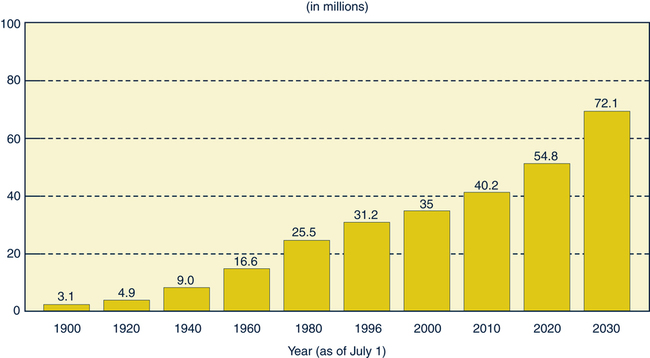
Sue E. Meiner, EdD, APRN, BC, GNP On completion of this chapter, the reader will be able to: 1. Trace the historic development of gerontologic nursing as a specialty. 2. Distinguish the educational preparation, practice roles, and certification requirements of the gerontologic nurse generalist, nurse practitioner, and clinical nurse specialist. 3. Discuss the major demographic trends in the United States in relation to the older adult population. 4. Describe the effects of each of the following demographic factors on the health, well-being, and life expectancy of older adults: 5. Explain why old age is considered a woman’s problem. 6. Describe the effect of functional ability on the overall health status of older adults. 7. Discuss how the “aging of the aged” will affect health care delivery. 8. Explore future trends in gerontologic nursing care along the continuum of care. 9. Explore the concept of ageism as related to the care of older adults in various settings. 10. Identify the issues influencing gerontologic nursing education. 11. Analyze the issues affecting the development and future of gerontologic nursing research. As of 2007, the population of Americans aged 65 or older comprised 37.9 million persons. The number of older adults has grown steadily since 1900, and they are now the fastest growing segment of the population (AOA, 2008). With a “gerontology boom” less than 10 years away, gerontologic nursing is recognized as a specialty. This was not always the case, and the struggle for recognition can be traced back to the beginning of the twentieth century. Burnside (1988) conducted an extensive review of the American Journal of Nursing (AJN) for historical materials related to gerontologic nursing. Between 1900 and 1940, she found 23 writings, including works by Lavinia Dock, with a focus on older adults that covered such topics as rural nursing, almshouses, and private duty nursing, as well as early case studies and clinical issues addressing home care for fractured femur, dementia, and delirium. Burnside discovered an anonymous column in AJN entitled “Care of the Aged” that was written in 1925, and it is now thought to be one of the earliest references to the need for a specialty in older adult care. During World War II and the postwar years (1940 to 1960), the population of older persons steadily increased, but articles about the care of older adults were general and not particularly comprehensive (Burnside, 1988). It was not until 1962, when the geriatric nursing conference group was established during the American Nurses Association (ANA) convention, that the question posed by the anonymous AJN columnist was finally addressed. The years 1960 to 1970 were characterized by many “firsts,” as the specialty devoted to the care of older adults began its exciting development (Table 1–1). Journals, textbooks, workshops and seminars, formal education programs, professional certification, and research with a focus on gerontologic nursing have since evolved. However, the singular event that truly legitimized the specialty occurred in 1969, when a committee appointed by the ANA Division of Geriatric Nursing Practice completed the first Standards of Practice for Geriatric Nursing (ANA, 1991). These standards were widely circulated during the next several years; in 1976 they were revised, and the title was changed to Standards of Gerontological Nursing Practice. In 1981 A Statement on the Scope of Gerontological Nursing Practice was published. The revised Standards and Scope of Gerontological Nursing Practice were published in 1987, 1995, and the current 2010 edition is in press. The changes to this document reflect the comprehensive concepts and dimensions of practice for the nurse working with older adults. In 1995 the revised Scope and Standards of Gerontological Nursing Practice reflected the nature and scope of current gerontologic nursing practice but also incorporated the concepts of health promotion, health maintenance, disease prevention, and self-care. In 2004 all scope and standards of practice were combined into a set of three books known as the Nursing Scope & Standards of Practice, Nursing’s Social Policy Statement (ANA, 2003), and the Code of Ethics for Nurses with Interpretive Statements (ANA, 2001). “These three resources provide a complete and definitive description for better understanding by specialty nursing organizations, policy makers, and the public of nursing practice and nursing’s accountability to the public in the United States” (ANA, 2004, p. vi). This merging of the standards of practice of all the specialties was an effort to outline the expectations of the professional role within which all registered nurses must practice nursing. However, with the tremendous increase in care of the older adult, the ANA has again published Scope and Standards of Gerontological Nursing Practice with input from nurses across the United States before the final publishing in 2010. This document can be obtained from the ANA website: www.nursingworld.org/. TABLE 1–1 DEVELOPMENT OF GERONTOLOGIC NURSING: 1960–1970 Modified from Burnside IM: Nursing and the aged: a self care approach, ed 3, New York, 1988, McGraw-Hill. Another hallmark in the continued growth of the gerontologic nursing specialty occurred in 1973, when the first gerontologic nurses were certified through the ANA. Certification is an additional credential granted by the ANA, providing a means for recognizing excellence in a clinical or functional area (ANA, 1995). Certification is usually voluntary, enabling the nurse to demonstrate to peers and others that a distinct degree of knowledge and expertise has been achieved. In some cases, certification can mean eligibility for third-party reimbursement for nursing services rendered. From the initial certification offering as a generalist in gerontologic nursing, to the first gerontologic nurse practitioner (GNP) examination offering in 1979, to the most recent gerontologic clinical nurse specialist (GCNS) examination (first administered in 1989), this specialty has continued to grow and attract a high level of interest. Eligibility criteria for the application process to take any one of the three certification examinations can be found in Box 1–1. The gerontologic CNS has at least a master’s degree in nursing. The first program was launched in 1966 at Duke University. The gerontologic master’s program typically focuses on the advanced knowledge and skills required to care for older adults in a wide variety of settings, and the graduate is prepared to assume a leadership role in the delivery of that care. GCNSs have an expert understanding of the dynamics, pathophysiology, and psychosocial aspects of aging. They use advanced diagnostic and assessment skills and nursing interventions to manage and improve patient care (American Nurses Credentialing Center [ANCC], 2009). The GCNS functions as a clinician, educator, consultant, administrator, or researcher to plan care or improve the quality of nursing care for older adults and their families. Specialists provide comprehensive care based on theory and research. Today, GCNSs can be found practicing in acute hospitals, long-term care or home care settings, or independent practices. • Geriatrics—from the Greek geras, meaning “old age,” geriatrics is the branch of medicine that deals with the diseases and problems of old age. Viewed by many nurses as having limited application to nursing because of its medical and disease orientation, the term geriatrics is generally not used when describing the nursing of older adults. • Gerontology—from the Greek geron, meaning “old man,” gerontology is the scientific study of the process of aging and the problems of aged persons; it includes biologic, sociologic, psychologic, and economic aspects. • Gerontologic nursing—this specialty of nursing involves assessing the health and functional status of older adults, planning and implementing health care and services to meet the identified needs, and evaluating the effectiveness of such care. Gerontologic nursing is the term most often used by nurses specializing in this field. • Gerontic nursing—this term was developed by Gunter and Estes in 1979 and is meant to be more inclusive than geriatric or gerontologic nursing because it is not limited to diseases or scientific principles. Gerontic nursing connotes the nursing of older persons—the art and practice of nurturing, caring, and comforting. This term has not gained wide acceptance, but it is viewed by some as a more appropriate description of the specialty. Butler (1975), in his classic book, Why Survive? Being Old in America, cautions against using chronologic age as a measure of being old. He offers the following on why age 65 is the discretionary cutoff for defining old age: For several decades, the American Association of Retired Persons (AARP) maintained a yearly update of the profile of older adults in America. This organization is a nonprofit, nonpartisan membership organization for people age 50 or older. The AARP is dedicated to enhancing the quality of life for all Americans as they age. The association acknowledges that its members receive a wide range of unique benefits, special products, and services. Additional information can be found at their website: www.aarp.org. In 1997 the organization stopped compiling profile demographics and began to collect more specific data on a narrower scope. The federal government maintains aging statistics that are available to the public. These publications include an annual chart book with the name of the year. Information can be found at www.agingstats.gov/agingstatsdotnet/Main_Site/Data/2008_Documents/OA_2008.pdf. Use the exact year (e.g., 2010) at the end of the web address for a specific year. This is now a part of public census and reporting efforts. Before review of current statistics of older adults in America, a look at past issues that have lead to these numbers is appropriate. The relatively high birth rate during the late nineteenth and early twentieth centuries accounts in part for the large number of older persons today (Burnside, 1988). Reduced infant and child mortality as a result of improved sanitation, advances in vaccination, and the development of antibiotics has also contributed. The large influx of immigrants before World War I is an additional important factor. The net effect, associated with a reduction in mortality for all ages and fertility rates at a replacement level, has been an increase in the older adult population. Not only are large numbers of persons living to age 65 but they are also living to older ages. When the current figures are validated, the population aged 85 or older is expected to be 5.7 million in 2010 and increase to 6.6 million by 2020. Data obtained in 2007 found that adults 65 or older numbered 3.8 million, which is an increase of 11.2% since 1997. The number of Americans aged 45 to 64, who will reach 65 over the next 20 years, increased by 38% during this past decade. One person in every eight is an older American. That accounts for 12.6% of the United States population (AOA, 2008). See Fig. 1–1 for population trends of persons 65 years or older through 2030.
Overview of Gerontologic Nursing
Foundations of the Specialty of Gerontologic Nursing
History and Evolution
Standards of Practice
YEAR
EVENT
1961
Formation of a specialty group for geriatric nurses is recommended by the American Nurses Association (ANA).
1962
First national meeting of the ANA Conference on Geriatric Nursing Practice is held in Detroit, Mich.
American Nurses’ Foundation receives a grant for a workshop on the aged.
First research in geriatric nursing is published in England (Norton D et al: An investigation of geriatric nursing problems in hospital, London 1962, National Corporation for the Care of Old People).
1966
First gerontologic clinical specialist nursing program is developed at Duke University by Virginia Stone.
Geriatric Nursing Division of the ANA is formed; a monograph is published, entitled Exploring Progress in Geriatric Nursing Practice.
1968
Laurie Gunter is the first nurse to present a paper at the International Congress of Gerontology in Washington, DC. First gerontologic nursing interest group, Geriatric Nursing, is formed.
Barbara Davis is the first nurse to speak before the American Geriatric Society.
First article on nursing curriculum regarding gerontologic nursing is published (Delora JR, Moses DV: Specialty preferences and characteristics of nursing students in baccalaureate programs, Nurs Res March/April, 1969).
The nine standards for geriatric nursing practice are developed.
1970
Standards of Geriatric Nursing Practice is first published.
First gerontologic clinical nurse specialists graduate from Duke University.
Roles
Terminology
Demographic Profile of the Older Population
The Older Population
Highlights of the Profile of Older Americans
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Overview of Gerontologic Nursing
Get Clinical Tree app for offline access