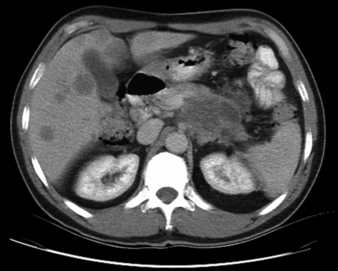
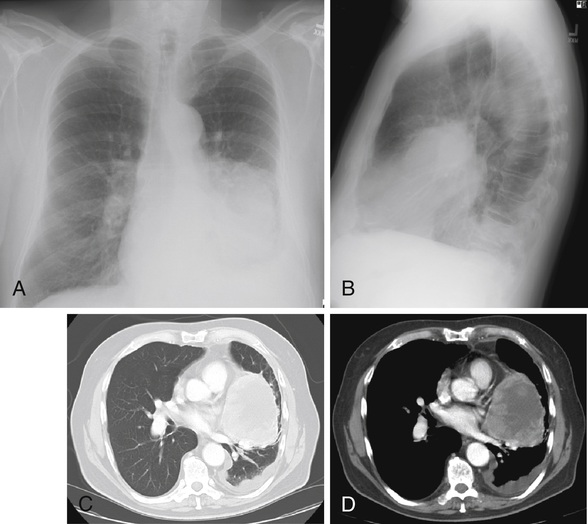
Metastatic cancer (Fig. 26-4). On the Step 2 examination, do not assume that the question is looking for the most common primary cancer unless the word “primary” is specified. CNS, Central nervous system; GI, gastrointestinal; MEN, multiple endocrine neoplasia. ∗The factor with the greatest impact is listed first. As with all cancers, you need a tissue biopsy (e.g., via bronchoscopy, computed tomography [CT]-guided biopsy, open lung biopsy) to confirm malignancy and to define the histologic type. Non–small cell lung cancer may be treated with surgery if the cancer remains within the lung parenchyma (i.e., without involvement of the opposite lung, pleura, chest wall, spine, or mediastinal structures). Early metastases of small cell lung cancer make surgery inappropriate. Small cell lung cancer and extensive non–small cell lung cancer (Fig. 26-6) are treated with chemotherapy with or without radiation. Usually a platinum-containing chemotherapy regimen (e.g., cisplatin) is used. Superior vena cava syndrome: Caused by compression of superior vena cava with impaired venous drainage. Look for edema and plethora (redness) of the neck and face (Fig. 26-7; Plate 59) and central nervous system (CNS) symptoms (headache, visual symptoms, and altered mental status). Hoarseness: From recurrent laryngeal nerve involvement (apical tumor not required).
Oncology
1 What are the key differential points for the commonly tested blood dyscrasias?
TYPE
AGE
WHAT TO LOOK FOR IN CASE DESCRIPTION/TRIGGER WORDS
ALL
Children (peak age: 3-5 yr)
Pancytopenia (bleeding, fever, anemia), history of radiation therapy, Down syndrome
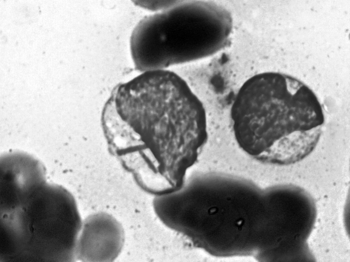
AML
>30 yr
Pancytopenia (bleeding, fever, anemia), Auer rods (Fig. 26-1; Plate 55), DIC
CML (Fig. 26-2; Plate 56)
30-50 yr
White blood cell count greater than 50,000, Philadelphia chromosome, blast crisis, splenomegaly
CLL
>50 yr
Male gender, lymphadenopathy, lymphocytosis, infections, smudge cells, splenomegaly
Hairy cell leukemia
Adults
Blood smear (hairlike projections), splenomegaly
Mycosis fungoides/Sézary syndrome
>50 yr
Plaquelike, itchy skin rash that does not improve with treatment, blood smear (cerebriform nuclei known as “butt cells”), Pautrier abscesses in epidermis
Burkitt lymphoma (Fig. 26-3; Plate 57)
Children
Associated with EBV (in Africa)
CNS B-cell lymphoma
Adults
Seen in patients with HIV infection, AIDS
T-cell leukemia
Adults
Caused by HTLV-1 virus
Hodgkin disease
15-34 yr
Reed-Sternberg cell, cervical lymphadenopathy, night sweats
Non-Hodgkin lymphoma
Any age
Small follicular type has best prognosis, large diffuse type has worst; primary tumor may be located in GI tract
Myelodysplasia/myelofibrosis
>50 yr
Anemia, teardrop cells, “dry tap” on bone marrow biopsy, high MCV and RDW; associated with CML
Multiple myeloma
>40 yr
Bence-Jones protein (IgG = 50%, IgA = 25%), osteolytic lesions, high serum calcium
Waldenström macroglobulinemia
>40 yr
Hyperviscosity, IgM spike, cold agglutinins (Raynaud phenomenon with cold sensitivity)
Polycythemia vera
>40 yr
High hematocrit/hemoglobin, pruritus (especially after hot bath or shower); use phlebotomy
Primary thrombocythemia
>50 yr
Platelet count usually greater than 1,000,000; may have bleeding or thrombosis


5 What is the most common cancer in most organs?
7 Name the mode of inheritance and types of cancer found in the following conditions
DISEASE/SYNDROME
INHERITANCE
TYPE OF CANCER (IN ORDER OF MOST LIKELY)/OTHER INFORMATION
Retinoblastoma
Autosomal dominant
Retinoblastoma, osteogenic sarcoma (later in life)
MEN, type I
Autosomal dominant
Parathyroid, pituitary, pancreas (islet cell tumors)
MEN, type IIa
Autosomal dominant
Thyroid (medullary cancer), parathyroid, pheochromocytoma
MEN, type IIb
Autosomal dominant
Thyroid (medullary cancer), pheochromocytoma, mucosal neuromas
Familial polyposis coli
Autosomal dominant
Hundreds of colon polyps that always become cancer
Gardner syndrome
Autosomal dominant
Familial polyposis plus osteomas and soft tissue tumors
Turcot syndrome
Autosomal dominant
Familial polyposis plus CNS tumors
Peutz-Jeghers syndrome
Autosomal dominant
Look for perioral freckles and multiple noncancerous GI polyps; increased incidence of noncolon cancer (stomach, breast, ovaries); no increased risk of colon cancer
Neurofibromatosis, type I (Fig. 26-5; Plate 58)
Autosomal dominant
Multiple neurofibromas, café-au-lait spots; increased number of pheochromocytomas, bone cysts, Wilms tumor, leukemia
Neurofibromatosis, type II
Autosomal dominant
Bilateral acoustic neuromas
Tuberous sclerosis
Autosomal dominant
Adenoma sebaceum, seizures, mental retardation, glial nodules in brain; increased renal angiomyolipomas and cardiac rhabdomyomas
Von Hippel-Lindau disease
Autosomal dominant
Hemangioblastomas in cerebellum, renal cell cancer; cysts in liver and/or kidney
Xeroderma pigmentosa
Autosomal recessive
Skin cancer
Albinism
Autosomal recessive
Skin cancer
Down syndrome
Trisomy 21
Leukemia

9 Cover the right-hand column and specify the major environmental risk factors for the following cancers
CANCER TYPE
ENVIRONMENTAL RISK FACTORS∗
Lung
Smoking, asbestos (also nickel, radon, coal, arsenic, chromium, uranium)
Mesothelioma
Asbestos and smoking
Leukemia
Chemotherapy/radiotherapy, other immunosuppressive drugs, benzene
Bladder
Smoking, aniline dyes (rubber and dye industry), schistosomiasis (in immigrants)
Skin
Ultraviolet light exposure (e.g., sun), coal tar, arsenic
Liver
Alcohol, vinyl chloride (liver angiosarcomas), aflatoxins (Africa)
Oral cavity
Smoking, alcohol
Pharynx/larynx
Smoking, alcohol
Esophagus
Smoking, alcohol
Pancreas
Smoking
Renal cell
Smoking
Stomach
Alcohol, nitrosamines/nitrites (from smoked meats and fish)
Clear cell cancer†
In utero exposure to diethylstilbestrol (DES)
Colon/rectum
High-fat and low-fiber diet, smoking, alcohol, obesity
Breast
Chest radiation, hormone replacement therapy, alcohol
Cervix
Sex/HPV infection, smoking, high parity
Thyroid
Childhood neck or chest irradiation, low dietary iodine
Endometrium
Unopposed estrogen stimulation, obesity, tamoxifen, high fat diet
All cancer overall
Smoking (number two is probably alcohol)
11 How do you diagnose and treat lung cancer?
12 What consequences can result from an apical (Pancoast) lung cancer?

17 What classic signs and symptoms indicate that a breast mass is cancer until proved otherwise?
 Fixation of the breast mass to the chest wall or overlying skin
Fixation of the breast mass to the chest wall or overlying skin
 Satellite nodules or ulcers on the skin
Satellite nodules or ulcers on the skin
 Matted or fixed axillary lymph nodes
Matted or fixed axillary lymph nodes
 Inflammatory skin changes (red, hot skin with enlargement of the breast caused by inflammatory carcinoma)
Inflammatory skin changes (red, hot skin with enlargement of the breast caused by inflammatory carcinoma)
 Prolonged unilateral scaling erosion of the nipple with or without discharge (may be Paget disease of the nipple)
Prolonged unilateral scaling erosion of the nipple with or without discharge (may be Paget disease of the nipple)
 Microcalcifications on mammography
Microcalcifications on mammography
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access


