Chapter 38 OXYGENATION
An adequate supply of blood is necessary for the normal function of every cell. Cells temporarily deprived of blood or oxygen will not function normally, and continued disruption of blood supply causes irreversible damage or cell death. Any disorder that interferes with the distribution or delivery of blood to tissues or the uptake or excretion of gases in respiration is a potential harm to body cells and may have permanent effects on a part, or all, of the body. The most common complication of a respiratory disorder is carbon dioxide retention. This can be a result of alveolar hypoventilation, or a cardiovascular disorder altering the ventilation or the perfusion of the lungs and other tissues.
STRUCTURE OF THE RESPIRATORY SYSTEM
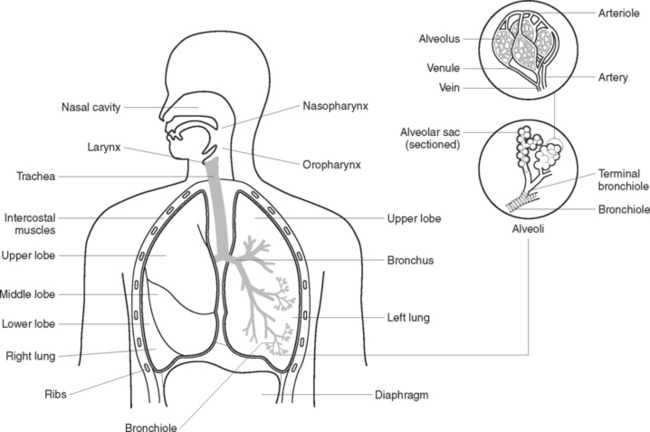
The function of the respiratory system (Figure 38.1) is to deliver oxygen from the atmosphere to the bloodstream and to deliver carbon dioxide from the bloodstream to the atmosphere. The structures that make up the respiratory tract constitute the means by which this exchange of gases occurs. The respiratory system consists of cavities and conducting airways that begin at the nasal and oral cavity and end at the alveoli, the functional unit of the respiratory system. The larger airways are composed of cartilage and smooth muscle that maintain their patency, and are gradually replaced with smooth muscle in the terminal airways, which allow alterations in airway diameter and ventilation. The two lungs are located in the thoracic cavity, encased by a double membrane known as the pleura, and are separated by the mediastinal cavity that contains the heart and great vessels. The thoracic cavity has ribs that aid in ventilation and protect the lungs from damage. The diaphragm and the internal and external intercostal regions are composed of skeletal muscle and constitute the main muscles of ventilation; other muscles are used when required for more forceful inhalation or expiration.
NASAL CAVITIES
THE PHARYNX
THE LARYNX
Voice production
The vocal cords are apart during normal breathing. Contraction of muscles attached to the cords brings them closer together, and expired air is used to cause vibration of the cords. The brain, tongue, lips, nasal cavity and facial muscles all help to convert the resultant sounds into speech. The pitch of the voice depends on the length and tightness of the cords, and the air sinuses in the skull bones influence the resonance of the voice. The vowels and consonants that make up speech are formed by various positions of the lips and tongue. Speaking requires coordination of the larynx, mouth, lips, tongue, throat, lungs and abdomen.
ALVEOLI
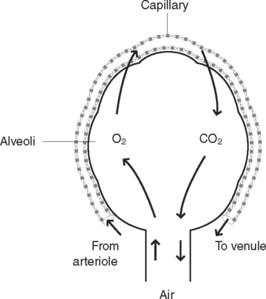
Alveoli are microscopic air sacs in the lungs. Their walls are composed of one layer of type I, simple squamous epithelial cells, and type II cells that produce surfactant that maintain alveolar expansion by reducing surface tension. Macrophages are present and their role is to phagocytose cell debris and pathogens. The alveoli form a surface area of about 70 m2 for semi-permeable membrane diffusion of gases. The alveoli are surrounded by networks of capillaries, arising from the pulmonary arteries and their tributaries. The function of alveoli is the interchange of oxygen and carbon dioxide between the air in the alveoli and the blood in the capillaries (Figure 38.2).
LUNGS
The two lungs lie in the thoracic cavity on either side of the mediastinum. The mediastinal cavity contains the heart, major blood vessels and the oesophagus. The lungs are light and spongy and consist of the bronchioles, alveoli and blood vessels and are supported by areolar tissue. There is also a great deal of elastic tissue to enable the lungs to expand and recoil freely during respiration. The base of each lung rests on the diaphragm and the apex of each extends to just above each clavicle. The right lung has three lobes and is shorter and wider than the left lung, which has two lobes (Figure 38.1). Each lobe is made up of lobules, each with its own blood, nerve and lymph supply. On the medial side of each lung is a depression called the hilus, through which the bronchi, lymphatic vessels and blood vessels enter and exit.
PLEURA
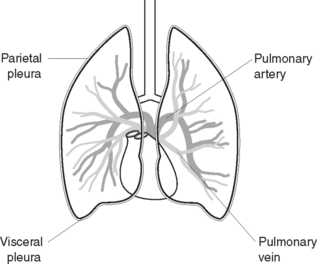
The pleura (Figure 38.3) comprise a double layer of serous membrane, consisting of the visceral pleura, which adheres to the surface of the lungs, and the parietal pleura, which lines the thoracic cavity and covers the superior surface of the diaphragm. The pleura secrete a thin film of serous fluid, maintained at about 50 mL, which lies between the two layers and prevents friction between the surfaces. The pressure within the pleura is 2 mmHg below atmospheric pressure to prevent lung collapse.
SCIENTIFIC PRINCIPLES RELATED TO THE RESPIRATORY SYSTEM
ATMOSPHERIC PRESSURE
The following three laws of physics define the characteristics of gases:
REGULATION OF VENTILATION
PRESSORRECEPTORS
Pressorreceptors, or mechanoreceptors, are stretch receptors present in lung tissue and within the thoracic wall. The bronchioles and alveoli also have stretch receptors that respond to extreme over-inflation as well as extreme deflation. When over-inflation occurs, impulses are transmitted from the stretch receptors to the medulla by the vagus nerve, the expiratory centre is activated and exhalation occurs. When extreme deflation occurs impulses from the lungs activate the inspiratory centre, and inhalation occurs.
VENTILATION AND RESPIRATION
Ventilation
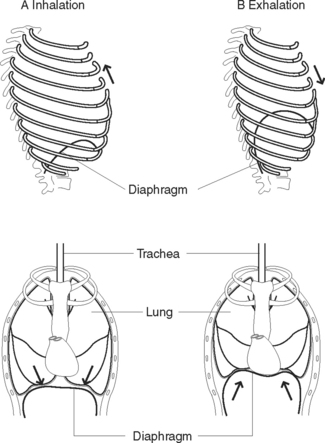
Ventilation has two phases: inhalation and exhalation (Figure 38.4).
Exhalation
Exhalation is normally a more passive process than inhalation except in exercise and respiratory conditions in which active expiration occurs via internal intercostal and accessory muscles. During exhalation the diaphragm relaxes thus decreasing the size of the thoracic cavity. The external intercostal muscles also relax, allowing the ribs and sternum to return to their former position, further decreasing the size of the thoracic cavity. The elastic tissue of the lungs allows for recoil, further forcing air out of the respiratory passages.
Respiration
External respiration
External respiration is the exchange of gases between air in the alveoli, and the blood travelling through the capillaries surrounding the alveoli. Branches of the pulmonary artery bring deoxygenated blood to the capillaries surrounding each alveolus. During gas exchange, gases normally diffuse through the semi-permeable walls of the alveoli and capillaries to the area of lowest concentration of each gas, as each gas diffuses independently of other gases, until the pressure is equal on both sides. Thus, oxygen moves from an area of higher concentration in the alveoli to an area of lower concentration in the blood capillaries, while CO2 moves from an area of a higher concentration in blood capillaries to an area of lower concentration in the alveolar air. Pulmonary venules then collect the blood rich in oxygen from the capillaries and unite to form the two pulmonary veins which leave each lung to enter the left atrium of the heart. Table 38.1 illustrates the concentration and movement of gases in the alveoli and capillary blood. Table 38.2 illustrates the approximate composition of inspired and expired air.
TABLE 38.2 COMPOSITION OF INHALED AND EXHALED AIR (APPROXIMATE)
| Substance | Inhaled air | Exhaled air |
|---|---|---|
| Nitrogen | 78.62% | 74.5% |
| Oxygen | 20.84% | 15.7% |
| Carbon dioxide | 0.04% | 3.6% |
| Water vapour | 0.50% | 6.2% |
| Total | 100.0% | 100.0% |
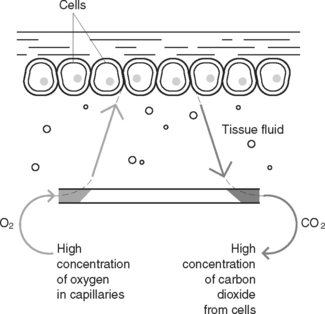
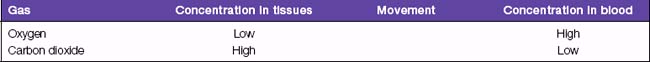
Internal respiration
Internal respiration is the exchange of gases between the bloodstream and the tissues (Figure 38.5). During this exchange, the gases diffuse through the semi-permeable walls of the capillaries to equalise the concentration of gases on both sides. Oxygen moves from the blood into the tissues, down a concentration gradient, to replenish oxygen used in cellular metabolism. Carbon dioxide moves from the tissues into the blood, down a concentration gradient, to rid the tissues of waste produced by cellular metabolism. Table 38.3 illustrates the concentration and movement of gases in the tissues and capillary blood.
STRUCTURE OF THE CARDIOVASCULAR SYSTEM
The structures that make up the cardiovascular system are the:
BLOOD
Constituents of blood
Blood group types
Human blood is grouped into four classifications based on immune reactivity. The groups are O, A, B, AB. The Rhesus factor (either negative or positive) is also determined. Eighty-five percent of the population has Rh antibodies on the surface of the red blood cell (that is RH positive). Generally speaking the blood of any one group is incompatible with the blood group of another. Therefore blood transfusions should be an exact match to the client’s blood group and Rh factor. When blood transfusions occur with mismatched blood a haemolytic reaction can occur (refer to Table 38.4 Preparing and monitoring a client undergoing a blood transfusion) (Tollefson 2004).
TABLE 38.4 PREPARING AND MONITORING A CLIENT UNDERGOING A BLOOD TRANSFUSION
| Review and carry out the steps in Appendix 1 |
| Action | Rationale |
|---|---|
| Check medical orders to ascertain type, frequency and amount of fluid to be administered, and time prepared | Ensures correct quantities are given to client |
| Explain procedure to client | Reduced anxiety/apprehension and gains client’s trust and cooperation |
| Measure and record blood pressure and vital signs | Provides a baseline of the client’s haemodynamic health status |
| Prepare equipment | |
| Wash and dry hands | Prevents cross infection and contamination of blood and tubing |
| Don appropriate equipment and clothing as per infection control guidelines | |
| Gather equipment including: | Ensures all equipment is at |
| Establish an IV infusion with normal saline | IV access is established by a doctor or accredited Registered Nurse (RN). Normal saline is the solution used during a blood transfusion because it is compatible with blood and does not cause red blood cell lysis |
| Identify the client and the blood product according to policy | Group and type of blood product matches on the order and the product |
| Two nurses check the: | |
| The blood transfusion must be initiated within 15 minutes of arrival to the ward | Minimises risk of bacterial infection |
• Wearing gloves, close clamp on saline infusion and attach blood product to the short tubing on the administrating set | Ensures cells and plasma are mixed |
| Initiate the transfusion slowly | Most reactions occur within the first 10 minutes. Beginning the transfusion slowly reduces the amount of blood for the system to react against reducing the severity of the reaction |
| Monitor the client | Vital signs are taken as per facility guidelines. Most are generally taken every 15 minutes for the first hour of the infusion then hourly for the remainder of the infusion |
| Observe for reactions such as: | Signs of a febrile reaction. Slow infusion rate |
| Observe for reactions such as: | |
| Observe for reactions such as: | Signs of a haemolytic reaction |
| Complete the transfusion | Ensures client receives the entire transfusion |
| Dispose of the blood unit as per facility guidelines | Some facilities require all blood units (including the giving set) to be returned to blood bank and kept for 24 hours in case of a delayed reaction |
| Monitor client | Clients can have a delayed reaction to the blood product for up to 24 hours |
| Vital signs are often recorded hourly for 4 hours then 4 hourly for 24 hours | |
| Report and document the procedure and any complications | Most blood products have a peel off identification tag that is identical to the blood unit ID number, grouping and Rh factor so that errors in transcription are avoided. This tab should be removed and placed in the |
BLOOD CELLS
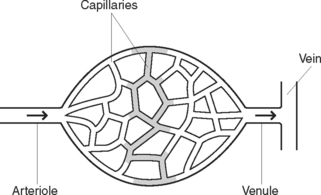
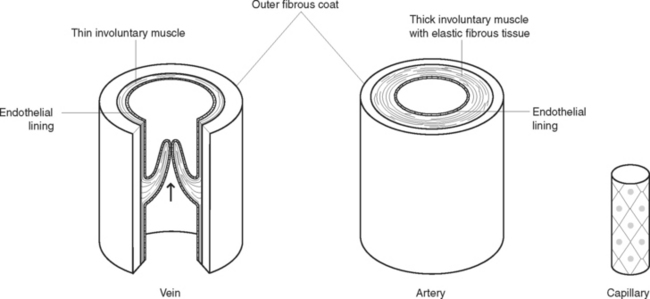
BLOOD VESSELS
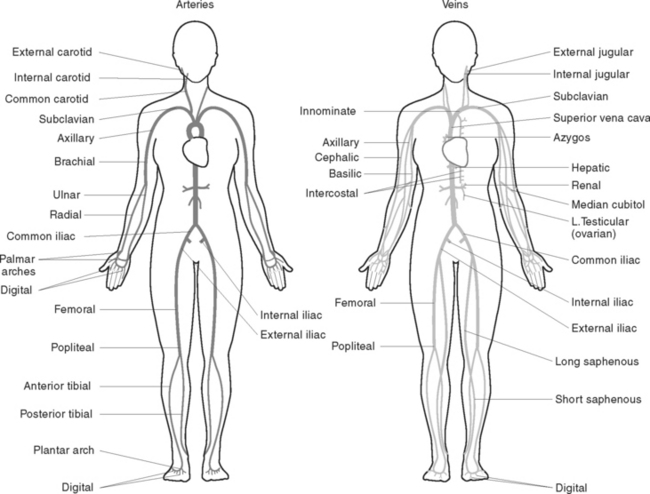
Blood is circulated throughout the body within vessels that form a closed continuous system (Figure 38.6). The walls of blood vessels have three layers: an outer coat of fibrous tissue, a thick middle layer of involuntary muscle with elastic fibrous tissue and an inner lining of endothelium to form a smooth surface for contact with blood (Figure 38.7). Blood vessels include the arteries, veins and capillaries (Figure 38.8).
THE HEART
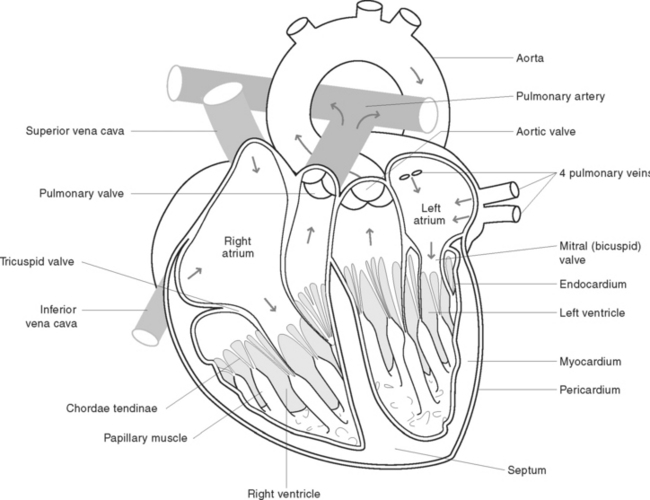
Structure of the heart
The heart is divided into a right, and a left side by a muscular partition called the septum. Each side is further divided into an upper receiving chamber, the atrium, and a lower distributing chamber, the ventricle (Figure 38.9). The walls of the heart consist of the pericardium, myocardium and endocardium:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree