include the PICU-MAPS and the COMFORT behaviour scale. The PICU-MAPS is a multidimensional scale developed for critically ill children, including five categories of physiological and behavioural items, providing a possible pain score between 0 (no pain) and 10 (maximum pain).58,59 The COMFORT scale has been validated in several studies in PICU60,61 and comprises seven behavioural items, where only six are rated (alertness, calmness/agitation, respiratory response or crying, physical movement, muscle tone, and facial tension), generating a possible score between 6 and 30. In combination with pain, assessment of sedation is paramount and the State Behavioral Scale (SBS) is particularly relevant to evaluate the level of sedation in infants and children in ICU.62 It consists of a six-level responsiveness continuum, ranging from −3 (unresponsive) to +2 (agitated), with a neutral state ‘awake and able to calm’ of 0.
Pain and Sedation Management
Painful procedures should be minimised when possible. Some nonpharmacological therapies have been shown to be beneficial alone in managing mild pain or in combination with drug therapy in infants and young children. These therapies may include non-nutritive sucking (e.g. finger or pacifier) with or without sucrose (for infants up to 4 months), swaddling, music therapy,63 and distraction with or without parental presence.64
Pharmacological treatment of pain and sedation in infants and children should be tailored to the child’s need and condition. Continuous opioid (morphine) infusions are used at the lowest effective dose and minimum duration based on regular pain assessment. Fentanyl boluses are not recommended in neonates as they may cause glottic and chest wall rigidity.65 Sedation management in children is similar to that in adults, except for the use of propofol, which should be used with caution in children. Although there is no strong evidence, propofol infusion in children has been associated with sudden myocardial failure and death.66 More recent data shows that propofol has an acceptable safety profile and could be used in children for short term deep sedation under close monitoring of the airways.67 Use of dexmedetomidine in paediatrics is promising, but additional safety and efficacy studies need to be carried out before routine use as a sedative agent can be recommended in children.68 Indications for the use of neuromuscular blocking agents in children, monitoring of the effects and management are similar to adult practice.69
Family Issues and Consent
When children are admitted to an ICU, the whole family is affected by the hospitalisation. ‘Family-centred care’ (FCC) provides a framework for the care of children and their family in hospital. FCC means that during a hospital stay, nursing care is ‘planned around the whole family, not just the individual child, and in which all the family members are recognised as care recipients’.70, p. 1318 Parents should receive unbiased information at regular times, be involved in the decision-making process and the care of their child; this parent–professional collaboration should be facilitated at all levels of healthcare.70,71 As the developmental issues highlight, parents are essential to a child’s coping with critical illness. Critically ill children are particularly vulnerable to short- and long-term emotional and psychological sequelae, but parental presence and participation in care can make a difference.72
Parents need to feel involved in their child’s care, which includes the need for information, communication, understanding the child’s illness and being part of the decision-making process.31,34,73,74 A partnership between staff and parents is the ideal situation, but parents often need to be reminded on how to maintain the parental role and how they can effectively care for both their child’s and their own psychological health.75 Parents should be allowed to be present during potentially stressful situations such as endotracheal suction, cannulation and resuscitation if they choose to, providing adequate support from a nurse or another designated health care worker is given.41 Being present at the end of their child’s life may help them accept the death.42 Not allowing parents to be present during procedures is a form of paternalism that goes against the right of the patient.64 Parents should however be informed that it is their right to leave if they wish.
Consent and Assent
Except for emergency treatment, parents or legal guardians need to consent to all aspect of medical care, including preventive, diagnostic or therapeutic measures for children. The legal age of consent differs between legislations but is 18 years in major European countries and all Australian states, except New South Wales and South Australia, where the legal age for consent is 14 and 16 years, respectively.76 However, a young person with the emotional maturity and intellectual capacity to agree to medical procedures, in circumstances where he or she is not legally authorised or lacks sufficient understanding for giving consent competently can provide informed assent.77,78 To be considered competent, young people must be able to understand the nature of the decision as well as the consequences of making or not making the decision.78 Whenever possible, it is recommended to obtain the child’s assent for treatment or procedures. Children, even when deemed not competent, have the right to be informed and, when appropriate, to be asked for their permission. However refusal of treatment by a child has no legal bearing when a parent has consented. Importantly, parents may also refuse consent, and in that case national laws and legal mechanisms for resolving disputes may be used.77,79
The Child Experiencing Upper Airway Obstruction
General Description and Clinical Manifestations
• a longer inspiratory phase with unchanged expiratory phase
• recessions of the chest wall
• in infants, head bobbing and nasal flaring
Observing and listening to the child’s symptoms without disturbing them will provide important clues about the level and degree of obstruction the child is experiencing. The aim is to assess the child without causing further distress, as a crying, agitated child can further increase the degree of obstruction and work of breathing, leading to respiratory collapse.80 The Paediatric Assessment Triangle (PAT) is a useful tool to facilitate rapid assessment of the child’s appearance, work of breathing, and skin circulation.81 Stridor indicates obstruction in the upper airway, while wheeze is suggestive of lower airway disease. When stridor is also associated with a barking cough, it is likely to be croup. A softer stridor in a child who looks systemically unwell may indicate epiglottitis. When a previously well child presents with a sudden onset of stridor, it is likely to indicate foreign body aspiration, and eliciting the history of a sudden choking episode can clarify the diagnosis.19,80,82
Congenital Airway Abnormalities
Laryngomalacia is the most common cause of stridor in the newborn period. Stridor is produced by flaccid, soft laryngeal cartilage and aryepiglottic folds that collapse into the glottis on inspiration.83 An inspiratory stridor, usually high-pitched, will be present. It may be intermittent, may decrease when the patient is placed prone with the neck extended, may increase with agitation, and is usually present from birth or the first weeks of life. The infant’s cry is usually normal. Feeding problems may be associated with increased respiratory distress. Laryngoscopy confirms the laryngomalacia diagnosis. Treatment is supportive, with only a small proportion of infants requiring airway reconstructive surgery unless respiratory distress interferes with feeding and growth, in which case a tracheostomy may be indicated.84
A laryngeal web is made of membrane that typically spreads between the vocal cords, with an inspiratory stridor present soon after birth. Diagnosis is confirmed by laryngoscopy. Treatment involves lysis in the case of thin membranous webs while a tracheostomy may be required for a thicker fibrotic web. Laryngeal webs can also develop after contracting illnesses such as diphtheria, and are occasionally reported in otherwise normal adults, typically at intubation for an operative procedure.85
Tracheomalacia and tracheobronchomalacia involve malformed cartilage rings, with lack of rigidity and an oval shape to the lumen. Secondary tracheomalacia is associated with prolonged intubation and prematurity and presents within the first year of life.17 Malacias are characterised by wheezing and stridor on expiration, with collapse of the tracheal or bronchial lumen. Diagnosis is confirmed by fluoroscopy and bronchoscopy, which demonstrate tracheal collapse on expiration. As the infant grows, cartilaginous development improves the airway by about two years of age, but a number of children will require airway stenting or reconstructive surgery.83
Vascular rings result from congenital malformations of the intrathoracic great vessels, resulting in compression of the airways.83 Infants present with stridor at birth or within the first few weeks of life. Other symptoms include wheezing, cough, cyanosis, recurrent bronchopulmonary infections, and dysphagia. Diagnosis may be confirmed by CT scan, MRI scan or endoscopy, which reveals indentations secondary to the extrinsic pressure of the vasculature.84 The anatomy of the vascular malformations is determined by angiography. Treatment is surgical correction of the vascular malformation.84
Monitoring and Diagnostics
Lateral airway X-rays are unlikely to be helpful in the setting of croup and epiglottitis and, when they are likely to involve separating the child from a parent, are potentially harmful and not recommended.19 When there is a less dramatic presentation of the infant or child, or when the diagnosis is not clear, as in the case of an inhaled foreign body, then a chest X-ray may be diagnostic.
Managing the Paediatric Airway
A child’s airway may be managed in a number of ways. Simple positioning may be all that is required to manage an infant’s airway. Children will often assume an upright sitting position and may become more distressed if placed into the supine position, thus when possible the best position for an infant or child with upper airway obstruction may be sitting on their parent’s lap. Because of the anatomy and physiology of the respiratory tract, avoid extending the head of infants. Chin-lift and jaw-thrust are useful airway adjuncts in children to maintain an airway and to facilitate use of a bag–valve–mask. It may be necessary to use an oropharyngeal airway or nasopharyngeal airway, laryngeal masks and endotracheal intubation in an unconscious or sedated infant.19,80
Intubation
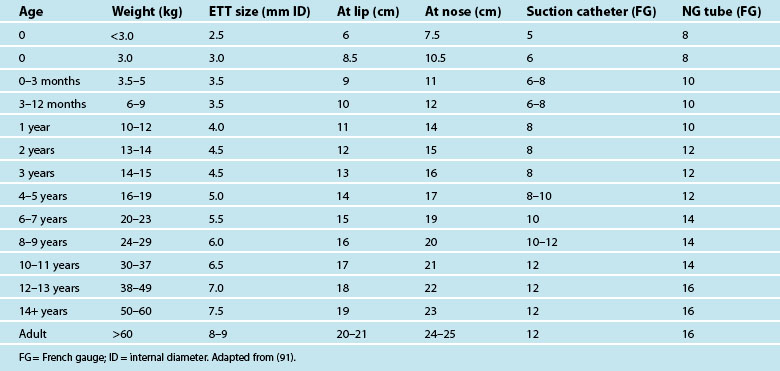
Intubation may be required to manage airway obstruction.86 Uncuffed endotracheal tubes (ETT) have been favoured in paediatric practice over cuffed tubes. Inflating the cuff of a regular ETT can cause damage in prepubescent children, as the subglottic area is the narrowest portion of their airways. The recent availability of a paediatric-specific ETT with microcuff and markings to ensure correct placement below the glottis has facilitated ventilation when a leak is undesirable, including in the child with facial and airway burns,87 and when using inhaled nitric oxide and for high frequency ventilatory strategies such as oscillation ventilation. Equipment necessary for paediatric intubation are shown in Figure 25.3. Figure 25.4 shows a range of sizes of uncuffed ETTS: 2.5 mm to 5.5 mm, that should be available in 0.5 mm increments, while cuffed ETTs are now available in sizes from 3 mm through to 9 mm. Selecting the correct ETT size includes having the recommended tube size plus tubes that are 0.5 mm larger and smaller than that. For children over 1 year of age, several formulae exist to calculate appropriate tube sizes, but the age-based and the fifth fingernail width-based predictions of ETT size are the most accurate.88 Table 25.4 provides a guide for ETT sizes, suction catheter size and nasogastric tube size for different-aged infants and children.
Practice tip
To calculate ETT tube size and length, use the following formula from the 2010 Australian and New Zealand Resuscitation Guidelines:89
• For term newborns ≥3 kg: size 3.0 mm or 3.5 mm (uncuffed tubes) or 3.0 mm (cuffed tubes)
• For infant up to 6 months: size 3.5 mm or 4.0 mm (uncuffed tubes) or 3.5 mm (cuffed tubes)
• For infant 7 to 12 months: size 4.0 mm (uncuffed tubes) or 3.5 mm (cuffed tubes)
• For children over 1 year: Uncuffed tubes: size (mm) = age (years)/4 + 4 or Cuffed tubes: size (mm) = age (years)/4 + 3.5
The most common method used to intubate children is the rapid-sequence method. Rapid-sequence intubation is performed where the child may have a full stomach and is at risk of aspiration during intubation.90 It involves the practically simultaneous administration of hypnotic medication and a muscle relaxant immediately before intubation.92,93 The main advantages of this method include good airway visualisation with a relaxed jaw, open immobile vocal cords, and the elimination of all movement, including gagging and coughing.90
Specific Conditions Affecting the Upper Airway
Bacterial and viral infections of the upper airway are common in children. Croup is the most common infection causing upper airway obstruction in children. Epiglottitis is now rarely seen since immunisation against Haemophilus influenzae type b (Hib) was introduced into the immunisation schedule for all Australian and New Zealand children. However, it is important to distinguish epiglottitis from croup in order to initiate appropriate management. Other less common infectious causes of upper airway obstruction seen in young children include bacterial tracheitis and retropharyngeal abscess, while diseases thought to have disappeared, such as Lemierre’s syndrome and diphtheria have not been completely eradicated.94
Infection of the lymphoid tissue around the nodes draining the nasopharynx, sinuses and eustachian tubes may cause pus to accumulate in the retropharyngeal space, leading to a retropharyngeal abscess. Presenting symptoms include history of upper respiratory tract infection (URTI), sore throat, fever, toxic appearance, meningismus, stridor, dysphagia, and difficulty handling secretions.94 Diagnosis is usually made on bronchoscopy. Treatment involves surgical drainage and antibiotic administration. Short-term intubation may be required until swelling has resolved following surgery.
Croup
Croup (laryngotracheobronchitis) is used to describe a set of symptoms caused by acute swelling causing obstruction in the upper airway (larynx, trachea and bronchi) from inflammation and oedema, caused mostly by the parainfluenza or influenza viruses.84,95 Croup occurs in approximately 2% of Australian children, generally aged 1–4 years, and in winter months.96 Recent advances in croup management have been responsible for a fall in the number of children requiring hospitalisation and intubation. Possible complications of croup include respiratory failure, respiratory arrest, hypoxic damage, secondary bacterial infection, acute pulmonary oedema, persistence or recurrence.84
Clinical manifestations
Croup is characterised by a barking or seal-like cough, inspiratory stridor and hoarse voice.97 The severity of croup is assessed based on increased respiratory rate, increased heart rate, altered mental state, work of breathing and stridor. Stridor at rest is noted in moderate to severe croup and is often quite loud. If a child’s stridor becomes softer but the work of breathing remains increased, it should be treated as an emergency as the obstruction may become more severe.98 The symptoms of croup are listed and compared with those of epiglottitis in Table 25.5. Diagnosis is made on physical assessment and the history of the illness.
TABLE 25.5 Clinical features of croup and epiglottitis
| Croup | Epiglottitis | |
|---|---|---|
| Aetiology | Viral | Bacterial |
| Age | 6 months–3 years | Infancy through adulthood |
| Onset | Subacute (over days) | Acute (over hours) |
| Fever | Mild (±38°C) | Severe (>38.5°C) |
| Cough | Present (often barking or seal-like) | Absent |
| Drooling | Absent | Present |
| Activity | Distressed | Lethargic |
| Colour | Pale/sick | Toxic |
| Obstruction | +++ | + |
| Stridor | Inspiratory, high-pitched | Expiratory snore |
| Sore throat | Uncommon | Common |
| Position | Any | Tripod; sitting up |
| Course | Gradual worsening or improvement | Unpredictable; fatal if not treated |
| Season | Autumn–winter | Throughout the year |
Adapted from (95).
Management
Management of croup depends on the severity of the upper airway obstruction and close cardiorespiratory observation and monitoring is essential. Children with moderate to severe croup should be given face-mask oxygen and allowed to adopt the position which they find most comfortable. Strategies such as positioning the child in a parent’s lap and holding the face-mask close to their face may limit their distress and can have beneficial effects on oxygenation.97
The use of steroids in combination with nebulised adrenaline is responsible for significant improvement of symptoms in children within 12 hours of administration, abating the need for intubation in the vast majority of cases.97,98 Nebulised adrenaline is efficacious to reduce airway inflammation, with effects seen within five minutes and lasting up to two hours. Although inhalations can be repeated, the benefits lessen with subsequent treatments. Adrenaline does not alter the course of croup.
Epiglottitis
Epiglottitis is inflammation of the epiglottis, frequently involving surrounding structures, with the classic description of a swollen, cherry-red, softened and floppy epiglottis, which tends to fall backwards, obstructing the airway.99 Obstruction also occurs circumferentially, from the oedematous, inflamed aryepiglottic folds surrounding the larynx. It is typically caused by Hib and since the introduction of childhood immunisation programmes to protect against Hib infection, the incidence has dropped from 23.8 cases per 100,000 children in 1991 to 2.81 per 100,000 in 2002 in the UK.100 A similar pattern was observed in Australia with a drop in prevalence rate from 22.7 to 3.3 per 100,000 children in 1998 and 2008, respectively.101,102 Hib infection can cause meningitis, septicaemia, septic arthritis and cellulitis as well as epiglottitis. The disease process and development of major symptoms progress rapidly over a few hours and an untreated child may become acutely obstructed. A child will make a full recovery without sequelae if diagnosis and treatment are appropriate and timely. Supraglottitis has emerged in recent times as a more accurate description of a similar range of symptoms as epiglottitis, and has been linked with the herpes virus and other organisms, requiring treatment with aciclovir and vancomycin.99
Clinical manifestations
The child with epiglottitis presents looking unwell with a fever, is unable to swallow secretions, drooling saliva and refusing to talk or swallow. The child may maintain an upright position, usually leaning with the head extended, supporting a sitting position with the arms stretched out behind in what is known as the tripod position. Hypoxaemia is usually present. Sudden respiratory arrest followed by cardiac arrest, can occur unpredictably. Cardiac arrest is likely to be asystolic in rhythm due to either vagal stimulation or hypoxia secondary to airway obstruction.94
Management
The most important aspect in the management of epiglottitis is rapid diagnosis and minimal handling of the child until an airway is in place. Children with epiglottitis require urgent intubation because acute airway obstruction followed by cardiac arrest is a potential hazard. Thus, the aim of management at this time is to keep the child as calm as possible until the airway is secured.19,99 The child should be nursed propped up with pillows or on a parent’s lap while arrangements are made for the insertion of an ETT. Procedures such as cannulation and examination of the throat should be avoided until the child’s airway is secure.95
Prophylaxis with antibiotics is required for families and household contacts if there is an infant under 12 months of age and/or a child in the household under the age of five years who is not fully immunised. Where the infected child has attended childcare for more than 18 hours each week, it is recommended that staff and other children at the centre also receive antibiotic prophylaxis.82
Foreign Body Aspiration
Aspiration of a foreign body into the upper airway is another relatively common cause of obstruction in children. Infants tend to swallow food items such as nuts and seeds, while toddler-aged children tend to swallow coins, teeth, and small toys or toy parts.103 An inhaled foreign body is likely to have a rapid onset with no previous symptoms. Sometimes the diagnosis is missed for days, weeks or even months, and the child’s symptoms may be non-specific, such as a cough with or without blood-stained sputum.83,103
Clinical Manifestations
Sudden onset of coughing, gagging and an audible stridor in a previously-well infant or child is suggestive of an inhaled foreign body.83 However, an accurate history – such as a recent coughing or choking episode – is the most sensitive factor in making a diagnosis of inhaled foreign body.
Management
Management will depend on the location and level of the aspirated foreign body, as it may have lodged in the pharynx, oesophagus, larynx, trachea or bronchial tree. Coughing is encouraged for mild airway obstruction.104 Up to five back blows may be successful in dislodging the foreign body, which may be followed by up to five chest thrusts and back blows. Direct laryngoscopy and removal of a foreign body using Magill forceps may be required for an acute episode when back blows and chest thrusts have been unsuccessful. When the foreign body has lodged below the carina, for the majority of children diagnosis and definitive treatment will consist of removal of the foreign body via a bronchoscopy under general anaesthesia.83
The Child Experiencing Lower Airway Disease
Lower airway disease in children is a common reason for admission to ICU. Infants under 12 months usually present with bronchiolitis or pneumonia. Asthma is more common in older children, but infants nearing 12 months of age may develop asthma105 and there is often confusion between bronchiolitis and asthma at this age.106
Specific Conditions
Bronchiolitis and asthma are commonly seen in children, and the management of each condition is discussed below. National and worldwide clinical guidelines for these conditions have been developed and are continually updated.107,108
Bronchiolitis
Viral bronchiolitis in infancy is characterised by obstruction of the small airways, resulting in air trapping and respiratory distress in infants less than 12 months of age. It is the most common severe respiratory infection in infancy, although the course is usually mild to moderate and is self-limiting, usually requiring no treatment. Severe infection represents less than 5% of all cases and is usually associated with prematurity or congenital heart disease.95 Respiratory syncytial virus (RSV) causes 90% of bronchiolitis cases.109 Other causative agents are parainfluenza virus types 1, 2 and 3, influenza B, adenovirus types 1, 2 and 5 and Mycoplasma. RSV invades the epithelial cells of the bronchioles, spreading via cell fusion and the creation of syncytia. This results in destruction of the epithelium and patches of necrosis. The debris associated with epithelial shedding and mucus production lead to small airway blockage and the clinical features of bronchiolitis.109
In temperate regions of Australia and New Zealand, most cases occur between late autumn and early spring, with sporadic cases throughout the year. There is a paradoxical relationship between the incidence of RSV and other viral pathogens causing bronchiolitis. RSV epidemics occur when other respiratory pathogen epidemics are diminishing, and vice versa. Although there are limited data on the actual incidence of bronchiolitis, laboratory isolation data in New South Wales estimate that about 1000 infants are hospitalised with bronchiolitis each year. The majority of these are under six months old.110 There is also a higher incidence of bronchiolitis in the Indigenous population of Australia111,112 and more severe illness when compared to non-Indigenous.113 Younger children with one or more comorbidities were at higher risk of complications.111 RSV infection occurs throughout the year, with an annual peak during the winter months.111,114
When bronchiolitis occurs, the highest risk for hospitalisation is infants under six months of age, those with exposure to tobacco smoke and underlying conditions such as congenital heart disease, prematurity and low socioeconomic group.20,102,115 Severe disease, requiring admission to a paediatric ICU, is associated with prematurity, particularly in infants with chronic lung disease or a history of ventilation in the newborn period and congenital heart disease.
Clinical manifestations
Bronchiolitis is a clinical diagnosis; non-isolation of a causative viral agent does not exclude the diagnosis. The clinical features of bronchiolitis are variable, and may include URTI symptoms such as rhinorrhoea (runny nose) and an irritating cough. Within three days the infant develops tachypnoea and respiratory distress, which may be mild, moderate or severe. An expiratory wheeze is often present and auscultation usually reveals fine to coarse crackles. Fever is present in approximately 50% of infants. In very young, premature or low-birthweight infants, apnoea is often the presenting symptom, which then develops into severe respiratory distress.116 The clinical course of bronchiolitis is usually 7–10 days; however, the effects of severe illness may last much longer. Respiratory distress is present. Indications for intensive care admission include frequent and/or prolonged apnoeas; hypoxaemia despite administration of oxygen; haemodynamic instability; an obviously tiring infant or decreased level of consciousness.20,117
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree