Ashley Zerwekh Garneau, MS, RN
Nursing Theory
The only good is knowledge and the only evil is ignorance.
—SOCRATES (469 BC-399 BC)
After completing this chapter, you should be able to:
• Identify the purposes for nursing theory.
• Describe the origins of nursing theory.
• Describe some of the key words associated with nursing theory.
• Identify some of the more well-known and well-developed nursing theories.
• Discuss some of the main points of each of these theories.
Just mentioning the word theory, let alone nursing theory, can make many nurses’ yawn reflexes start to work overtime. What is theory? Who are nursing theorists? What are the different nursing theories? Most nurses are not aware of theory, nor can they name a nursing theorist. Nursing theories are a way to organize and think about nursing, and the people who wrote theories are part of our nursing history. Theory provides an overall “theme” to what nurses do. In this chapter, the key words related to theory are defined, and the main elements of eight nursing theories are summarized.
Nursing Theory
What Is Theory?
Quite simply, theories are words or phrases (concepts) joined together in sentences, with an overall theme, to explain, describe, or predict something. A more complex definition of a theory is “a set of interrelated concepts, definitions, and propositions that present a systematic way of viewing facts/events by specifying relations among the variables, with the purpose of explaining and predicting the fact event” (Kerlinger, cited in Hickman, 2003).
Theories help us understand and find meaning in our nursing experience and also provide a foundation to direct questions that provide insights into best practices and safe patient care. Ellis (1997) stated, “A theory is a coherent set of hypothetical, conceptual and pragmatic principles forming a general frame of reference for a field of study” (p 373). You might see theory referred to as a conceptual model or a conceptual framework.
Nursing theory is, according to Meleis (cited in Hickman, 2003), “an articulated and communicated conceptualization of invented or discovered reality in or pertaining to nursing for the purpose of describing, explaining, predicting or prescribing nursing care” (p 16).
The bottom line is that words and phrases (concepts) are put together into sentences (propositions that show the relationships among the words/concepts), with an overall theme, to create theories. Theories also have some basic assumptions (jumping-off points; what is assumed to be true), such as the idea that patients need nurses. Nursing theories also define four metaparadigms (metaparadigms refer to big, comprehensive concepts) and address the nursing process.
What Nursing Theory Is Not
Nursing theory is not managed care, primary nursing, team nursing, or any other more business-related method of delivering care. Nursing theory is not obstetric nursing, surgical nursing, home health nursing, or any other nursing specialty; however, nursing theory can be applied to all of areas of nursing, including administration, education, patient care, and research. Nursing theory is by nurses and for nurses, providing quality care to their patients, either directly or indirectly.
Why Theory?
Consider all that you do as a nurse. What you do is based on principles from many different professions, such as biology, sociology, medicine, ethics, business, theology, psychology, and philosophy. What is specifically based on nursing? Also, if nursing is a science (and it is), there must be some scientific basis for it. Furthermore, theory helps define nursing as a profession (Figure 8-1).
Theory is a means to gather information, to more clearly and specifically identify ideas, to guide research, to show how ideas are connected to each other, to make sense of what we observe or experience, to predict what might happen, and to provide answers. A nurse is not a “junior physician,” although for years nursing care has been based on the medical model. Because nursing is a science (as well as an art) and a unique profession in its own right, nurses need nursing theory on which to base their principles of care (Critical Thinking Box 8-1; Evidence-Based Practice Box 8-1).
What Is the History of Nursing Theory?
In studying nursing theories and the people who created them, it is important to look at the background of the theorist, as well as how life experiences, beliefs, and education influenced the resulting theory. What are the overall theme and main ideas of the theory, and how does the theorist define the four nursing metaparadigms (Box 8-1)?
Florence Nightingale is considered to be the first nursing theorist. She saw nursing as “A profession, a trade, a necessary occupation, something to fill and employ all my faculties, I have always felt essential to me, I have always longed for; consciously or not … The first thought I can remember, and the last was nursing work …” (cited in Dunphy, 2002). Now, you might not feel that dedicated, but Nightingale also stated, “Nursing is an art … It is one of the Fine Arts; I had almost said, the finest of the Fine Arts” (cited in Dunphy, 2002).
Nightingale had various influences, including her education (which was fairly comprehensive for a 19th century English woman), her religion (Unitarianism), the history of the time (the Crimean War and invention of the telegraph), and her social status. The Unitarian belief involved salvation through health and wholeness, or our modern-day “holism.” Nightingale believed that there was no conflict between science and spirituality. Science was necessary for the development of a mature concept of God. She also studied many other religions throughout her lifetime and considered starting a Protestant religious order of nuns (Dunphy, 2002).
Nightingale came from a very wealthy family and enjoyed traveling throughout Europe, one of the destinations being Kaiserwerth in Germany, where she observed and was moved by nuns caring for the ill. Nightingale felt a “calling” to care for others and began training with various groups, usually nuns who cared for the sick. When the Crimean War broke out, Nightingale was asked and volunteered to go to care for the wounded English soldiers. The Crimean War was the first war since the invention of the telegraph, so news of the war was more immediate than had been previously experienced (Dunphy, 2002).
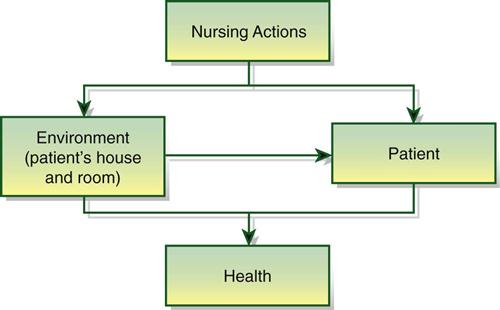
The overall theme of Nightingale’s theory was that the person is influenced by the environment. When she went to help soldiers during the Crimean War, her initial intent was to feed the soldiers healthy food and to clean the place (Figure 8-2). When soldier mortality rates fell, a legend was born (Dunphy, 2002)!
Nightingale believed that nursing was separate from medicine and that nurses should be trained (although we prefer the word educated). She also believed that the environment was important to the health of the person and that the nurse should support the environment to assist the patient in healing (Dunphy, 2002).
To define the metaparadigms, Nightingale noted that the person is the center of the model and incorporated a holistic view of the person, someone with psychological, intellectual, and spiritual components. The nurse was a woman (because only women were nurses in Nightingale’s day) who had charge of the health of a person, whether in providing wellness care, such as with a newborn, or in providing care to the sick. Health was the result of environmental, physical, and psychological factors, not just the absence of disease (Dunphy, 2002).
No other theories were identified or published until the 1950s when Peplau published her theory based on the interpersonal process. Other nurses were working on theories during that time and into the 1960s. In the 1970s, nursing was beginning to see itself as a scientific profession based on theoretical ideas (Table 8-1). In 1972, the National League for Nursing (NLN) required that nursing curricula be based on conceptual frameworks (McEwen, 2011).
TABLE 8-1
| YEAR | THEORIST | THEORY DESCRIPTION |
| 1860 | Florence Nightingale | Although her model did not have a specific name, the basic underpinnings revolve around how a person is influenced by the environment. Nursing was a “calling” to help the patient in a reparative process by directly working with the patient or indirectly by affecting the environment to facilitate health and recovery from illness. |
| 1952 | Hildegard Peplau | Interpersonal Relations Model—describes the four phases of the dynamic relationship between nurse and patient: orientation, identification, exploitation, and resolution. |
| 1960 | Faye Abdellah | Patient-Centered Approach—develops a list of 21 unique nursing problems related to human needs; promoted the use of a problem-solving approach to practice rather than merely following physician orders. Responsible for changing the focus of nursing theory from a disease-centered to a patient-centered approach and moved nursing practice beyond the patient to include care of families and the elderly. |
| 1961 | Ida Jean Orlando | Theory of Deliberative Nursing Process—focuses on the interpersonal process between nurse and patient through a deliberative nursing process; most concerned with what was uniquely nursing. |
| 1966 | Virginia Henderson | One of her main topics is the “unique functions of nurses.” All of her materials provide a focus for patient care via 14 basic needs. |
| 1969 | Myra Estrin Levine | Conservation Model—focuses attention on the wholeness of the person, adaptation, and conservation, which is guided by four principles (conservation of energy, structure, personal integrity, and social integrity). |
| 1970 | Martha Rogers | Science of Unitary Human Beings—an abstract model addressing the complexity of the “unitary human being,” which allows for the examination of phenomena (energy fields, paranormal) that other theories do not describe, as nurses promote synchronicity between human beings and their environment/universe. |
| 1971 | Dorothea Orem | Self-Care Nursing Theory—three interwoven theories of self-care, self-care deficit, and nursing system help the nurse to identify strategies to meet the patient’s self-care needs. |
| 1971 | Imogene King | Theory of Goal Attainment—patient goals are met through the transaction between nurse and patient involving three systems (personal, interpersonal, and social). |
| 1972 | Betty Neuman | Neuman Systems Model—focuses on wellness and mitigating stress within three levels of prevention: primary, secondary, and tertiary. |
| 1974 | Sister Callista Roy | Roy’s Adaptation Model—individual seeking equilibrium through the process of adaptation; identified six physiological needs (exercise and rest; nutrition; elimination; fluid and electrolytes; oxygenation and circulation; and regulation of temperature, senses, and endocrine system). |
| 1976 | Josephine Paterson and Loretta Zderad | Humanistic Nursing Theory—focuses on the nurse and the patient; dignity, interests, and values are of greatest importance; belief that there is more to nursing that is not explainable by scientific principles. |
| 1978; 1991 | Madeline Leininger | Theory of Culture Care Diversity and Universality—a grand theory that considers the impact of culture on the person’s health and caring practices. |
| 1979 | Margaret Newman | Theory of Health as Expanding Consciousness—every person in every situation is ever-changing in a unidirectional, unpredictable, all-at-once pattern involving movement, time, space, and consciousness; emphasizes the importance of viewing patients in the context of their holistic patterns. |
| 1979 | Jean Watson | Theory of Human Caring—identifies 10 “carative” factors focusing on the interactions between the one who is caring and the one who is being cared for. |
| 1980 | Dorothy Johnson | Behavioral Systems Model—focuses on human behavior rather than the person’s state of health; this theory helped clarify the differences between medicine and nursing. |
| 1981 | Rosemarie Rizzo Parse | Theory of Human Becoming—focuses on the human-health-universe; views nursing as a participation effort with the patient that focuses on health. |
| 1983 | H. Erickson, E. Tomlin, and M. Swain | Modeling and Role Modeling Theory—uses the understanding of the patient’s world to plan interventions that meet the patient’s perceived needs and that will assist the patient to achieve holistic health; focus is on the person receiving the care, not the nurse, not the care, and not the disease. |
| 1984 | Pat Benner | Professional-Advancement-Model—applies the Dreyfus model of skill acquisition to nursing; area of concern is not how to do nursing but rather, “How do nurses learn to do nursing?”; identifies seven domains: practice-helping, teaching/coaching, diagnosing and monitoring, managing changes, administering and monitoring therapeutic interventions, monitoring quality care, and organizing to enact the work role. |
From Fawcett J: Analysis and evaluation of contemporary nursing knowledge: nursing models and theories, Philadelphia, FA Davis, 2005; Alligood MR, Marriner Tomey A: Nursing theorists and their work, ed 7, St. Louis, 2010, Mosby.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree