P
Papanicolaou smear
Includes: Human Papilloma Virus testing (HPV DNA)
Purpose of the test
The Papanicolaou smear is used to detect inflammation, infection, premalignant changes, and malignancy of the cervix.
Basics the nurse needs to know
The borderline lesion (inconclusive result) is defined as atypical squamous cells of undetermined significance (ASC-US). The squamous intraepithelial lesions (SIL) are graded from low grade to high grade. The low-grade squamous intraepithelial lesion (LSIL) consists of condyloma, mild dysplasia (CIN 1)—a precancerous state—or both. A high-grade squamous intraepithelial lesion (HSIL) ranges from moderate dysplasia (CIN 2) to severe dysplasia (CIN 3), including carcinoma in situ and invasive carcinoma or adenocarcinoma (Box 8).
Box 8 The Bethesda System for Reporting Cervical Cytology
From Katz VL, Lentz GM, Lobo RA et al: Comprehensive gynecology, ed 5, St Louis, 2007, Mosby.
Human papilloma virus
The human papilloma virus is the causative agent for genital warts and almost all cases of carcinoma of the cervix. There are 200 genotypes (genetic subtypes) of this virus, but 15 to 20 of them are capable of causing cancerous cervical mutations (Forbes, Sahm & Weissfeld, 2007). HPV infection is the most common of the sexually transmitted diseases. Diagnosis of the HPV infection and its viral subtype is made by HPV DNA probe assay performed on the cervical cells obtained from the PAP smear. Genotypes 16 and 18 cause 70% of the cases of cervical cancer and the remainder of the cases are caused by various other HPV genotypes (CDC, 2010).
Most women who are sexually active develop an HPV infection. Usually, these infections are cleared spontaneously within a few weeks to months. There are, however, some cases where the virus persists and eventually cancer of the cervix develops. To date, except for those women who are immunocompromised, there is no way to predict which women will be unable to eliminate the infection spontaneously.
How the test is done
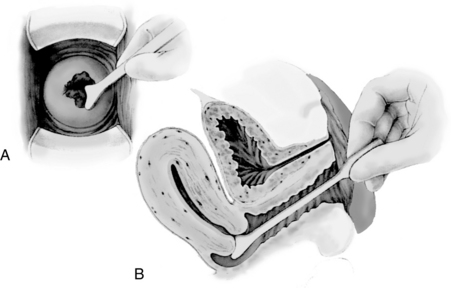
Using a vaginal speculum to enhance visibility, the physician or nurse practitioner collects the patient’s secretions and cells from the cervix (Figure 74). The fluid and tissue scrapings are placed in the specimen jar with liquid-based/thin prep solution. In the laboratory, the cells of the tissue are examined microscopically. A sample of the cells also can be analyzed for the DNA of the human papilloma virus and its genotype.
Interfering factors
NURSING CARE
During the test
Posttest
Health promotion
Paracentesis and ascitic fluid analysis
Also called: Abdominal Paracentesis; abdominal tap
Basics the nurse needs to know
A healthy person has less than 50 mL of peritoneal fluid and no distention of the peritoneal (abdominal) cavity. The abnormal condition of accumulated fluid in the peritoneal cavity is called ascites and the fluid is called ascitic fluid. When the ascites is advanced, the fluid volume has dramatically increased. The ascitic fluid can be aspirated by a needle that penetrates into the peritoneal cavity. Laboratory analysis of the fluid specimen includes cytologic study, chemistry analysis, and microbiologic examination, as requested.
REFERENCE VALUES
Ascitic fluid analysis
Appearance: Clear, odorless, colorless or pale yellow, scanty
Microbiology: Bacteria and fungi: None present
Cytology: No malignant cells present
Red blood cells: <103/μL or SI: <1 × 109/L
White blood cells: <500 /μL or SI: <0.5 × 109/L
Neutrophils: <250 /μL or SI: <0.25 × 109/L (or <50% of the white blood cell count)
How the test is done
Paracentesis
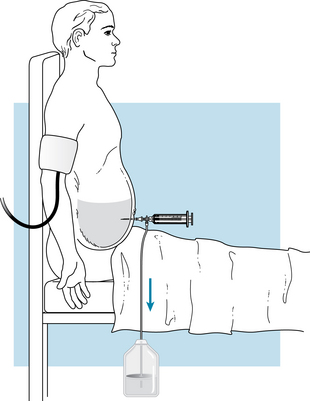
If the physician also wants to drain the peritoneal cavity of a large volume of ascitic fluid for therapeutic purposes, the nurse will assist in connecting sterile IV tubing to the needle or stopcock at one end and a large vacuum container at the other end (Figure 75). Volumes of 4 L or more may be collected.
Interfering factors
NURSING CARE
Pretest
During the test
Posttest
Parathyroid hormone
Also called: (PTH); Parathormone; Immunoreactive PTH
Basics the nurse needs to know
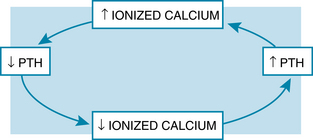
Parathyroid hormone is produced and secreted by the parathyroid glands. Its role in the body is the regulation of calcium. Its secretion is based on a negative feedback mechanism with calcium (Figure 76).
Parathyroid hormone affects calcium levels by stimulating osteoclast activity and inhibiting osteoblast activity in the bone. This causes bone reabsorption, which shifts calcium and phosphate out of the bone into the blood. Parathyroid hormone also causes increased reabsorption of calcium at the kidney’s distal tubules and decreased reabsorption of phosphate at the proximal tubules. The result of parathyroid hormone activity is an increase in calcium in the blood with a decrease in plasma phosphate levels.
Patch test, skin
Basics the nurse needs to know
Allergic contact dermatitis causes an eczematous skin change. It is an inflammatory skin response that occurs when the skin is in contact with a particular antigen. The person is sensitized to the antigen over time, without the immediate development of a skin reaction. Eventually, reexposure to the antigen induces a vigorous allergic response at the site of contact with the antigen.
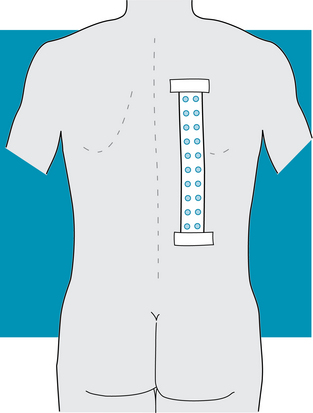
How the test is done
Samples of selected allergens used by the patient or of a number of standard allergens are taped to the patient’s skin for 48 hours of contact exposure (Figure 77). The readings of the results are performed after 48 hours and again after 72 hours to 7 days, as prescribed.
Interfering factors
NURSING CARE
Pretest
Posttest
The nurse instructs the patient to refrain from showers and physical exercise during the following 48 hours. This is because water and perspiration will loosen the tape of the patch. The patient is also told that if itching, irritation, or pain occurs under one of the discs of allergen, it should be removed immediately.
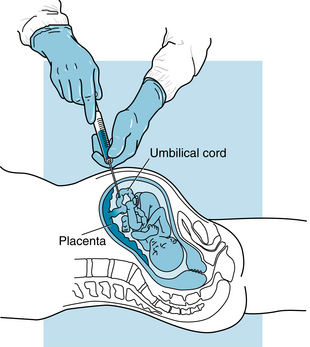
Percutaneous umbilical blood sampling
Also called: PUBS; Cordocentesis
Basics the nurse needs to know
Fetal blood analysis
Prenatal chromosomal analysis
The karyotype consists of the characteristics of the chromosomes, their number, form, size, structure, and grouping. Chromosomal abnormality in the fetus is identified by analysis of the fetal blood cells using chromosomal-specific DNA probes.
Thrombocytopenia
REFERENCE VALUES
Hematologic evaluation: Within normal limits for gestational age
Chromosomal analysis: Normal karyotype
Biochemistry analysis: Within normal limits for gestational age
Immunoglobulin G (IgG) antibodies: Within normal limits
IgM antibodies: Within normal limits
Fetus of 18-20 weeks 11.47 ± 0.78 g/dL or SI: 115 ± 7.8 g/L
Fetus of 21-22 weeks 12.28 ± 0.89 g/dL or SI:123 ± 8.9 g/L
Fetus of 23-25 weeks 12.40 ± 0.77 g/dL or SI: 124 ± 7.7 g/L
Fetus of 26-30 weeks 13.35 ± 1.17 g/dL or SI: 134 ± 11.7 g/L
Fetus of 18-20 weeks 2.66 ± 0.29 × 106 cells/μL or SI: 2.66 ± 0.29 ×12 cells/L
Fetus of 21-22 weeks 2.96 ± 0.26 × 106 cells/μL or SI: 2.96 ± 0.26 ×12 cells/L
Fetus of 23-25 weeks 3.06 ± 0.26 × 106 cells/μL or SI: 3.06 ± 0.26 ×12 cells/L
Fetus of 26-30 weeks 3.52 ± 0.32 × 106 cells/μL or SI: 3.52 ± 0.32 ×12 cells/L
How the test is done
Guided by ultrasound imaging, the physician inserts a sterile 20- to 22-gauge spinal needle through the maternal abdomen and uterus. The needle is then advanced into the umbilical cord until it is placed in one of the umbilical veins (Figure 78). Once the needle placement is verified, a syringe is used to aspirate 0.5 to 3 mL of venous blood. The blood is then transferred to microtubes for specific laboratory analyses.
Interfering factors
NURSING CARE
Pretest
During the test
Posttest
Premature labor.
Premature labor may develop, as characterized by uterine contractions recorded on the fetal monitor. The mother may complain of backache, uterine cramping, or rhythmic contractions. There may be leakage of amniotic fluid from the vagina because of premature rupture of the membranes.
Perfusion studies, cardiac
Interfering factors
NURSING CARE
Pretest
During the test
Pericardiocentesis
Also called: Pericardial fluid analysis
Basics the nurse needs to know
Pericardiocentesis is a diagnostic and therapeutic procedure in which the pericardial space is accessed with a needle or cannula, and fluid is aspirated (Figure 79). For diagnostic purposes, the fluid is then analyzed. For therapeutic purposes, either fluid is drained on a one-time basis or a catheter is inserted and left in place for 1 to 48 hours (rarely, it may be kept in for 72 hours).

Figure 79. Pericardiocentesis.
(From Custalow CB: Color atlas of emergency department procedures, Philadelphia, 2005, Saunders.)
How the test is done
The physician inserts a needle and approximately 20 mL of fluid is removed for analysis. Echocardiography is used to guide the needle into the pericardial sac. See Echocardiography, pp. 270. If cytologic studies are performed, a heparinized container is necessary. The fluid is usually analyzed for color; hemoglobin concentration; hematocrit value; red blood cell, white blood cell, and differential counts; and protein and glucose determinations. In addition, Gram stains and culture, fungal stains and culture, and cytologic studies are performed. Additional fluid is removed if viral and parasite studies, immunologic and serologic screens, or lipoelectrophoresis are planned.
Interfering factors