CHAPTER 26
Other Medical Complications
1 Describe the data to be documented in obtaining a history from pregnant patients with cardiac, respiratory, renal, hematologic, gastrointestinal, and hepatic complications.
2 Describe the fetal implications for pregnant patients with medical complications.
3 Describe the signs and symptoms and laboratory data that indicate cardiac, respiratory, renal, hematologic, gastrointestinal, and hepatic complications of pregnancy.
4 Formulate a plan of care consisting of interventions and health education based on nursing history and assessments for the pregnant patient with cardiovascular, respiratory, renal, hematologic, gastrointestinal, and hepatic complications.
5 Design a plan to teach principles necessary for maintenance of health for pregnant patients with cardiac, respiratory, renal, hematologic, gastrointestinal, and hepatic complications.
6 Define specific preconception health education strategies to maximize maternal and fetal outcomes for patients with cardiovascular, respiratory, renal, hematologic, and gastrointestinal complications.
INTRODUCTION
A Women who enter pregnancy with a preexisting disease or a chronic condition are at risk for complications; the disease can complicate the course of pregnancy, or, alternatively, the pregnancy might worsen the disease process.
B Women with medical complications of pregnancy often experience anxiety regarding the effect of the complication on the outcome of the pregnancy.
CLINICAL PRACTICE
1. Discuss patient’s fears and concerns about her pregnancy and its outcome.
a. Provide reassurance and comfort.
b. Encourage patient to ask questions about tests, medications, treatments, and physician orders.
c. Explain all procedures and their purpose.
d. Acknowledge patient’s feelings and respond appropriately to her needs.
2. Maintain clean, orderly, quiet, and stress-free environment.
3. Discuss effects of prolonged hospitalization on the family process.
4. Assess financial burden on family.
5. Assess family members’ level of anxiety and knowledge of disease process; assess them as a support system for patient.
a. Assist family members in reorganizing roles at home and setting priorities to maintain family integrity and to reduce stress.
b. Aid family members in changing and maintaining realistic expectations of the patient.
c. If patient is hospitalized, encourage her friends and family to visit frequently; instruct them about visiting hours.
6. Allow patient and family members to ventilate fears about pregnancy outcome.
7. Prepare patient and her family members for signs of depression, anxiety, and dependency.
8. Assess the patient’s and family’s spiritual needs and help them to meet those needs.
9. Arrange for a tour of special care nursery or for infant special care staff to visit with patient/family as appropriate; orient patient to have realistic expectations for newborn.
10. Encourage patient’s interest in diversional activities (e.g., crafts, books, music).
11. Encourage patient and her family to participate in support groups and education programs.
12. Use additional resources as appropriate.
a. Advanced practice nurses (clinical nurse specialist, nurse practitioner)
d. Lay support and self-help groups
13. Determine patient’s knowledge of her illness, its treatment, and preventive measures.
14. Assess patient and family members’ readiness and ability to learn.
a. Begin patient and family education regarding the disease and its effects on the mother and fetus.
15. Assess patient’s adherence to prescribed treatment regimen and its effect on her lifestyle.
16. Discuss with patient and family signs and symptoms to report.
17. Explain the purpose of treatments, interventions, and tests.
18. Teach patient behavioral interventions and explain physiologic rationale as appropriate to her condition.
a. Bedrest in lateral position
b. Observance of prescribed medication regimen
c. Maintenance of a quiet and stress-free environment as is possible
19. Explain to patient the rationale and procedure for fetal assessment tests such as:
CARDIAC COMPLICATIONS
A Cardiac disease of varying severity occurs in approximately 1% of all pregnancies and is the leading nonobstetric cause of maternal mortality (Cunningham et al, 2001).
B Assessment and management of women with known cardiac disease should begin before conception to optimize the woman’s health and determine the best time for pregnancy (Arafab & McMurtry Baird, 2006; Dobbenga-Rhodes & Privé, 2006)
C The woman’s cardiac problem, functional capacity, exercise tolerance, medication needs, history of arrhythmias, degree of cyanosis, and New York Heart Association (NYHA) classification should be taken into consideration when assessing risk stratification (Arafab & McMurtry Baird, 2006; Blanchard & Shabetai, 2009; Dobbenga-Rhodes & Privé, 2006).
D Pregnancy causes significant alterations in maternal cardiovascular physiology; these hemodynamic changes have a profound effect on pregnant patients with cardiac disease; each of these changes increases cardiac work and might exceed the functional capacity of a diseased heart, resulting in pulmonary hypertension, pulmonary edema, congestive heart failure, or maternal death (Arafab & McMurtry Baird, 2006; Gei & Hankins, 2001); these changes include:
E The risk of maternal mortality associated with specific cardiac lesions is outlined in Box 26-1; the potential for a successful pregnancy is also determined by the functional limitation with which the patient enters pregnancy; those patients entering pregnancy at NYHA functional class I or II usually do well during pregnancy (Cunningham et al, 2001; Sui & Colman, 2001) (Table 26-1); the risk of perinatal and maternal morbidity and mortality associated with cardiac disease during pregnancy depends on:
TABLE 26-1
New York Heart Association Functional Classification of Cardiac Disease
| Class | Description |
| I | Patients with cardiac disease and no limitation of physical activity. Patients in this class neither have symptoms of cardiac insufficiency nor experience pain. |
| II | Patients with cardiac disease and slight limitation of physical activity. They are comfortable at rest, but if ordinary physical activity is undertaken, discomfort results in the form of excessive fatigue, palpitation, dyspnea, or anginal pain. |
| III | Patients with cardiac disease and marked limitation of physical activity. They are comfortable at rest, but less-than-ordinary activity causes discomfort in the form of excessive fatigue, palpitation, dyspnea, or anginal pain. |
| IV | Patients with cardiac disease and inability to perform any physical activity without discomfort. Symptoms of cardiac insufficiency or of the anginal syndrome might occur even at rest, and if any physical activity is undertaken, discomfort is increased. |
1. The specific cardiac lesion
2. The functional abnormality produced by the lesion
3. Development of pregnancy-related complications, such as infection, hemorrhage, or preeclampsia
F Cardiac disease during pregnancy may be categorized as congenital, acquired (rheumatic), or ischemic (Blanchard & Shabetai, 2009; Gei & Hankins, 2001; Wenstrom & Malee, 1999).
a. Is increasing due to advances in diagnosis and treatment, allowing more women with congenital heart defects to survive to reproductive age and achieve a successful pregnancy
b. Includes atrial septal defect, ventricular septal defect, pulmonic stenosis, congenital aortic stenosis, coarctation of the aorta, tetralogy of Fallot, and Eisenmenger syndrome
a. Is mainly rheumatic in origin
b. Incidence of rheumatic heart disease is decreasing, resulting in a decline in rheumatic valvular disease.
c. Includes valvular lesions such as mitral stenosis and aortic stenosis
3. Ischemic cardiac disease (rare in pregnancy)
1. The fetus is at risk for hypoxia because of maternal hypoxemia.
2. The incidence of prematurity, intrauterine growth restriction (IUGR), spontaneous abortion, and stillbirth is increased because of maternal hypoxemia.
3. If the woman has congenital heart disease, there is an increased incidence of fetal congenital cardiac anomalies.
CLINICAL PRACTICE
a. Category of heart disease: congenital, acquired, or ischemic
b. Duration and course of disease
c. NYHA Functional Classification of Cardiac Disease: degree of limitation of physical activity
e. Response to previous pregnancies
a. Vital signs: blood pressure and apical/radial pulse
b. Signs and symptoms of heart disease; Table 26-2 lists the signs and symptoms common to normal pregnancy compared with those of actual heart disease
TABLE 26-2
| Normal Pregnancy | Actual Cardiac Disease |
| Chest discomfort | Chest discomfort with myocardial ischemia |
| Dyspnea | Severe dyspnea that limits activity; paroxysmal nocturnal dyspnea |
| Orthopnea | Progressive orthopnea |
| Palpitations | Cardiac arrhythmia |
| Easy fatigability | Fatigue with chest pain and syncope |
| Dizzy spells | Dizzy spells plus other actual signs and symptoms |
| Syncope | Syncope with exertion |
| Systolic murmurs | Loud, harsh, systolic murmurs: grade III intensity, diastolic murmurs |
| Dependent edema | Dependent plus nondependent edema |
| Rales in lower lung fields | Rales that do not clear with deep inspiration; hemoptysis |
| Visible neck veins | Persistent neck vein distention |
| Cardiomegaly | Cardiomegaly plus hepatomegaly and ascites |
c. Signs and symptoms of cardiac decompensation (Gilbert, 2007)
(1) Dyspnea severe enough to limit usual activity
(3) Paroxysmal nocturnal dyspnea
(4) Syncope during or immediately following exertion
(5) Chest pain associated with activity
d. Signs and symptoms of congestive heart failure (CHF)
e. Laboratory and diagnostic studies
1. Assess for risk of decreased cardiac output related to structural defects, CHF, or pulmonary edema.
a. Monitor for signs and symptoms of decreased cardiac output (Carpenito, 1997).
2. Teach patient to avoid stress and anxiety.
3. Instruct the patient in following a low-sodium diet to prevent fluid retention.
4. Monitor weight gain; encourage patient to avoid excessive weight gain, which causes increased cardiac workload.
5. Counsel patient to avoid physical exertion and encourage frequent rest periods in left lateral recumbent position.
6. Encourage patient to obtain 8 to 10 hours of sleep per night and to take frequent rest periods during the day.
7. Assist patient with activities of daily living (ADL) and ambulation as necessary, or refer to appropriate social services for help with household responsibilities, as needed.
8. Administer cardiovascular medications as ordered; evaluate the patient’s response to medication (Table 26-3 lists cardiovascular drugs used during pregnancy).
TABLE 26-3
Cardiovascular Drugs Used during Pregnancy
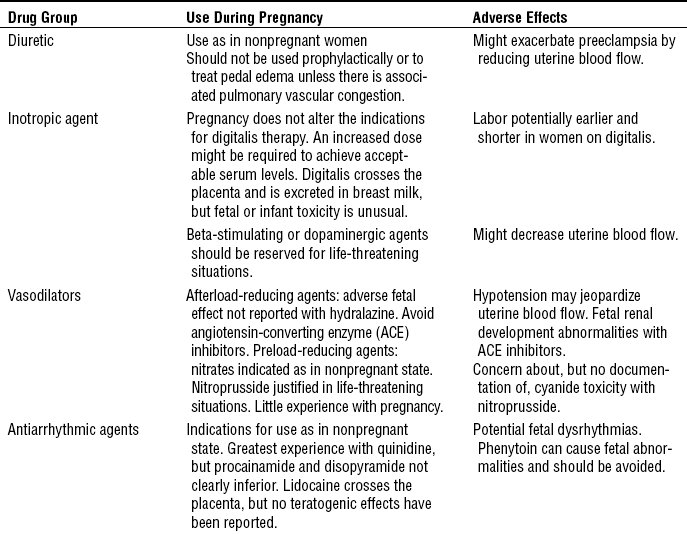
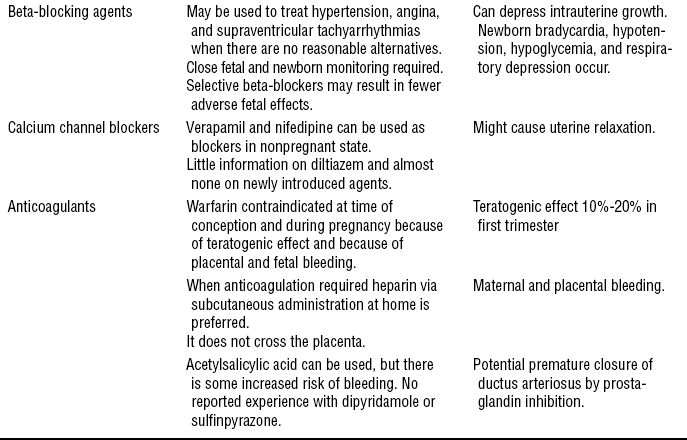
From Burrow, G., & Ferris, T. (1995). Medical complications during pregnancy (4th ed., p. 134). Philadelphia: Saunders.
9. Provide nutritional counseling, encourage high-iron foods, and administer iron and vitamin supplements as ordered to prevent anemia.
a. Iron and folic acid supplements are frequently needed, and hemoglobin and hematocrit levels should be carefully monitored.
10. Monitor for infection related to increased risk due to bacterial invasion, pulmonary congestion, or invasive procedures.
a. Teach the patient to recognize the signs and symptoms of infection.
b. Caution the patient to avoid exposure to infection.
c. Antibiotic prophylaxis is frequently used to prevent bacterial endocarditis.
d. Use strict aseptic technique during invasive procedures.
11. Assess for signs and symptoms of thromboembolism (Carpenito, 1997).
a. Diminished or absent peripheral pulses
b. Unusual warmth and redness or coolness and cyanosis
d. Sudden severe chest pain, increased dyspnea, and tachypnea
12. Anticoagulant therapy (usually heparin) and monitoring of blood coagulation laboratory results to detect any preliminary indications or risk of abnormal bleeding
13. Encourage patient to labor in lateral position; avoid lithotomy position during second stage of labor.
14. Provide effective pain control during labor and delivery to decrease cardiac workload.
15. Encourage gentle pushing to avoid erratic venous return associated with Valsalva effect.
16. Assess hemodynamic function and cardiac output during the intrapartum period and after delivery by implementing hemodynamic monitoring as ordered (e.g., cardiac monitor, arterial line, central venous pressure catheter, pulmonary artery catheter).
17. Monitor intake and output carefully, and regulate intravenous (IV) fluids with an infusion pump to prevent fluid overload and possible pulmonary edema.
HEALTH EDUCATION
1. Discuss the risk of pregnancy to the mother and the risks to the fetus.
2. Discuss potentially teratogenic cardiovascular drugs.
3. Discuss the advances that have improved the outcome for women with cardiac disease in:
B Discuss the importance of early, regular, and frequent medical supervision and encourage patient to be in the care of an obstetrician and a cardiologist.
C Discuss the importance of a multidisciplinary team including cardiology, obstetrics, nursing, dietary, social service, and pediatrics/neonatology.
D Teach patient about rationale for modifying her diet and activities and for taking prescribed medications.
E Teach patient to limit exposure to infection.
F Discuss the importance of obtaining antibiotic prophylaxis before dental and surgical procedures.
G Teach patient to get adequate rest with frequent rest periods and to restrict activity to that which is just short of fatigue.
H Assist patient to modify diet as prescribed.
I Teach patient to avoid excessive weight gain.
J Teach patient to maintain normal hemoglobin levels by eating increased amounts of high-iron and folic-acid–containing foods and taking supplements if needed.
K Teach patient to report signs and symptoms of cardiac decompensation.
L Discuss other topics as appropriate (Arafab & McMurtry Baird, 2006).
RENAL COMPLICATIONS
A Anatomic and physiologic changes that occur in the kidney during pregnancy include:
1. Marked dilation of the collecting system
2. Stasis of urine in the upper part of the collecting system
4. Increase in renal plasma flow
5. Increase in glomerular filtration rate (GFR)
6. Changes in tubular reabsorption of glucose and amino acids so glycosuria and aminoaciduria are normal in pregnancy
7. Decrease in blood urea nitrogen (BUN) and serum creatinine
9. Increased uric acid filtration and secretion, leading to decreased levels of uric acid (Thorsen, 2002)
B Renal disease during pregnancy falls into two categories: new onset of renal disease during pregnancy and chronic renal disease.
1. New onset of renal disease during pregnancy
(1) Approximately 4% to 10% of all pregnant women have asymptomatic bacteriuria, and if untreated, 25% to 40% will experience pyelonephritis; acute pyelonephritis affects 1% to 3% of pregnancies (Cunningham et al, 2001; Wenstrom & Malee, 1999; Williams & Davidson, 2009).
(2) Escherichia coli is responsible for more than 80% of infections.
b. Acute nephrolithiasis (renal stones) occurs in 1 of every 1000 deliveries.
(1) Incidence of 1 in 10,000 pregnancies
(2) Multiple causes are categorized as:
(a) Women with preexisting renal disease
(b) Consequences of pregnancy-associated event
(c) Consequences of a nonpregnant event (i.e., trauma) (Thorsen, 2002)
(3) Most common cause is severe preeclampsia or following hemorrhagic shock.
a. Chronic renal disease in pregnancy is uncommon, with the incidence of moderate to severe chronic renal disease estimated to be less then 1 in 1000 pregnancies (Ramin, Vidaeff, Yeomans, & Gilstrap, 2006).
b. There are multiple causes of chronic renal disease each with its own pathophysiologic mechanisms.
c. The degree of renal function impairment appears to be the most important determinant for pregnancy outcome. In patients with mildly impaired renal function, pregnancy does not usually accelerate renal damage (Cunningham et al, 2001; Ramin et al, 2006).
d. Fetal outcomes are related to maternal renal function impairment and underlying disease (Vidaeff, Yeomans, & Ramin, 2008).
e. Preexisting hypertension along with the degree of renal insufficiency are predictive of pregnancy outcome; hypertension is an indicator of poor pregnancy outcome (Ramin et al, 2006).
f. Patients with renal transplants can sustain a pregnancy; pregnancy should not be considered for 2 years following implantation of a cadaver kidney, or 1 year after a live donor kidney, with the understanding that continuation of immunosuppressive therapy is essential (Thorsen, 2002).
C Adverse consequences of pregnancy in renal disease
CLINICAL PRACTICE
a. Incidence of urinary tract infections (UTIs)
b. Incidence and duration of acute and/or chronic renal disease
c. History of medical conditions associated with acute renal failure
b. Signs and symptoms of pyelonephritis
c. Signs and symptoms of fluid overload and systemic vascular resistance
d. Neurologic signs and symptoms of rapid onset acute renal failure
e. Laboratory and diagnostic tests for renal disease
(a) Proteinuria: indicates glomerular damage
(b) Hematuria: red cell casts indicate glomerular inflammation and injury
(2) Urine culture and sensitivity
(9) Intravenous pyelography (IVP)
(11) Arterial blood gases as indicated
1. Monitor for risk for infection related to anatomic and physiologic changes of the renal system in pregnancy.
a. Monitor for signs and symptoms of infection (UTI or pyelonephritis).
b. Administer antibiotics as ordered.
c. Maintain adequate hydration; encourage oral intake, and if necessary, administer IV fluids as ordered.
d. Assess for maternal bacteremia via blood culture.
e. Assess for maternal septic shock by monitoring vital signs for tachycardia and hypotension.
f. Monitor for contractions and other signs and symptoms of preterm labor.
2. Monitor fluid volume related to inability of the kidney to regulate fluid balance.
3. In chronic renal disease monitor for signs and symptoms of improvement or deterioration in renal status by observing the following parameters:
b. Kidney function tests: serum creatinine, BUN, uric acid, and creatinine clearance
h. Dependent edema and sacral edema
j. Skin turgor, color, and temperature
4. Position in left lateral position when on bedrest.
5. Administer prescribed medications (e.g., antihypertensives).
6. Maintain prescribed sodium restrictions.
7. Adjust the patient’s daily fluid intake as ordered, and distribute fluid intake fairly evenly throughout the day.
8. Observe for signs and symptoms of superimposed preeclampsia.
9. Observe for signs and symptoms of renal insufficiency (Carpenito, 1997).
b. Increased serum creatinine; decreased creatinine clearance
j. Electrolyte imbalance (sodium, potassium, calcium, phosphorus, magnesium)
l. Urine output less than 30 mL/hr
10. Monitor for signs and symptoms of metabolic acidosis.
11. Consult with dietitian for an appropriate diet.
12. Monitor for impaired comfort related to bladder spasm or renal colic; risk for renal calculi
13. Monitor for signs and symptoms of calculi.
14. Strain urine for calculi as indicated.
15. Instruct the patient to increase fluid intake, if not contraindicated.
16. Assess pain-precipitating factors, and document deviation from baseline.
17. Have patient evaluate pain intensity on a 1 to 10 scale (10 being most severe).
18. Provide and encourage rest periods and a restful environment.
19. Medicate patient with analgesics, antispasmodics, and antibiotics as ordered.
21. Teach patient and her family about factors that contribute to pain experience.
22. Assess patient’s urgency and frequency of urination and nocturia.
23. Palpate patient’s bladder for distention.
24. Provide preoperative and postoperative care if surgery is required for ureteral obstruction.
HEALTH EDUCATION
1. Discuss increased risk of fetal loss and preeclampsia with patients already demonstrating proteinuria and hypertension.
2. Discuss increased incidence of anovulation, menstrual irregularities, loss of libido, and decreased fertility among patients with underlying chronic renal disease.
3. Discuss effects of pregnancy on progression of chronic renal disease.
B Teach patient self-monitoring of weight gain, edema, and blood pressure.
C Teach patient to avoid exposure to infection.
D Educate patient regarding prophylactic antibiotic therapy.
E Discuss increased risk of anemia and fluid imbalance, and the importance of adequate nutrition and compliance with prescribed diet and fluid intake.
F Teach patient to recognize and report signs of fluid and electrolyte imbalance and superimposed preeclampsia.
G Discuss the importance of early, regular, and frequent medical supervision, and encourage patient to be in the care of an obstetrician and nephrologist.
H Discuss the importance of a multidisciplinary team including nephrology, obstetrics, nursing, dietary, social service, and pediatrics/neonatology.
I Teach proper front-to-back perineal hygiene.
J Teach all women to recognize and report the symptoms of UTI.
K Teach patient signs and symptoms of premature labor and increased uterine irritability and when to report.
RESPIRATORY COMPLICATIONS
Pulmonary diseases have become more prevalent in the general population and therefore in pregnant women. Normal physiologic changes of pregnancy can cause a woman with a history of compromised respirations to decompensate. The outcome of a pregnant woman with respiratory complications depends on the adequacy of ventilation and oxygenation as well as early detection of decompensation. Hypoxia is the major fetal threat.
1. Asthma is the most common form of lung disease that can affect pregnancy and its affects approximately 4% to 8% of pregnancies (Murdock, 2002; National Asthma Education and Prevention Program [NAEPP], 2007; Rey & Boulet, 2007).
2. Asthma is a reversible syndrome characterized by varying degrees of airway obstruction, bronchial hyperresponsiveness, and bronchial edema (Dombrowski & Schatz, 2008; Wendel, 2001).
3. Well-controlled asthma during pregnancy allows women to continue a normal pregnancy with little or no increased risk to their health or that of their fetuses (Murdock, 2002; Whitty & Dombrowski, 2009).
4. Pregnancy has variable effects on the course of asthma with a third each becoming worse, improving, or remaining unchanged; the course of asthma in a previous pregnancy predicts the course in a subsequent pregnancy in approximately 60% of women; typically the more severe the disease, the more likely it is to worsen (Cunningham et al, 2001; Murdock, 2002; Wenstrom & Malee, 1999).
5. The goal of asthma therapy during pregnancy is to prevent maternal hypoxic episodes and maintain adequate oxygenation of the fetus.
6. Arterial blood gases should be interpreted according to normal values for pregnancy.
7. Asthma should be as aggressively treated during pregnancy as at any other time because the benefits of asthma control far outweigh the risks of medication usage. The National Asthma Education and Prevention Program (NAEPP, 2007) found that it is safer to treat pregnant women with asthma medications than to allow these women to have symptoms and exacerbations.
8. Virtually all of the commonly used asthma medications are considered safe during pregnancy; however, data are scarce on the safety of leukotriene modifiers in pregnancy (NAEPP, 2007; Rey & Boulet, 2007).
9. Asthma in pregnancy is associated with an increase in:
10. Treatment of asthma is based on four management components (NAEPP, 2007):
a. Assessment and monitoring of asthma signs and symptoms, including pulmonary function studies
b. Avoidance of triggers and other factors contributing to asthma severity
c. Pharmacologic therapy using the stepwise approach
11. Goals of therapy and special considerations in pregnant women with asthma include (NAEPP, 2007):
a. Optimal control of asthma symptoms, including nocturnal symptoms
b. Maintain normal or near normal pulmonary function.
c. Manage exacerbations aggressively.
d. Avoid delay in diagnosis and treatment.
e. Assess medication needs and response to therapy frequently and avoid adverse effects from asthma medications.
f. Assess for rhinitis, gastric reflux, and other comorbidities.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


