O
Ostomies
Description
An ostomy is a surgical procedure that allows intestinal contents to pass from the bowel through an opening in the skin on the abdomen. The opening is called a stoma, and it is created when the intestine is brought through the abdominal wall and sutured to the skin. The intestinal contents then empty through the hole on the surface of the abdomen rather than being eliminated through the anus.
An ostomy is used when the normal elimination route is no longer possible. For example, if the person has colorectal cancer, the diseased portion is removed together with a certain margin of healthy tissue. Sometimes the tumor can be resected, leaving enough healthy tissue to immediately anastomose (reconnect) the two remaining ends of healthy bowel, and no ostomy is necessary. If the tumor involves the rectum and is large enough to necessitate the removal of the anal sphincters, the anus is sutured shut and a permanent ostomy is created.
Types of ostomies
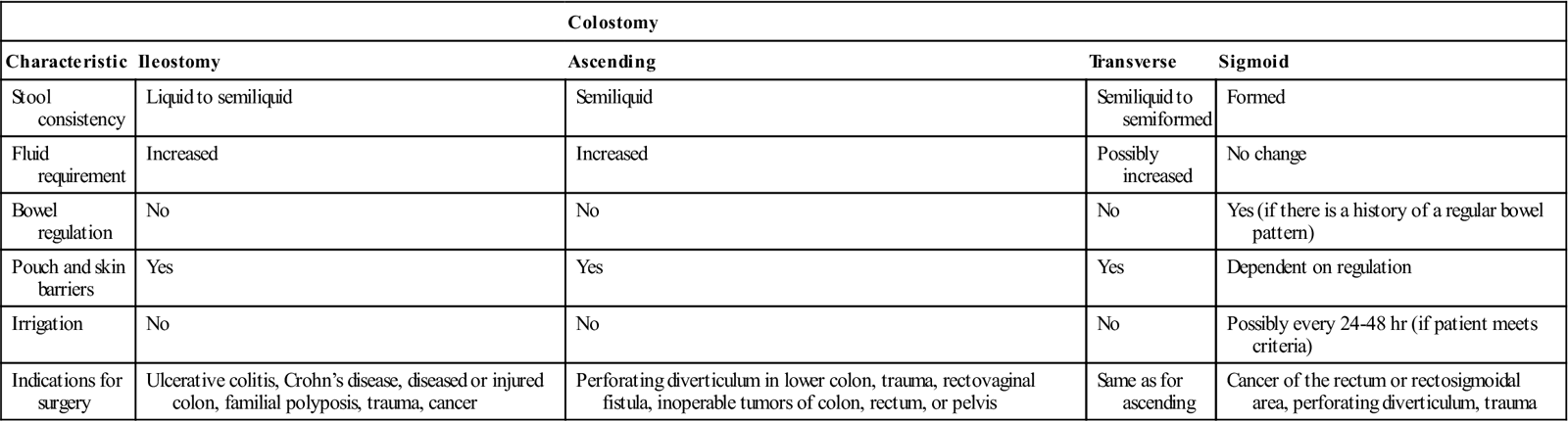
Ostomies are described according to location and type (Fig. 23). An ostomy in the ileum is called an ileostomy and an ostomy in the colon is called a colostomy. The ostomy is further characterized by its anatomic site (e.g., sigmoid or transverse colostomy). The more distal the ostomy, the more the intestinal contents resemble feces that is eliminated from an intact colon and rectum. A comparison of colostomies and ileostomies is shown in Table 95.
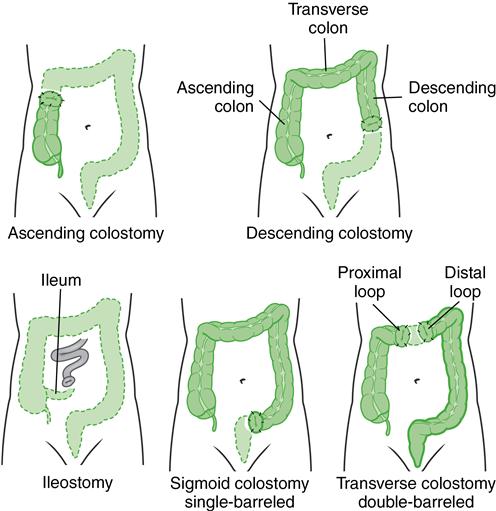
Table 95
Comparison of Ileostomy and Colostomy
| Colostomy | ||||
| Characteristic | Ileostomy | Ascending | Transverse | Sigmoid |
| Stool consistency | Liquid to semiliquid | Semiliquid | Semiliquid to semiformed | Formed |
| Fluid requirement | Increased | Increased | Possibly increased | No change |
| Bowel regulation | No | No | No | Yes (if there is a history of a regular bowel pattern) |
| Pouch and skin barriers | Yes | Yes | Yes | Dependent on regulation |
| Irrigation | No | No | No | Possibly every 24-48 hr (if patient meets criteria) |
| Indications for surgery | Ulcerative colitis, Crohn’s disease, diseased or injured colon, familial polyposis, trauma, cancer | Perforating diverticulum in lower colon, trauma, rectovaginal fistula, inoperable tumors of colon, rectum, or pelvis | Same as for ascending | Cancer of the rectum or rectosigmoidal area, perforating diverticulum, trauma |
The major types of ostomies are end stoma, loop, and double-barrel ostomies.
The procedures used to perform ostomy surgeries are further discussed in Lewis et al.: Medical-Surgical Nursing, ed. 9, pp. 990 to 991.
Nursing management
Preoperative care
Preoperative care that is unique to ostomy surgery includes (1) psychologic preparation for the ostomy; (2) selection of a flat site on the abdomen that allows secure attachment of the collection bag; and (3) selection of a stoma site that will be clearly visible to the patient to facilitate self-care. Psychologic preparation and emotional support are important as the person copes with the change in body image and a loss of control over elimination and its odors.
Postoperative care
Postoperative nursing care includes assessment of the stoma and provision of an appropriate pouching system that protects the skin and contains drainage and odor. The stoma should be dark pink to red. A dusky blue stoma indicates ischemia, and a brown-black stoma indicates necrosis. Assess and document stoma color every 4 hours. Teach the patient that the stoma is mildly to moderately swollen the first 2 to 3 weeks after surgery.
All pouching systems consist of an adhesive skin barrier and a bag or pouch to collect the feces. The skin barrier is a piece of pectin-based or karaya wafer that has a measurable thickness and hydrocolloid adhesive properties.
 Patient and caregiver teaching
Patient and caregiver teaching
Colostomy care
A colostomy in the ascending and transverse colon has semiliquid stools. Instruct the patient to use a drainable pouch. A colostomy in the sigmoid or descending colon has semiformed or formed stools and sometimes can be regulated by the irrigation method. The patient may or may not wear a drainage pouch. A well-balanced diet and adequate fluid intake are important.
Colostomy irrigations may be used to stimulate emptying of the colon. Regularity is possible only when the stoma is in the distal colon or rectum. If bowel control is achieved, there should be little or no spillage between irrigations, and the patient may need to wear only a pad or cover over the stoma. The procedure for colostomy irrigation is presented in Table 96.
Table 96
Patient and Caregiver Teaching Guide
Colostomy Irrigation



