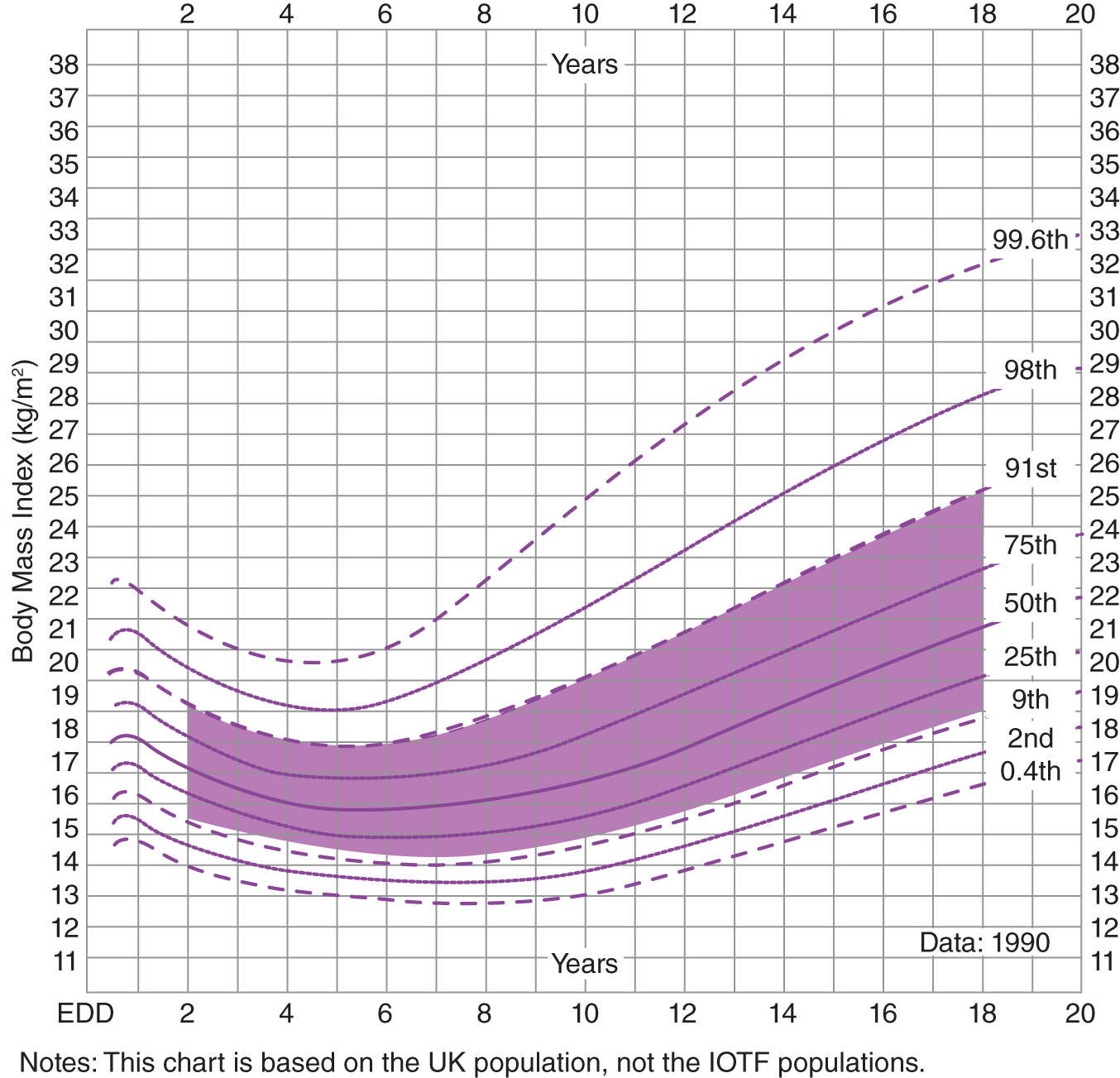
Janice Christie School nurses are responsible for health promotion and health maintenance of school-aged children, they support the wellbeing of individual children and attend to the public health of the school population; for further information of the public health role see Christie et al. (2009). In this section you will be asked to consider Jane’s intervention for one child (Jake) and in addition, interventions for the school population. The Neuman system model (Neuman & Fawcett 2002) can be applied to one person, a group or population of people and therefore, it can be used as a model to develop a one-child and a public health school care plan. You may find that some of your answers (particularly for questions 5 and 6) differ from the ones suggested. There are many possible acceptable responses for some questions, a good answer is based on evidence, so ensure that you use contemporary research and/or relevant local or national evidence-based guidelines when formulating your answers. Obesity is a condition that indicates risk to health, associated with excess body fat. It is usually defined according to body mass index (WHO 2020). Body mass index (BMI) is a ratio of a person’s weight in kilograms divided by height in metres2. For adults BMI can be classified as follows: BMI may be supplemented with waist measurements in adult with a BMI less than 35 kg/m2 (NICE 2014); waist size has close link to morbidity (disease) and mortality (death) even in people who are not overweight (Harvard School of Public Health 2012). It is more complicated to undertake an obesity assessment in children as BMI varies with age and gender. NICE (2014) suggests using the RCPCH UK-WHO growth charts (RCPCH, 2021). Children who are over the 91st centile on the BMI centile look up chart may be classified as overweight and those above the 98th centile, classified as obese. Children and young people who have excess weight are more likely to have an associated morbidity such as joint problems and pre-diabetes, they often have poor psychological wellbeing, be bullied and have more school absences (PHE, 2016). It is recommended that healthcare professionals should help identify children and families at risk (ASK), explain how to change to healthy behaviours (ADVISE) and refer for further support (ASSIST) (PHE, 2017). This discussion should be supportive, non-blame based, and factual. Refer to Figure 18.1 for boys growth charts. FIGURE 18.1 RCPCH UK-WHO growth charts for boys. Obesity arises from an energy imbalance between energy intake (from food and drink) and energy expenditure (internal body processes and physical activity) (RCP et al. 2004). Weight gain occurs when energy intake (calories consumed) exceeds total daily energy expenditure for a prolonged period. Childhood obesity is associated with maternal and parental obesity, poor diet, and lower amounts of physical activity (PHE 2016). There is a complex mix of personal, social, and environmental factors that contribute to weight gain (PHE 2016), and Butland et al. 2007) suggests that genetics/biology loads the gun of obesity (makes people predisposed to obesity) and the environment factors pull the trigger (brings about the conditions in which obesity happens). Neuman’s system model (Neuman & Fawcett, 2002) identifies five client variables: The consequences of obesity (drawn from PHE 2016) will be considered for each of these five client variables. Physiological consequences of obesity in childhood include: Current evidence indicates that interventions that help improve diets and/or activity levels can promote more healthy weights in children up to 12 years of age (Brown et al. 2019). Psychological/cognitive consequences of obesity in childhood include a lower self-esteem (PHE 2016). Socio-cultural consequences of obesity in childhood include stigmatisation, bullying and increased school absence (PHE 2016). There is currently little evidence about the spiritual consequences of obesity in childhood, however, adult studies with people with eating disorders suggest it may be associated with reduced hope and lower spiritual wellbeing (Boisvert and Harrell 2013a; 2013b). Developmental consequences of obesity in childhood may include a life course impact; obese children are more likely than their non-obese peers to become obese adults with an increased risk of ill health and premature mortality (PHE 2016). Neuman’s system model (Neuman and Fawcett, 2002) identifies three types of stressors that can act on individuals or groups of individuals’ five variables. Stressors can be: Stressors can have actual (overt), potential (covert) or residual effects. The model also identifies that people have lines of defence or resistance that help protect the body from stressors. Intrapersonal stressors include: Interpersonal stressors include: Extra-personal stressors include: Jake’s lines of defence and resistance could include: A Neuman system model assessment and intervention tool has been developed to help apply the model to the nursing process in practice settings, for more information about this tool please refer to Neuman and Fawcett (2002). Note, the author has adapted and modified the Neuman’s system model care plan process to better support the learning aims of this book. When devising a care plan, please remember to identify the level of nursing intervention (as per Neuman’s model) that you will use. Neuman’s system model identifies three levels of nursing interventions: PHE (2016) recommends that health professionals should provide evidence-based advice about weight, diet and physical activity for children/young people and their families. In addition, NICE (2013) advises that healthcare professionals should assess the family for readiness and willingness to be referred to and attend a local effective lifestyle management service. If a child or young person is assessed as needing specialist support, they should also be referred to appropriate services (e.g. specialist obesity, paediatric of Child and Young People Mental Health Services (CYPMHS/CAMHS) services). Jake’s care plan Secondary prevention advice to Jake and his mother regarding: Food served on smaller plates to reduce food portion consumed. Regular meals to reduce binge eating. Increase in daily intake of water, complex carbohydrates, and fruit and vegetables consumption; to decrease sugary drink and fried food/processed intake. Ensure Jake and his mother are aware of local resources and services that support healthy eating and/or healthy weight. Secondary prevention: Reduce time of uninterrupted playing of video games (sedentary behaviour). Encourage walking to school. Encourage a range of different physical activities such as sport and climbing to build muscle and bone strength. Family activity at weekends. Ensure that Jake and his family are aware of local services and resources supporting physical activity e.g. sports clubs. Secondary prevention: To repeatedly set realistic, easily achievable, short-term goals. To encourage and praise Jake for achieving goals. Encourage and support Jake in undertaking new activities. Conjointly work on coping strategies for situations and social interaction skills. Referral to school healthy club for peer support or other local support services or resources as appropriate e.g. Child and Young Peoples’ Mental Health Services or YoungMinds. Meet with Jake weekly and ask about his accomplishments, self-belief, and coping. Record monthly BMI readings for next six months with supportive feedback on progress. Tertiary prevention: Ensure that Jake and his mother are aware of school anti-bully policy procedures and empower and support the family in reporting incidents. Build Jake’s self-esteem and teach assertive and communication skills strategies; offering support in line with school policy. Ensure that Jake and his family are aware of additional voluntary support services, such as Childline or ParentLine Plus. Intra-school stressors: Interschool stressors: Extra-school stressors: School lines of defence and resistance: Rates of obesity among children and young people are currently high in many countries and obesity has enduring impacts on health and wellbeing; due to these enduring impacts we now need across sector and community action to protect and improve child and young person health (Davies, 2019). There are many personal and environmental factors that impact attaining and maintain healthy weight (PHE 2016); therefore, it is appropriate supporting individuals and schools through pupil-specific and school-focused care plans. The Neuman grand theory/model (Neuman & Fawcett 2002) focuses on ‘prevention’ which makes this model relevant for nurses involved in promoting both public and personal health, as it supports nursing assessment and interventions for both individuals and populations. In addition, the model promotes assessment of psychosocial, physical, and developmental needs and this holistic focus means it can help address a wide range of factors that influence child and young person health. Thus, the Neuman model is a useful tool for care planning for children’s and school nurses, engaged in individual child, young person, family, or community focused health promotion. Primary prevention Working with headmaster, pupils, and canteen staff regarding canteen image and marketing healthy foods on the menu. Working with teachers and pupils regarding classroom teaching about healthy foods, how to make food choices, and how to make basic healthy foods (resources for teachers are available via PHE 2021). Working with headmaster, school staff, parent committee, and pupils regarding holding family fun events to promote healthy eating and food preparation. Working with Treeland neighbourhood committee to improve local food amenities. Primary prevention: Working with teachers and pupils regarding increasing activity in classrooms, a range of active playground games, and additional PE/sports sessions in school week. Working with teachers regarding classroom teaching about healthy activity and increasing physical activity during class. (Resources for teachers are available via PHE 2021). Working with headmaster, school staff, parent committee, and pupils regarding holding family fun events to promote physical activities and improving school open spaces and playground to create active environments. Work with school and families to promote active travel to and from school. Working with Treeland neighbourhood committee to improve local play amenities. Primary prevention dietary and physical activity as above. Encourage school to register with Change4life School Zone (PHE, 2021) to access resources promoting health in the classroom. In addition: Secondary prevention. Healthy after school club set up for children who are overweight, offering professional advice/ support and peer support. * Accelerometers are recording devices that record body movement and distance moved.
CHAPTER 18
Obesity
SOME HELPFUL ADDITIONAL INFORMATION
PROPOSED ANSWERS TO QUESTIONS
Question 1. What is obesity and how is it usually defined?
Question 2. What are the risk factors for childhood obesity?
Question 3. Considering Neuman’s system model/grand theory five variables; what are the possible consequences of childhood obesity for pupils, such as Jake?
Question 4. Using Newman’s model and the scenario at the start of this chapter, identify possible stressors and lines of defence or resistance for one pupil (Jake) by considering the five variables and their effect on his weight.
Question 5. Based on the information from questions 2–4, develop a healthy weight care plan for Jake
Assessed need
Plan
Type of intervention/implementation
Evaluation
Rationale
Jake has an imbalanced dietary intake contributing to unhealthy weight.
To increase Jake’s consumption of healthy foods and drink within a month focusing on positive change.
Meet with Jake and his family weekly to discuss Jake’s dietary intake and changes made.
Advice to follow the Eatwell guide (NHS choices, 2021).
Jake has low physical activity, contributing to unhealthy weight.
To increase Jake’s level of physical activity to an average of at least 60 minutes of moderate to vigorous intensity physical activity (PA) per day across a week and minimise the duration of sedentary activity.
Meet with Jake and his family weekly to discuss physical activity undertaken and changes made.
Advice to follow UK Chief Medical OfficersPhysical Activity guidelines (2019).
Jake has low self-esteem and has few friends.
To improve self-esteem so that he believes in himself so that he can achieve a healthy weight within the next six months.
Communicate supportively, using neutral and non-blaming language (PHE 2017).
Jake has previously been bullied and is at continued risk.
Within the next three months help Jake to deal with bullying behaviour effectively.
During meetings with Jake and his family during the next three months, enquire about Jake’s wellbeing and achievements, also his relationships with other children.
Adhere to DE (2017) and local guidelines on preventing and tackling bullying.
Question 6. Identify the possible stressors and lines of defence or resistance on healthy weight maintenance for the entire Treewood school population. Based on your assessment and the information from questions 2–3, can you develop a healthy weight care plan for the school?
SUMMARY
Assessed need Treewood
Plan
Type of intervention/implementation
Evaluation
Rationale
School has social, organisational, and environmental factors that are contributing to unhealthy food choices by pupils.
To help school pupils in making healthy food choices, thereby increasing the intake of fruit and vegetables and decreasing the amount of high sugar and high fatty foods eaten within the next six months.
Evaluation of interventions put in place and monitor their effect on reception year and year 6 students by helping students complete a diary of foods eaten during school time and out of school time, in six months’ time.
Work with school to support compliance with DE, (2019).
School has social, organisational, and environmental factors that are contributing to unhealthy physical activity levels in pupils.
To help school pupils to make healthy physical activity and thereby reduce sedentary behaviour and increase activity levels within the next six months.
Evaluation of interventions put in place and their effect on reception year and year 6. Monitor school physical activity rates and amount of sedentary behaviour by diary or using accelerometers* (during and outside school hours), in six months’ time.
Ensure a multicomponent intervention and active environment in line with PHE (2020).
Some pupils are overweight or obese.
To decrease the percentage of overweight or obese pupils over a school year.
Evaluation of Healthy club outcomes and BMI recording at beginning and end of this school year.
Application of NICE (2013) guidelines for effective lifestyle programmes.
Some pupils who have been overweight or obese are now healthy weights.
To help previously overweight or obese pupils maintain healthier weights over their school career.
Tertiary prevention: Ongoing healthy club support for children who have regained normal weight, i.e. offering ongoing professional and peer support.
Evaluation of healthy club outcomes, BMI recording as required during their time at school.
There is a need for ongoing support to ensure long-term programme effects are sustained (Flynn et al. 2006).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


