Office Environment and Daily Operations
Learning Objectives
1. Define, spell, and pronounce the terms listed in the vocabulary.
3. Explain why patient traffic flow is an important consideration in the office design.
4. List some of the expenses involved in the operation of a medical practice.
5. Describe how prices can be compared for medical office supplies.
6. Discuss the importance of routine maintenance of office equipment.
7. List several ways to save money and prevent waste in the medical office.
8. Discuss fire safety issues in a healthcare environment.
10. Identify emergency preparedness plans in the community.
11. Discuss potential roles of the medical assistant in emergency preparedness.
12. Describe the fundamental principles for evacuation of a healthcare setting.
13. Explain the difference between medical waste and regular waste.
Vocabulary
advance An amount of money or credit furnished in anticipation of repayment.
backorder An ordered item that is not delivered when promised or demanded but will be filled at a later date.
depleted Lessened markedly in quantity, content, power, or value.
discrepancies Differences between conflicting facts, claims, or opinions.
honorarium A payment in recognition of acts or professional services, usually on a special occasion.
incurred To become liable or subject to; to bring down upon oneself.
mitigating To cause to become less harsh or hostile; to make less severe or painful.
outsourcing The practice of subcontracting work to an outside company.
packing slip A list of items included in a shipment.
per diem By the day; per day. An allowance for daily expenses.
proactive Acting in anticipation of future problems, needs, or changes.
Scenario
Kayla Kemper performed her externship at Dr. Richard Tarago’s office, a general practice clinic downtown that serves lower income patients, most of whom do not have medical insurance. Some patients have a co-payment of $5 to $25; others have no co-payment, depending on their income level. Kayla’s family is quite wealthy, and working with patients whose lifestyle is very different from hers has been an eye-opening experience. On many days she wanted to leave the clinic, because she realized that a large number of patients were unable to seek medical care at the start of an illness, and when they finally came to the clinic, they were in worse condition.
Kayla is a caring person, and she saw the suffering many patients experienced daily. She found it tough to see people who had difficulty obtaining health care, yet she realized that a large number of Americans have no insurance coverage at all. Kayla discussed her feelings with the clinic manager, Elaine Mays, and expressed her concern for the patients in the clinic. Elaine asked whether Kayla would like to continue working with the patients, and Kayla admitted that she would, although it was not easy for her. Elaine then suggested that because Kayla’s background is so different from the patients, she might want to stay at the clinic as a volunteer for a few months to add to her learning experience. She accepted the offer, and after 3 months as a volunteer, Elaine hired Kayla to work in the clinical area full time. The patients consistently commented on how compassionately and considerately Kayla treated them. Kayla truly learned the meaning of giving as it relates to the medical profession. Her externship was the start of her full-time career.
While studying this chapter, think about the following questions:
• Why is it a good practice to allow the person who uses a certain supply to order it?
• Why might outsourcing be less expensive than doing testing or procedures in the office?
• How might an extensive list of community resources be helpful to patients?
New medical assistants may have difficulty putting all their skills together and using them at the same time throughout the course of a day. Medical assistants must be multitaskers and must develop a good memory. They also must be efficient workers. While in school, medical assisting students spend several days learning a specific skill, such as phlebotomy. However, during the externship and on the job, the medical assistant may need to perform a phlebotomy, chart a procedure, and check out a patient, all within a matter of minutes.
Most of the general tasks in the physician’s office are done daily, weekly, or monthly. Such tasks include preparing for the day, using the office policy manual, ordering and receiving supplies, cleaning, office budgeting, lunches and breaks, office security, travel arrangements, and ergonomics. The physician’s office is a busy environment where the medical assistant encounters new challenges each day. This chapter details the general office environment and the daily operations that the medical assistant may perform in the physician’s office. Multitasking is a critical skill that all medical assistants should strive toward; during a typical day, many duties will be carried out at one time and the medical assistant must keep track of the progress of each responsibility.
The more flexible the medical assistant, the more valuable he or she is to the physician. By learning and refining adaptation skills, medical assistants increase office efficiency, allowing the schedule to handle interruptions and emergencies. Remember that the patient is the reason the office exists and is of primary importance to the office staff. However, various tasks demand attention in the daily operation of the medical office.
The Office Policy and Procedures Manual
Virtually all businesses have some type of policy and/or procedures manual, but it is especially important in the physician’s office and other medical facilities. The manual should be easy to read, detailed, and logically organized. Besides providing administrative information, the manual also should provide procedural sheets that outline the steps of each procedure performed in the office. The manual should be a “living” document, constantly updated as technology advances and changed whenever regulations change. The manual must be reviewed annually for corrections and additions; this review must be documented as a step in the compliance with regulations established by the Occupational Safety and Health Administration (OSHA). Documentation can be a statement verifying that the manual has been reviewed; this statement should be dated and signed by the office manager or physician. One of OSHA’s most common citations for noncompliance is having a policy manual but not following the stated policy in various areas. The medical assistant must form the habit of going to the office policy manual whenever in doubt about any procedure.
Using the Office Policy Manual
All employees should read the office policy manual when they begin working in the physician’s office. Manuals and other office policy documents may be posted on the physician’s Web site, often in the sections pertaining to employees. Some physicians make these and other employee-related documents available in pdf format. Reading the manual helps the medical assistant become informed about the expectations of supervisors. However, the office policy manual is not only used for new employees (Procedures 12-1 and 12-2). The manual should be a reference that all employees use whenever necessary. OSHA requires that the policy manual be reviewed at least annually to make sure all the information is accurate and up-to-date. Whenever revisions are made, insert a page in the manual giving the date the revisions become effective.
After the revised manual has been reviewed and accepted, a memo can be distributed detailing the changes made and where to look for them.
The office policy manual should include sections that deal with several topics, such as:
Some offices require employees to sign a document stating that they have read and understand the entire policy. The manual should be written clearly and concisely in language that is easily understood. It should be used if a question arises about policy matters and also when an employee is unsure of the reason for or way to proceed with a task. A procedures manual often is combined with the policy manual. Regardless of the setup, every office task should be detailed in one of the two documents.
Opening the Office
Employees arrive earlier than patients so that the office can be prepared for the day. Some office policies dictate that the office be readied for the next day the evening before, but for the purposes of this chapter, assume that the policy requires preparation in the morning.
Although the physician may trust the employees, office policy should demand that supervisors be proactive in preventing theft. Depending on the size of the clinic, a certain number of employees will have keys and will know the alarm codes for the facility. The best policy is to monitor this access and information strictly. When numerous keys are distributed, more employees have after-hours access to the office. By limiting this access, the physician may prevent some losses to theft. Two things in particular make the physician’s office a target: money and drugs. Usually, only a limited amount of cash is kept in the office. However, most offices keep some medications, often narcotics, which can be addictive or sold for a profit on the street. If such items are used, they must be protected, not only for safety but also to remain in compliance with the law. Even during regular office hours, the staff should practice careful methods, such as keeping back doors locked securely, so that only those authorized are able to enter the building.
Preparing for the Day Ahead
Once the employees have arrived for work, all of them should begin preparing for patients and visitors. Each employee is responsible for his or her own work space, and the staff may work as a team to prepare common areas of the office, such as the reception area. When each person understands the duties required and when they are divided up among the staff, work can be completed quickly and efficiently.
Several duties are completed before the patients arrive. The voice mail or answering service should be checked to collect any messages left since the last time the staff was in the office (Figure 12-1). Some answering services send calls by e-mail or fax. Make sure a phone message book is handy when retrieving messages; write each one into the message book and include all information needed to respond to the message properly. This ensures that copies of the messages are available if one happens to get lost. Patients’ records may need to be pulled so that the medical assistant can take action and follow up on the messages.
Print two copies of the day’s appointments and place one copy on the physician’s desk unless he or she chooses to view the appointments on a computer system. Use the other copy to pull medical records for the patients who will visit the office during the day if paper records are kept. If the office does not use electronic health records, keep the paper medical records in a convenient, central area so that staff members can find them easily once the patients begin to arrive. Make sure the physician has enough room in the progress notes section of the medical record to write the details of the office visit. If needed, add a new sheet of progress notes. Glance over the notes from the last visit to determine whether laboratory work or treatments were ordered and find out whether the results are available.
Patient exam rooms should be restocked with all the regular supplies used in the individual rooms. Items such as cotton balls, bandages, gauze pads, patient gowns, and drapes need to be replenished daily. The physician and patient should never be forced to wait in the examination room while the medical assistant searches for supplies. Check the restrooms to make sure adequate toilet paper, soap, and hand towels are available. If urine specimen cups and towelettes are kept in patient restrooms, make sure enough are available to last throughout the day.
Be sure prescription pads are available for the physician, although they should not be left in open areas or on counters in exam rooms (Figure 12-2). Many physicians keep one pad in their pocket and the extras stored in a locked cabinet. Physicians using electronic health records can print prescriptions directly from their computer system or have them sent to the pharmacy electronically. Patients should never have access to prescription pads, because they might try to forge a prescription; this is a breach of federal or state law or both. Take extra care to keep prescription pads out of patients’ sight.
Certain equipment may need to be turned on, such as computers, laboratory equipment, and copy machines. Lights should be turned on in all the examination rooms. If quality assurance tests need to be performed on any of the laboratory machines, run the tests and record the results.
Some specimens from previous days may need to be checked for results or additional testing, although many physicians today use outside laboratories. Always record test results in the patient’s medical record. The medical assistant cannot decide whether a test result is abnormal; however, if that information is clearly indicated on the lab’s report form, then act according to office policy. Some physicians only want to see the test results if they fall outside normal ranges. Most laboratories print test results so that abnormal results are emphasized; they may be printed in a different color ink or in a separate column labeled “Abnormal.” If results are abnormal, the physician may need to do follow-up work or see the patient again. As mentioned, the medical assistant cannot judge whether a test result is abnormal, but if that information is clearly indicated, the medical assistant can file the document according to office policy.
The patient accounting system should be prepared for the day. Secure enough encounter forms for each patient in the appointment book. Stock the patient checkout area with plenty of appointment cards. If the office gives small gifts to patients, such as refrigerator magnets or coffee mugs, make sure they are available for use. Many offices place the physician’s business card just outside the receptionist’s window or in the patient reception area. Because patients often take one of the cards, this supply should also be checked.
Various specialty offices may need to prepare additional equipment; therefore, make sure everything necessary is available for the physician and staff members. The day runs smoother when the office is completely prepared for the patients. When all of these duties have been completed, the last task is to unlock the front door and begin welcoming patients to the practice.
Patient Traffic Flow
Ideally, the physician’s office is located in an area of town that is easy to find, has ample parking, and does not force the patient to do any excess walking, especially upstairs. The medical assistant is usually not involved with designing the interior of the office; however, the placement of all furniture and equipment is an important factor in the efficient flow of traffic. Patients should be able to quickly determine the location of the patient waiting room. It is helpful if one room is designated as a “sick room” so that well patients will not be stricken with an illness just from visiting the office (when space is short, a face mask may be issued to patients with symptoms of communicable disease). Good traffic flow is important so that the patients and employees can maneuver through the office easily and avoid retracing their steps. Additionally, patients should be able to locate separate parts of the office, such as the lab or check-out areas. Neither patients nor employees should be subjected to dodging furniture or tripping over equipment cords. When moving through the hallways, guide the patient along the right side and leave the left for those traveling in the opposite direction.
Visitors to the Office
Many people besides patients visit the physician’s office. Some of these individuals have appointments; others stop by at random. The office policy manual should detail the procedure to follow in dealing with such individuals. Most physicians prefer to set aside a specific time for pharmaceutical representatives (also called detail persons or drug reps). These professionals usually are quite competent and knowledgeable about various drugs, and they should be treated with respect by all members of the office staff. In the past, pharmaceutical representatives were allowed to leave memo pads, pens, and other gift items for the physicians and staff that advertised a certain drug or treatment. Many states have laws that prevent pharmaceutical companies from providing these perks. However, some states may not have passed such laws, and physicians still can receive these items. Lawmakers are more concerned about perks such as an honorarium for serving as a guest speaker than about pens and notepads. However, many lawmakers believe that physicians’ prescribing habits are directly related to pharmaceutical company perks. The company’s goal is to educate the physician about their products so that the physician can better care for patients. Some states are developing laws that require reporting of any gifts of more than $25; in most states, this does not include the free samples of the actual drugs. In general, most physicians have decided not to accept these gifts so that no question arises of any breach of ethical conduct.
Pharmaceutical representatives are not the only salespersons who may visit the physician’s office. Salespeople from office supply stores, medical equipment sellers, and others may stop by to make appointments or take orders for various items. The office manager usually can address the needs of salespeople and normally is authorized to place orders.
At times, other physicians stop by the office to see the doctor. They may not have an appointment, but the physician should be notified at once when another doctor is waiting in the reception area. If office policy allows, take the visiting physician to the doctor’s office instead of forcing him or her to wait in the patient reception area. Because doctors understand busy schedules, most do not stop by another doctor’s office without an important reason.
The physician’s family members or friends may visit the medical office. Never send family members or friends away without notifying the physician of their presence and asking whether he or she has time to speak to them.
Daily, Weekly, and Monthly Duties
Develop a list of duties that are performed daily, weekly, and monthly. Checklists are helpful when staff members want to make sure all duties are completed. The lists help the supervisors divide work evenly among staff members. Be specific on the checklist and include every task that needs to be done, even the most insignificant ones. If a staff member is struggling to finish her daily duties, other staff members should assist so that all required jobs are completed for the day. Take the initiative and work as a team; the effort may be important when supervisors choose employees to promote or terminate.
Constant Cleaning
Patients expect the physician’s office to be immaculate. Nothing should be or appear dirty in any part of the facility. Keeping the office truly clean helps curb the spread of germs and communicable diseases. Effective cleaning products should be used daily, especially in high traffic areas. Countertops, sinks, door handles, and restrooms should be checked frequently and cleaned whenever necessary. When and if slow periods occur between patients or during lengthy office visits, take a cloth and use a disinfectant on nearby counters or around door handles. Look for things to clean in the office. By being conscientious about these things, the medical assistant becomes more valuable to the physician. Supervisors and physicians notice this productivity; good cleaning habits reflect positively on the medical assistant and are important factors in employee evaluations.
Cleaning Services
Many offices employ a cleaning service that performs more intensive chores. These professionals usually come to the facility during the evening, when patients and staff are gone. They clean and disinfect the bathrooms, vacuum, dust, and empty trash. They also may perform other specific tasks as required by the office staff. The office manager should establish some means of communicating with the head of the cleaning team. Many offices leave a notebook for the cleaning crew that details specific cleaning tasks to be performed in addition to regular cleaning tasks. The office manager should delegate a staff member to be the contact person for the service. If any task is not completed in a satisfactory manner, immediately contact the cleaning supervisor and resolve the problem. Make sure a log is kept so that tasks are listed and note whether they were completed or the reason they were not completed. Always inspect what is expected; the cleaning service must perform the jobs it is being paid to do. Do not allow situations to go unresolved. Be open and frank with services that do not meet expectations.
Filing
The medical assistant rarely has a shortage of documents ready to be filed. Although this task sometimes is monotonous, filing is a critical job that must be completed accurately and in a timely manner (Figure 12-3). If a laboratory result is not placed in the right medical record, important information that may affect the patient’s health could be lost.
Supplies and Equipment in the Physician’s Office
The medical assistant is responsible for stocking exam rooms and making sure all supplies and equipment are available and in good working order. The following sections describe the process of ordering and receiving medical supplies and equipment.
Identifying the Need for Specific Supplies
The medical assistant orders supplies periodically to ensure that the physician has everything needed to treat patients. The office policy and procedures manual details how employees should identify the need for certain supplies, order them, check them in, and place them in the office inventory for use. Nothing is more frustrating to the physician than reaching for an item during a procedure, only to find it is unavailable. Communication is the key to keeping supplies in stock.
Budgeting
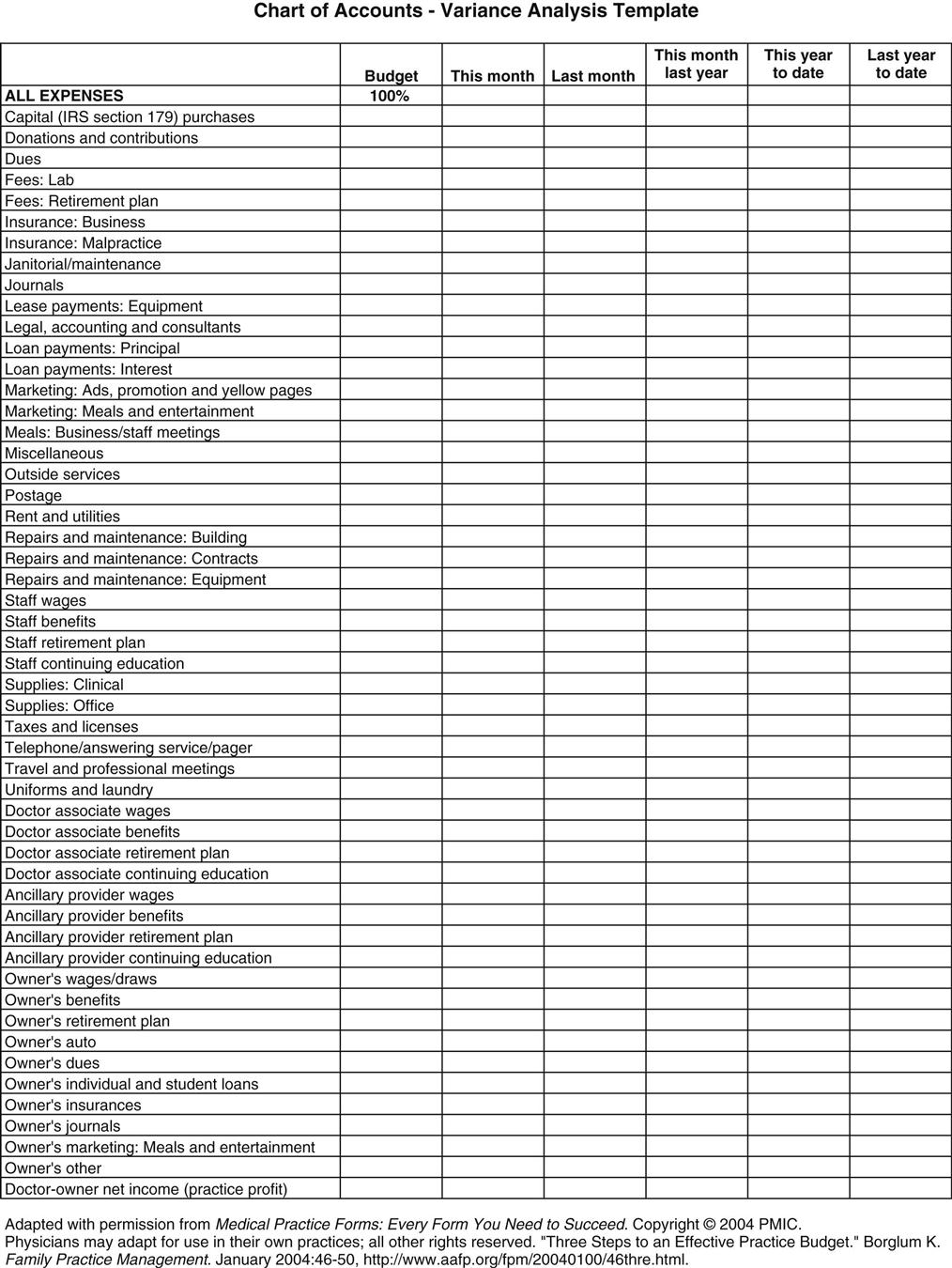
Most offices use an annual budget to determine the amount of money to be spent on various categories of expenses (Figure 12-4). Some expenses involved in the operation of a medical practice include:
Expense categories are important, because most business expenses can be deducted on tax returns, and staff salaries are directly related to the physician’s overhead costs. Always keep receipts for items to be used in the medical office and submit them in a timely manner to the office manager or other designated individual.
Businesses usually plan expenses for the year in advance, allocating expected income into various categories of expenses. Then, at least monthly, expenses are logged into a ledger or spreadsheet and separated into specific categories. This allows tracking of expenses to ensure that a category is not over budget. If a specific category of expenses is over budget, adjustments may need to be logged in, either to allot more funds to that category or to stop spending in that category until the next year. Exceeding the allowed amount in a budget is not necessarily uncommon; however, good business practice dictates that budgets come in very close to the estimations made at the beginning of the budget year. When a category goes over budget, money often must be taken from another budget category to cover the amount. This reduces the money available in the second category. Employees should not be allowed to spend money needlessly or wastefully. The physician should designate a minimum number of people to make purchases on behalf of the facility.
Comparing Prices
A good shopper is an asset to the physician’s office. Compare prices when shopping for supplies and equipment. Tell salespeople that comparisons will be conducted and that price will be a strong consideration when the time comes to make a purchase. However, price should not be the only consideration. Warranties, bulk purchase opportunities, maintenance agreements, and other factors may influence the best deal available on a certain item. Quality is another important factor; the physician may be willing to pay more for an item based on its quality and durability. Personal preference also influences purchasing decisions. The clinical medical assistant may prefer one brand of needles over another, even though they are the same price. In most circumstances, those who regularly use a certain item should be allowed to decide the brand, model, or other specifics before the item is purchased.
Most companies produce a catalog, whether online or printed. When a need has been identified, compare the prices from at least three sources before placing an order. For instance, if 70% isopropyl alcohol is needed, and the stock must last 6 months, first determine how much is needed. Suppose that approximately one 16-ounce bottle is used per month in each of five treatment rooms. Further suppose that the following prices are listed:
| Smith’s Medical Supply | 1 dozen bottles | $10. 53 |
| Argosy Medical and Dental Supply | 2 dozen bottles | $17. 44 |
| Walgreens | 1 bottle | $ .53 |
| CVS Pharmacy | 1 gallon | $ 6. 12 |
If these prices are compared, and assuming all other aspects of the products are equal, buying bottles of alcohol at Walgreens clearly is a better deal than buying one or two dozen at either Smith’s Medical Supply or Argosy Medical and Dental Supply. The alcohol at Smith’s costs approximately 87¢ per bottle; at Argosy, the cost is approximately 72¢ per bottle. Is the gallon a better buy? Let’s work it out. The alcohol can always be poured into containers from the gallon bottle. A gallon has 128 ounces; it therefore can provide only 8 16-ounce bottles; the cost per bottle is approximately 76¢. Walgreens, at 53¢ per bottle, has the lowest price. Still, if Walgreens is 15 miles away, the gas used to get the alcohol may push the total cost higher than the total cost of driving 2 miles to Argosy to buy the product. Also consider delivery and shipping and handling charges, in addition to sales taxes, that might be added to the cost of the order. Some suppliers may cut the cost on certain items to get the order, either meeting or beating the deal offered by another supplier. Examine all costs before placing the order with a supplier.
Ordering Supplies
Responsibility for ordering supplies in the medical office should be assigned to one person. The medical assistant who assumes this task can use various methods to track the needed supplies and then place orders to replenish them. One simple method is to develop a spreadsheet that lists all the products and supplies that need to be ordered periodically (Procedure 12-3). Post the sheets in areas where supplies are stored. When staff members take supplies from storage, they should make a note on the spreadsheet. When it is time to place an order, the sheets are gathered and used to determine which supplies need to be replenished. Some offices use software programs to prepare orders, and others use a computer system to enter products taken from the supply area. Still others may use a sticker system, in which a coded sticker is removed when a product is used and placed on a card or form; that amount then is charged to the patient. Others use a note card system, in which a note card is prepared for each supply item, and after the inventory has been performed; orders are completed based on the needs reflected by the note cards. After determining the items that need to be ordered, browse medical or office supply catalogs to shop for the best prices (Procedure 12-4). The order may need to be divided and offered to two different suppliers if certain items can be obtained at a better rate.