Chapter 14 Oncological Diseases
When you have completed this chapter you will be able to
INTRODUCTION
GLOSSARY OF TERMS
This chapter requires familiarity with the following terms:
WHAT IS CANCER?
THE CELL CYCLE
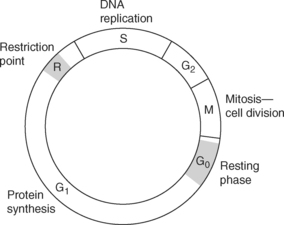
At any one time, most cells in the body are not dividing (the Go phase of the cell cycle), (see Figure 14.1).
Cells, however, can be stimulated to enter a cycle of division by growth factors or hormones. This ultimately results in the cell dividing into two daughter cells, each of which contains an identical copy of the DNA of the original cell. There are several phases to this cell cycle1. The first (G1 or Gap 1 phase) is a time where proteins and ribonucleic acid are synthesised in preparation for the replication (the process of duplicating or reproducing) of the DNA. At the end of this phase is a checkpoint or restriction point (R), which determines whether a cell will enter the next phase of the cycle, the S phase. This next phase is where the replication of the DNA occurs. There follows a second gap (G2) in preparation for the mitotic phase (M). This second gap has a checkpoint to determine whether the cell will enter the mitotic phase. The mitotic phase is where a spindle of fibrin monomers (material resulting from the action of thrombin on fibrinogen) is formed which draws a copy of the duplicated sets of chromosomes to opposite sides of the cell in preparation for forming two daughter cells. Progression through the cell cycle depends on multiple factors, for example, proteins called cycline dependent kinases control the transitions through the cell cycle.
ONCOGENES
Oncogene translates as ‘cancer causing gene’2. Why would the body have genes that cause cancer? There are normal genes in the body called proto-oncogenes. The products of these genes regulate the cell proliferation and growth and these genes are closely regulated. Oncogenes can be turned on because of a mutation in a proto-oncogene or a virus inserting an oncogene into the cell. Products of oncogenes behave abnormally, or are over-expressed and cause cells to divide independently of the normal body signals. Oncogene products can act in the cytoplasm of the cell to disrupt the signalling of growth factors or in the nucleus to alter the control of transcription of genes.
GROWTH FACTORS
Growth factors are signals that reside outside the cell and many are products of oncogenes. To impact on cell function, growth factors have to attach to a receptor (like a key fitting into a lock) that straddles the membrane of a cell and activates transmembrane proteins called tyrosine kinases. Activation of these proteins initiates a cascade, enabling the signal to travel from the outside of the cell, through the cytoplasm of the cell to the DNA in the nucleus of the cell, where the reading of genes and the duplication of DNA are controlled. This flow of information is called signal transduction. Having a receptor activated by a growth factor can cause proliferation of a cell or differentiation, or migration of the cell, or confer protection from programmed cell death and sometimes even growth arrest. These signalling pathways are not just single events but multiple paths interacting with each other, and the outcomes can differ, depending on the duration and intensity of the signals and the cooperation between pathways3. This creates some overlap in signalling pathways, which explains why a minimum of 4 or 5 hits on oncogenes or tumour suppressor genes (which code for the growth factors, their receptors and the signal transducers) are needed to disrupt the normal regulation of cell function which then leads to cancer.
TUMOUR GROWTH
Theoretically, a cancer cell population that keeps dividing into two daughter cells will exhibit exponential growth, with doubling of the cell population after every cycle. If this were the case, after 30 cycles from each cell, there would be 230 (109) cells or 1 gram (or 1 cm3) of tissue. This is the minimal size for detection of a tumour on current scanning machines. Only ten more doublings would produce 1012 cells or 1 kg tissue, which could be lethal. However, since some cells will die if a tumour outgrows its blood supply and some will differentiate into non-dividing cells so the rate of growth will not be as rapid. In fact, the peak growth rate of a tumour occurs just before it is clinically detectable and then slows down. This pattern produces what is known as a Gompertzian growth curve, where the growth fraction (the number of dividing cells) of the tumour declines over time4.
ANGIOGENESIS
A tumour could not grow beyond 2–3 mm2 without new blood vessels growing to provide it with nutrients. Angiogenesis is the growth of new blood vessels from existing vessels and occurs during processes such as the healing of wounds. Cancer cells can produce angiogenic factors (such as vascular endothelial growth factor and basic fibroblast growth factor) that stimulate the formation of new blood vessels. These are balanced with anti-angiogenic factors (such as angiostatin and endostatin)5.
METASTASES
One of the features of cancer is its ability to spread from one part of the body to another6. One way that tumours can cause problems is to directly invade from the primary site into surrounding tissues. Cancer cells can also travel via the blood vessels or via lymphatic vessels which are drainage channels between lymph nodes but also connect with the blood vessels. Another route of tumour invasion is transcoelomic spread, where cancer cells can invade the peritoneal cavity or pleural space.
For tumours to spread, the cancer cells must be able to detach themselves from each other. This is regulated through adhesion proteins (cadherins) on the cells’ surfaces which then attach to the membrane separating them from the adjacent extracellular matrix where they want to go. This basement membrane is a scaffold with collagen fibres containing proteins such as laminins and a coating of fibronectin. The cancer cells bind to these fibres in preparation for breaking through. There are many adhesion molecules, such as immunoglobulin adhesion molecules, intergrins and selectins, which all take part in regulating the binding of cells to each other and to the extracellular matrix through which they must move. Cancer cells move through the matrix in response to chemicals in the tissues which attract them or which they produce themselves in order to move independently. The cells move by a series of adhesion and release of the surrounding tissues. They can move into blood and lymph vessels or directly into adjacent organs.
WHAT CAUSES CANCER?
In the chain of events that results in cancer, the initiating event may be a change in a single gene in a cell. A person can inherit a defective gene. An example is the discovery that inherited mutations in the BRCA 1 or 2 genes (breast cancer 1 and 2 genes) make women susceptible to developing breast cancer7. Carcinogens can also come from the environment, such as the cancer causing agents found when tobacco is burned. In the early stages a cell may not be cancerous, but other agents may promote the process by causing the altered cells to form lumps (such as occurs with polyps in the bowel) which progressively become larger and more abnormal. The agents that promote this change may be viruses or chemicals or even hormones in the case of breast and prostate cancer. Eventually, the pre-cancerous cells will become malignant, either by loss of genes when dividing or further exposure to tumour-promoting agents. Not all damage to the DNA results in the eventual development of cancer, as sometimes, cells can repair the DNA before becoming cancerous. We see then that cancer is caused if a cell is genetically susceptible, perhaps because of inheriting a mutated gene and then, either further mistakes occur when it divides, or agents in the environment trigger the cell to become malignant over time.
AGENTS THAT CAUSE CANCER
In our environment, there are many agents that can cause cancer. These have been discovered by studying large populations of people or in instances where rare cancers cluster together and have in common exposure to a particular agent. Here we will look at the more common cancer causing agents8.
ALCOHOL
In combination with smoking, heavy alcohol intake has been implicated in the development of head and neck cancer. It can also cause liver damage that will lead to liver cancer and may have a smaller role among other factors for common cancers, such as breast cancer.
HORMONES
Over-stimulation of hormone-sensitive organs such as the breast or endometrium may promote cancer in those where a gene mutation is already present. Sometimes, these may be greater production of hormones or from taking hormone medications.
HOW ARE CANCERS DETECTED?
NURSING IMPLICATIONS
A diagnosis of cancer is likely to be a traumatic event for the person concerned, as well as for their family and friends. While the word ‘cancer’ can be simply defined as an abnormal proliferation of cells, as previously explained cancer can actually be more than a hundred different diseases, depending on the cells and organs affected. More importantly however, the meaning of the word cancer can be interpreted in many different ways by those affected, and their response will be influenced by various factors, such as their experiences leading up to the diagnosis, their perception of the meaning of cancer, their cultural background, their knowledge of treatment and treatment effects, how they have coped with traumatic events in the past and their individual coping styles9. Thus, it is important not to make assumptions about ‘cancer patients’, but rather to approach people diagnosed with cancer on an individual basis. It is also important to dispel any myths associated with cancer, for example, that cancer can be caught by kissing or touching.
Patients diagnosed with cancer face the daunting task of learning about the disease and possible treatments, as well as making a decision about treatment, usually within a relatively short time. Nurses caring for patients with cancer may play a role both in helping the person adjust to their diagnosis and in supporting them through the decision-making process. Nurses can teach patients to self-advocate for quality cancer care through teaching communication skills, how to find and manage information, as well as decision-making and negotiation skills10. Nurses can assist the person adjust to the diagnosis of cancer through: checking what information has been given by medical staff (to aid consistency); asking if they need more information, what support they need and how they are feeling; and above all, listening to their responses. Additionally, it is important to provide information at the pace and in the level of detail as preferred by the person concerned. Repetition of information may be needed, as it has been shown that patients may retain only a portion of the information provided, due to factors such as their emotional and psychological response to the diagnosis of cancer, any cognitive impairment, or a lack of motivation to learn (for whatever reason)11.