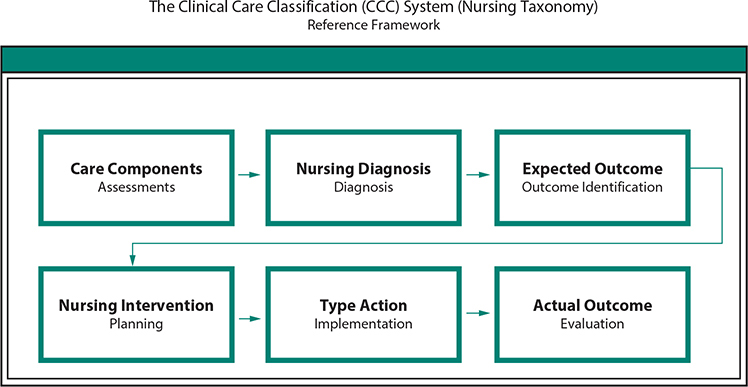
More than 4 million nurses, the largest segment of the United States healthcare sector, have indisputably demonstrated an ability to improve healthcare outcomes. The Health Information Technology for Economic and Clinical Health (HITECH) Act, part of the American Recovery and Reinvestment Act of 2009 (ARRA, PL 111-5), energized most healthcare facilities to implement healthcare information technology (HIT) and electronic health record (EHR) systems for processing patient care data as well as for reimbursement of patient care services. Today, national healthcare policy promotes substantial changes in healthcare delivery to obtain transparency in healthcare services and quality. The EHR system provides the bases for national data interoperability, and health information exchange (HIE). A minimum level of data quality in healthcare is essential to promote the necessary changes in performance delivery among the nation’s providers of care. For a transparent and complete healthcare communication as well as data quality, EHRs must collect, document, store, and retrieve standardized, coded nursing data concepts following the American Nurses Association (ANA) Nursing Process framework. A coded, structured nursing documentation standard is needed to exchange nursing communication to bring transparency to the contributions of nursing to patient care continuity and the quality of healthcare outcomes. With a successful HITECH incentive to implement EHRs, national HIT policy has turned to defining and promoting the “actionable” use of EHR data. Parasrampuria and Henry (2019) reported 94% of hospitals used EHR data to perform hospital processes that inform clinical practice. “The most common uses of EHR data in 2017 were supporting a continuous quality improvement process (82%), monitoring patient safety (81% of hospitals), and creating a dashboard with measures of organizational performance (77%). EHR data are least commonly used to develop an approach to query for patient data (51%), assess adherence to clinical practice guidelines (59%), and identify care gaps for specific patient populations (60%)”(p. 8). The current view among U.S. policy-makers is for the use of EHR data in actionable decision-making to persist and extend with implementation of the 21st Century Cures Act. The 21st Century Cures Act (Cures Act) and the Office of the National Coordinator for Health Information Technology (ONC) define interoperability in the context of health information technology as health IT that— (A) enables the secure exchange of electronic health information with, and use of electronic health information from, other health information technology without special effort on the part of the user; (B) allows for complete access, exchange, and use of all electronically accessible health information for authorized use under applicable State or Federal law; and (C) does not constitute information blocking as defined in section 3022(a). (ONC, 2018a, 2018b) (Office of the National Coordinator for Health Information Technology [ONC], 2018a, p. 3) With the passage of the 21st Century Cures Act (2016), current legislative initiatives and regulations are having a substantial impact on patient care and the professional nurses who lead the care team. As a result, there is an immediate need for structured nursing care data. The vision of ONC is a HIT system capable of exchanging data from various healthcare sources for clinical decision support. “Currently, there are more than 100 regional health information exchanges (HIEs) and multiple national level organizations that support exchange use cases” (ONC, 2018c, p. 3). In 2018, the ONC proposed Trusted Exchange Framework and Common Agreement (TEFCA) focused on healthcare data agreements to “enable stakeholders to exchange data across organizational boundaries. At this time, a single network is not feasible, since there are technical limitations, security concerns, variations in the participants being served in use cases, and resource limitations for each network; However, establishing a single ‘on ramp’ to Electronic Health Information that works regardless of one’s chosen network is feasible and achievable” (ONC, 2018c, p. 6). The TEFCA legislation establishes the HIE role of “Qualified Health Information Networks” (QHINs) to facilitate a standardized method for connectivity between and among HIEs through an administrative organization known as the Recognized Coordinating Entity (RCE). The RCE serves as the governing body to operationalize the Trusted Exchange Framework. The TEFCA legislation also specifies a common set of data classes for interoperable exchange known as the U.S. Core Data for Interoperability (USCDI). The TEFCA and USCDI are “the collaborative vehicles around which the industry can coalesce to identify the critical data needed to enable interoperability and achieve the goals outlined in the Cures Act” (ONC, 2018b, p. 3). In the USCDI there is a “Data Class” that is an aggregation of various Data Elements by a common theme or use case. A USCDI “Data Element” is the most granular level at which a piece of data is represented in the USCDI for exchange” (ONC, 2018d, p. 3). The usefulness of the USCDI is in defining what electronic healthcare data must be readily available for exchange. In defining the USCDI, the ONC has clarified the definition of interoperability in the Cures Act. The Version 1 USCDI data provided in the appropriate format must be available upon request based on the implementation of TEFCA. The USCDI Version 1 requires metadata (data about data) to understand when and who created the data. The data classes (when and who) were “included in the draft USCDI based on significant feedback from the industry post-2015 Edition rulemaking and Trusted Exchange Framework and Common Agreement stakeholder sessions” (ONC, 2018a, pp. 5–6). The USCDI also includes data classes for future inclusion identified as “Candidate Status.” For Candidate Status consideration a data class “must be clearly defined and have proven real-world applicability across a broad and diverse array of use cases, and substantial work in technical standardization has been or is actively being done by the industry” (ONC, 2018a, p. 7). Data classes may also be considered “Emerging.” The Emerging data classes are proposed and identified by stakeholders as crucial to the exchange of EHI for interoperability, although the priority of promotion of the data class to Candidate status is somewhat ambiguous. “In accordance with stakeholder feedback, ONC will consistently propose new data classes to be added to emerging status, thereby providing the industry with sufficient notice of what advancements lay ahead and allowing them appropriate time to react and prepare” (ONC, 2018a, p. 9). Note: During the USCDI initial public comment period, January 2018, a “Plan of Care” Data Class was proposed with the rational that a Plan of Care standard for interoperability is available (2009) from the Integrating the Healthcare Enterprise (IHE) (www.ihe.net) as part of the IHE Patient Care Coordination (PCC) Technical Framework. In most EHRs, the standard nursing data (sometimes called system nursing terminology, data dictionary, or nomenclature) is proprietary with a pre-existing data structure/framework. The proprietary HIT/EHR data framework acts as a barrier to nursing documentation by constraining the available concepts for nursing documentation and the nursing care plan fields. Without interoperable standardized, coded, electronic nursing care data concepts available for the documentation, nursing care become unstructured free-text and may not be recognized or included in coded HIEs. Due to the highly structured architectural designs of the today’s EHRs, by default, nursing practice is determined by the system’s terminology and ontology framework configuration, and nursing is constrained by the information model of a proprietary database, rather than nesting in flexible, portable, and universal nursing concepts enabling nurses and other clinical providers to improve population healthcare interventions, clinical practices, and patient care outcomes. In this chapter, the authors discuss (1) the framework of an electronic Nursing Plan of Care, (2) ANA Nursing Process, (3) Nursing Plan of Care operational requirements, (4) Transitions of Care using the coded concepts of the Clinical Care Classification (CCC) System and the CCC Information Model, and (5) Care Planning solutions for documenting nursing care, enhancing nursing data interoperability, and improving nursing workflows. Nursing “encompasses autonomous and collaborative care of individuals of all ages, families, groups and communities, sick or well and in all settings.” Nursing includes “The promotion of health, the prevention of illness, and the care of ill, disabled and dying people” (World Health Organization, 2019). Nursing care documentation is one of the most critical factors in a patient’s treatment and recovery to improve healthcare quality. Nurse executives continue to require hospitals to ensure nursing develops dynamic nursing plans of care for each patient. The nursing process is informed by patient’s values and provides the knowledge to participate with patients and others in changing health states, beliefs, and the quality of life. Nurses have long had a professional responsibility to advance knowledge that honors the patient’s meaning, reality, wishes, and choices and have meaningful relationships with clients. While the history of professional development of nursing observation documentation is important, the essential development of a planned, systematic Nursing Plan of Care (POC) advances the collection, storage, and retrieval of nursing data. The nursing care of individuals must be personalized. This personalization requires the Nursing Plan of Care to be refined in the current HIT and EHR systems to achieve optimal outcomes for specific patient needs (Whittenburg, Lekdumrongsak, Klaikaew, & Meetim, 2017). As nursing standards developed, nursing documentation conformed to the principles of the nursing process. Faye Abdellah, the first female U.S. Deputy Surgeon General, proposed nursing based on research and established the professional view that nurses use a problem-solving approach to practice beyond following medical orders. In 1981, Abdellah expanded the Nursing Process concept into a list of 21 unique nursing problems (Parascandola, 1994) and recognized that the care problems of a patient required nursing to modify care to meet an individual’s needs. In 1991, Carpenito cited the benefits of nursing care planning as (1) ability to provide written directions rather than verbal communication to reinforce patient safety in hand-offs of care, (2) ensure continuity of care, (3) prioritize patient problems, (4) provide a means to review and evaluate care, and (5) demonstrate the complex role of professional nurses in the health settings. Almost 25 years later, current legislation is bringing nurses closer to standard-based care planning. The ANA describes the common framework of professional nursing practice documentation as the Nursing Process. The Nursing Process is professional nursing’s foundation for the documentation of nursing care. In the EHR, nursing documentation is reused during the patient’s stay, over and over, with the documentation being done from the nursing assessment as if the documentation was a template. The Nursing Process is the framework and essential core of practice for the registered nurse to deliver holistic, patient-focused care (ANA, 2019). The Nursing Process encompasses all significant nursing actions—the process forms the foundation of the nurse’s professional practice and decision-making. In 1970, the ANA recommended the Nursing Process become the professional standard of nursing practice. The Nursing Process framework is based on the human existence “Needs Theory” adapted for nursing and nursing research. The nursing Needs Theory was first articulated in 1978 by Yura and Walsh (Lauri, Lepisto, & Kappeli, 1997). The Nursing Process is the total of nursing activities including assessment (identifying human needs), intervention (administering to human needs), and evaluation (validating the effectiveness of the help given). Yura and Walsh (1978, 1983), at the Catholic University of America, Washington, DC, reflected that human needs result from internal tension and organized a theory of nursing practice on the assumption that all basic human needs are relevant to nursing and all basic human needs are similar across all nursing practice areas. Yura and Walsh (1978) described four basic human needs applicable to patients in all nursing situations: (a) vital functions, (b) functional health status, (c) reactions to functional health status, and (d) environment. The six steps of the Nursing Process are as follows: (1) Assessment, (2) Diagnoses, (3) Outcome Identification, (4) Planning, (5) Implementation, and (6) Evaluation (Fig. 27.1). • FIGURE 27.1. Nursing Process Model (ANA, 1998). (Reproduced, with permission, from American Nurses Association. (2010). Nursing’s Social Policy Statement the Essence of the Profession, 3rd ed. (p. 23). Silver Springs, MD: nursesbooks.org. @2020 American Nurses Association.) Other characteristics of the Nursing Process framework include the following: Universally Applicable: Nursing Process framework is appropriate for any patient, of any age, with any clinical diagnosis, at any point on the health continuum and in any setting (e.g., school, clinic, hospital, or home) across all nurse specialties (e.g., hospice, maternity, pediatric, etc.). Goal-Oriented: Nursing Process interventions are determined by the nursing diagnoses and chosen for the purpose of achieving the nursing outcome. Cognitive Process: Nursing Process involves nursing judgment and decision-making. (Chapman, Ranzenberger, Killpack, & Pryor, 1984) In 1992, the ANA approved “Nursing Informatics” as a nursing specialty (Bickford, 2007) developing the Scope and Standards of Nursing Informatics Practice which endorsed the Nursing Process and six standards (phases/steps) of the Nursing Informatics (NI) practice (ANA, 2008, 2014). The theoretical framework for a fully operational Nursing Plan of Care is the Nursing Process, “the common thread uniting different types of nurses who work in various areas of nursing practice is the nursing process—the essential core of practice for the registered nurse to deliver holistic, patient-focused care” (“Nursing Process,” n.d., para. 1). In using the Nursing Process, the professional nurse is required to apply nursing knowledge systematically and logically to interpret, analyze, and use data to determine the appropriate plan of care based on knowledge of the physical, biological, and behavioral sciences. This knowledge of the basic sciences enables nurses to recognize patient problems and determine how the patient’s health is disrupted by a health problem. The 21st century use of an electronic Nursing Plan of Care supports the role of nursing as a caring profession contradicting the prevailing HIT/EHR image of nursing as a menudriven profession. The Nursing Process is the framework for the Nursing Plan of Care that requires the continual assessment and reassessment and evaluation of patient responses to nursing care and interventions to achieve expected nursing outcomes for patient care. The Nursing Process remains focused on Nursing Plan of Care of the patient and continually adapted to meet patient needs and concerns. The Nursing Plan of Care provides crucial information about patient care provided in healthcare facilities and the healthcare industry regardless of setting. The Plan of Care informs healthcare professionals about care delivery plans among nursing, allied health, and providers and supports an integration of care and an understanding of care effects on quality outcomes. The use of the nursing process to inform the Nursing POC focuses on nursing and greater accountability for individual nursing care actions regardless of whether the action is a mandatory action for regulatory, public disclosure, or quality measures with standardized care process activities. Nurses have the agency and ability to improve the quality of patient outcomes by maximizing data interoperability using the structured, coded nursing data elements so that nursing knowledge is accessible for nursing practice and documentation in the Nursing Plan of Care. As patients transition through the healthcare system, the Nursing Plan of Care is modified and communicated. This iterative Nursing POC supports a continuum of care, serves as a source of knowledge for healthcare providers, and may increase efficiency of patient care processes, improve healthcare data quality, and impact the cost of care across care settings by contributing to the evaluation of the efficacy of care interventions and treatment. In 1992, Saba adapted Nursing Process to provide a framework that focuses on patient care processes provided by nurses and allied health personnel in clinical practice settings (Saba, 2007). She defined it as follows: The nursing process operationalizes and demonstrates the art and science of nursing. The six steps of the nursing process describe the standard levels of nursing care and encompass all significant actions taken by nurses to provide care to patients/clients, and form the basis for clinical decision making. (p.152) Saba also adapted the Nursing Process as appropriate for a Nursing POC: During the Assessment phase, the professional nurse collects comprehensive data pertinent to the patient’s health or situation. The data is then analyzed to determine the patient Diagnoses or problems. The nurse then identifies the Expected Outcome or Goal for development of a plan of care (POC) individualized to the patient and situation. The plan is established that prescribes strategies and alternatives to attain the Expected Outcome for each Diagnosis. The nurse Implements the identified POC with ongoing Evaluation of progress toward the attainment of the identified Actual Outcome/Goal (Fig. 27.2). • FIGURE 27.2. The CCC System Framework Relationship to the Nursing Process (Saba, 2007). (Copyright © 2006 by Saba. Reprinted with permission.) Producing effective EHR systems for nursing requires a deep understanding of how nurses create and conduct cognitive documentation as well as task-oriented documentation. Most EHR systems dictate rather than adapt to nursing workflows and nursing information is not organized to fit the ANA model of care. The EHRs often assume a nursing care delivery model that is represented as algorithmic sequences of choices, yet nursing care is iterative with reformation of patient goals, revising interventions and actions, and updating care sequences with individual patients based on encountered condition changes and constraints. In the dictated workflow of EHRs, nursing data is collected as care assessments with nursing diagnoses, interventions, and actions in formats used to create single patient encounters. An electronic HIT/EHR Nursing Plan of Care based on the ANA Nursing Process framework for patient care complements the patient’s treatment plan and creates a healthcare environment of safety and patient-focused practice. Nursing documentation in structured text incorporating a standardized, coded, nursing terminology following the Nursing Process offers essential, useful, and a common representation for pertinent nursing documentation. The retrieval of nursing documentation can then be exchanged among HIEs for patient care continuity and outcomes analysis. Standardized nursing data allows information from disparate locations to deliver data for evidence-based practice to improve the nation’s health profile and the data quality of exchanged healthcare information. A Nursing POC using the CCC System as a data integrator and standard for the exchange of nursing documentation among and across health information record systems supports patient care continuity and a safe transition of patient care. The goal of nursing is to improve the health of communities, families, and individuals; then medical diagnoses cannot be expected to explain the nursing care of patients and cannot be the compelling framework for documenting patient care and professional nursing data. Nursing POC using the CCC System allows nurses to communicate the nursing diagnoses of patients, the nursing interventions performed, and resulting care outcomes. The CCC System is a “research-based, coded terminology standard that identifies the discrete data elements of nursing practice—the ‘essence of care’. The CCC System includes a holistic framework and coding structure of diagnoses, interventions, and outcomes for assessing, documenting, and classifying care in all healthcare settings” (Hunter & Bickford, 2011, p. 183). The CCC research project was conducted under a federal contract “to develop a methodology for classifying patients and measuring outcomes.” The research project represented every state in the United States, including Puerto Rico and the District of Columbia (Saba, 1992). The CCC System uses the six steps of the nursing process (Fig. 27.3) to describe professional nursing practice using a coding structure designed for processing nursing care data in HIT/EHR systems. (See www.clinicalcareclassification.com and Wikipedia.org/Clinical_Care_Classification_System.) • FIGURE 27.3. Clinical Care Classification (CCC) Information Model (Saba, 2007). (Copyright © 2006 by Saba. Reprinted with permission.) Another representation of the Nursing Process is shown in Fig. 27.4. The Clinical Decision Support view is consistent with Nursing Process content using a different more detailed visualization (Davis, 2018). • FIGURE 27.4. Clinical Decision Support Information Model. (From Davis, A. (2018). Clinical Decision Support Information Model©. Unpublished. Copyright © Davis, A., 2018.) CCC System Framework The CCC System Framework which expands the Nursing Process concepts of the ANA links together nursing diagnoses, nursing interventions, and nursing outcomes used to describe a patient encounter in the Clinical Care Classification System (Saba, 2007). The CCC System Information Model (Fig. 27.3) follows the six steps of the Nursing Process focusing on patient care provided by nurses and other healthcare professionals. “The measurement of nursing through the use of a standardized vocabulary leads to the development of large databases; and from these databases, evidence-based standards can be developed to validate the contribution of nurses to patient outcomes” (Rutherford, 2008, p. 2). The standardized, coded nursing concepts of the CCC System are Nursing Care Components, Nursing Diagnoses/Problems, Expected Outcomes (Goals), Nursing Interventions, and action types and Actual (Nursing Diagnosis) Outcomes. The CCC System uses a standardized framework consisting of 21 Care Components for classifying two interrelated terminologies: (1) CCC System of Nursing Diagnoses and Outcomes and (2) CCC of Nursing Interventions and Actions. The CCC System consists of four levels of healthcare that can be used to aggregate upward as well as downward. The CCC System codes the two terminologies to integrate the documentation of nursing concepts for an episode of illness (Saba, 2007). Care Components (21) Concepts designed to classify the patient’s signs/symptoms on admission. Nursing Diagnoses/Problems (176) Analysis of the patient’s signs/symptoms to determine the patient’s problems requiring therapeutic nursing care. Nursing Interventions/Actions (804) Atomic actions/services used for planning and implementing the therapeutic care of each patient problem. Each Nursing Intervention must also include one of four “Action Type Qualifiers.” Nursing Outcomes (528) Outcome qualifiers that depict the result of actual patient care are based on one of three conditions (Fig. 27.5). • FIGURE 27.5. The CCC System Framework (Saba, 2011). (Copyright © 2006 by Saba. Reprinted with permission.) The computable structure of the CCC System, which is in the public domain, promotes terminology upgrades to existing EHR nursing/clinical documentation systems. The implementation of structured, standardized, coded nursing terminology offers organizations a firm return on investment through transparency and insight into the intrinsic value of nursing care. The CCC System uses a fivecharacter alphanumeric structure to code the constructs of the two terminologies making standardized, coded nursing documentation possible to link and track the patient care process for an illness (Saba, 2007) (Figs. 27.6A,B). • FIGURE 26.6. The Five-Character Alphanumeric Structure of the Two CCC System Terminologies: (A) Diagnosis and (B) Intervention. (Copyright © 2006 by Saba. Reprinted with permission.) As early as Florence Nightingale, who was concerned with the lack of information about the patients under her care, can be considered as the first nursing researcher (Nightingale, 1860). A description of the effects of nursing practice on patients through research, that is, the analysis of standardized, coded nursing concepts, can benefit nursing practice. The importance of collected and analyzed nursing data can predict protocol and care processes. The CCC System concepts provide the structure for the documentation of a coded patient POC following the CCC Information Model. Once the Plan of Care has been implemented and tracked for a specific inpatient episode of illness, the POC nursing process codes for a given clinical/nursing condition can be summarized and analyzed providing different statistical solutions. The coded analysis for each of the six steps of the Nursing Process provides significant implications for Nursing Practice. For example, the interpretations of the POC four Action Types analytics about the Nursing Interventions have been used to measure the quality of care outcomes. The CCC Information Model’s structure is followed to create the patient’s Plan of Care using the four CCC Action Type Qualifiers (Monitor, Perform, Teach, and Manage). The Action Types clarify and expand the focus of the CCC Nursing Interventions (core). The CCC System Nursing Analytics of the CCC’s coded nursing concepts can be used to demonstrate a Nursing Plan of Care framework based on the CCC Information Model that provides reliable analytics which reflects the value and contribution of nursing to patient healthcare outcomes. The opportunities to integrate nursing information standards into EHR solutions to meet current information needs and challenges are appropriate in all care across the care continuum: (1) inpatient hospital stays, (2) community home health visits, and (3) outpatient encounters. Relevant clinical information documented by care team members, physicians, nurses, and other healthcare professionals contribute to the optimal outcome for a patient’s episode of care. Nurses assess (1) the healthcare problems, (2) goals of the proposed healthcare services, (3) medical and/or nursing orders for nursing care services, (4) actual nursing interventions combined with (5) each nursing intervention’s action type, and (6) the actual outcomes of the healthcare problem resulting from the therapeutic care. The use of coded nursing care interventions and actions tailored to the patient’s need for nursing care provide the evidence for which patient outcomes of the assessed diagnosis can be correlated and nursing care value can be calculated. In a Nursing POC example for a patient admitted with pneumonia using the CCC-coded documentation, the coded care data can be depicted using tables and graphs. The frequencies and other statistical solutions describe and predict the protocols of nursing care practices. The analytics supports the value of the care as well as demonstrates the effectiveness of implementing the CCC System–coded nursing concepts in a Nursing POC. Table 27.1 provides the distributions of the nursing intervention/actions for each nursing diagnosis carried out to treat the sample pneumonia patient’s nursing diagnoses. The nursing diagnoses can provide the disease condition (pneumonia) but combined with nursing interventions/actions can represent an evidence-based protocol for Nursing POC of a pneumonia patient. TABLE 27.1. Frequency of Nursing Interventions by Nursing Diagnosis for an Inpatient Hospitalization
27
Nursing Plan of Care Framework for HIT
INTRODUCTION
Background
Nursing Process Foundation

Nursing Plan of Care Framework
NURSING PROCESS AND HIT/EHR SYSTEMS
Transitions of Care Using the CCC System




NURSING POC ANALYTIC MODEL
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


