CHAPTER 6 Nursing patients with disorders of the immune system
Introduction
The defence mechanisms providing immunity include: physical, chemical and microbiological barriers, second-line non-specific defences and specific immune responses (Storey & Jordan 2008). These can be categorised as first-, second- and third-line defences (Figure 6.1):
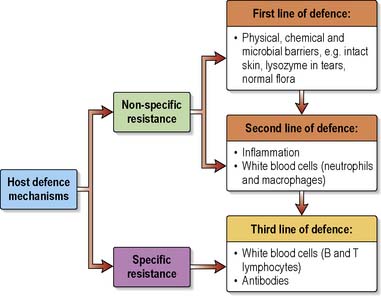
Figure 6.1 Overview – first-, second- and third-line defence mechanisms.
(Reproduced from Rennie-Meyer 2007.)
For the most part the immune system functions to protect individuals from microbes and infection (see Ch. 16), and natural killer (NK) cells (a type of lymphocyte) undertake immunological surveillance in order to detect and destroy foreign, infected, damaged or cancerous cells. However, abnormalities may occur and immune responses may be excessive (hypersensitivity), may fail to function properly (immunodeficiency) or may fail to recognise ‘self’ leading to an immune attack on body cells (autoimmune disorders).
This chapter outlines immune responses, concentrating on adaptive immunity, and describes the nursing management of some immune response disorders: hypersensitivity, immunodeficiency and autoimmune conditions. It will come as no surprise that problems of the immune system impact on all body systems. Nurses working in all areas of practice may encounter people with immune disorders. Readers are provided with cross references to relevant chapters (e.g. Chs 5, 11, 16, 31), and suggestions for further reading.
Components and features of the immune system – an overview
Bone marrow and thymus
Lymphocytes develop in the bone marrow (see Ch. 11) but require further processing to form the two functionally different groups, B and T lymphocytes. The T lymphocytes are so called because they are processed in the thymus gland, which lies behind the sternum in the mediastinum and extends into the neck. Well developed in infants, it reaches maximum size at puberty, thereafter becoming smaller as lymphoid tissue is replaced by fat.
Types of immunity
This part of the chapter outlines natural non-specific immunity and considers both types of adaptive specific immunity. Table 6.1 contrasts the features of natural and adaptive immunity. As mentioned earlier there is considerable interaction between natural and adaptive immunity, and between both parts of adaptive immune responses. For example, tissue macrophages engulf antigens and act as antigen-presenting cells (APCs), which stimulate T-lymphocyte responses.
Table 6.1 Contrasting the features of adaptive and natural immunity
| Feature | Natural Non-Specific Immunity | Adaptive Specific Immunity |
|---|---|---|
| Resistance | Unaltered response on further exposure to the antigen. No ‘memory’ | Improved by repeated infection, i.e. has ‘memory’ |
| Sensitivity | Generally effective against all organisms. Cannot recognise specific antigens | Specific for the stimulating antigen |
| Major cell types | Phagocytes – neutrophils, monocytes, macrophages Natural killer (NK) cells | B and T lymphocytes (macrophages act as APCs in cell-mediated immunity) |
| Important chemicals | Complement proteins Lysozyme (antibacterial enzyme) Cytokines, e.g. interferons (IFNs) Acute phase proteins Inflammatory mediators, e.g. histamine, bradykinin | Antibodies (immunoglobulins) Other cytokines produced by lymphocytes (sometimes called lymphokines) |
Note. Natural non-specific immunity is more primitive in evolutionary terms, and the mechanisms of adaptive specific immunity are directed to amplifying and increasing the efficiency of the mechanisms of natural immunity.
(adapted from Staines et al 1993)
Information about the numerous cells and chemicals involved in immune responses is provided in Box 6.1.
Box 6.1 Information
Cellular and chemical components of the immune responses
Cells – white blood cells (leucocytes) (see Ch.11 for further information)
Chemicals
Natural non-specific immunity
Natural non-specific immunity represents first- and second-line body defences (see Figure 6.1) and includes: intact skin/mucosae, specialised epithelial surfaces, body secretions containing antibacterial substances such as lysozyme and immunoglobulins (Storey & Jordan 2008) (Box 6.2) and the microorganisms that comprise the normal flora. The processes of inflammation (see Ch. 23) and phagocytosis (engulfing and destroying foreign particles by white blood cells) are also included (see Further reading, e.g. Waugh & Grant 2010). These defences can be breached in a number of situations, for example when skin is inflamed or damaged (see Ch. 12).
Box 6.2 Information
Adaptive specific immunity
Humoral (antibody-mediated) immune response
Antibodies (immunoglobulins)
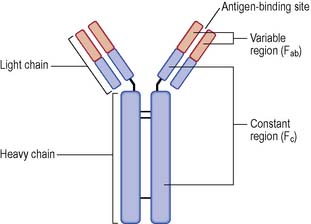
Antibodies are globular proteins with the ability to recognise and bind to a specific antigen, usually a microorganism. They are produced by plasma cells and, once formed, circulate in the blood and other body fluids. Antibodies are characteristically Y-shaped, with two identical heavy chains, each connected to two identical light chains (Figure 6.2).
They have many roles that include:
Each of the five classes may be produced with specificity for a single antigen. Their structure varies according to function and they are present in different amounts in the blood and other body fluids (Box 6.3).
Box 6.3 Information
Classes of antibodies (immunoglobulins)
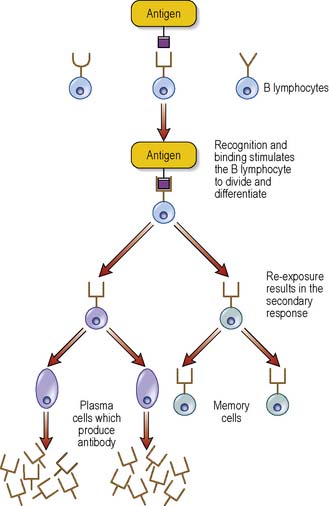
Primary and secondary antibody-mediated immune response
Primary response
Cell-mediated immune response
Cell-mediated immunity comprises T-lymphocyte-dependent responses directed against foreign cells/tissue (such as in transplant rejection), microorganisms that invade the host cells (viruses, fungi, parasites), phagocytosis-resistant bacteria and cancer cells. T lymphocytes are described as being thymus dependent (see p. 178). They are also antigen specific, have an antigen receptor and are capable of ‘memory’.
There are several subsets of T lymphocytes (cells):
Box 6.4 provides further information on the T-cell subsets.
Box 6.4 Information
(adapted from Brooker 2010 with permission)
T-cell subsets
T-cell subsets are also classified according to their surface molecules, i.e. the glycoproteins CD4 or CD8. T-helper cells are designated CD4+; T-cytotoxic cells and T-suppressor cells are CD8+. The level of CD4+ cells and the ratio of CD4+ to CD8+cells are used when assessing the immune system in people with HIV disease (see Ch. 35) or other viral infections and following organ transplant.
T cells function in a variety of ways:
Immunity against infectious disease
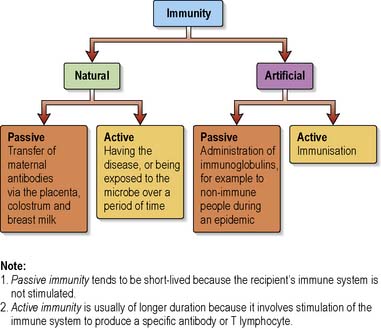
Immunity to a specific infectious disease may be due to inherited qualities. Otherwise immunity develops by natural processes or is achieved by artificial means, i.e. vaccines. Both natural and artificial immunity may be passive or active (Figure 6.4).
Natural immunity
Active natural immunity is acquired if the person has the specific infection. Because this involves the production of a specific antibody or T lymphocyte, active immunity tends to be of longer duration (see primary and secondary response, p. 181).
Artificial immunity
involves processes whereby immunity is initiated or augmented. Passive artificial immunity is achieved by the administration of immunoglobulins (usually obtained from the plasma of immune individuals). There are normal immunoglobulins produced from pooled plasma and disease-specific immunoglobulins including those for rabies, tetanus, hepatitis B and varicella-zoster. Immunoglobulins are used in disease outbreaks, e.g. measles, to protect non-immune individuals, or in the prophylaxis and/or management of specific diseases such as for people with tetanus-prone wounds. Passive immunity is short-lived because the person’s immune system is not stimulated to produce specific antibodies (see Further reading, e.g. Health Protection Agency 2008, Provan et al 2008). Note. Immunoglobulins obtained from animals (antisera) can result in serious allergic reactions, including serum sickness, and have largely been replaced by human immunoglobulins.
Active artificial immunity is achieved by immunisation and, because this involves the production of a specific antibody or T lymphocyte, tends to be of longer duration (see primary and secondary response, p. 181).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree