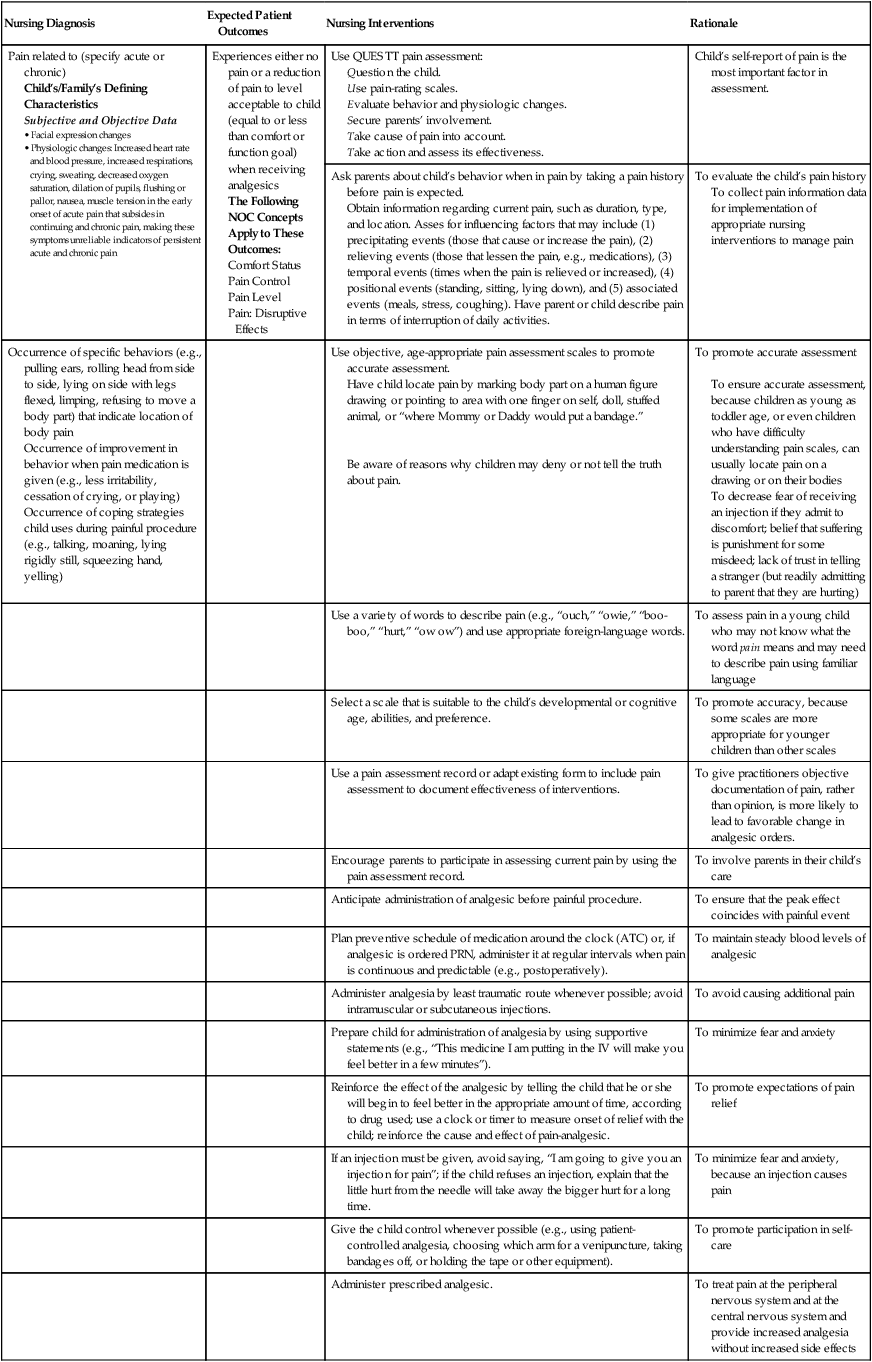
Pain related to (specify acute or chronic)
Child’s/Family’s Defining Characteristics
Subjective and Objective Data
|
Experiences either no pain or a reduction of pain to level acceptable to child (equal to or less than comfort or function goal) when receiving analgesics
The Following NOC Concepts Apply to These Outcomes:
|
Use QUESTT pain assessment:
Question the child.
Use pain-rating scales.
Evaluate behavior and physiologic changes.
Secure parents’ involvement.
Take cause of pain into account.
Take action and assess its effectiveness. |
Child’s self-report of pain is the most important factor in assessment. |
Ask parents about child’s behavior when in pain by taking a pain history before pain is expected.
Obtain information regarding current pain, such as duration, type, and location. Asses for influencing factors that may include (1) precipitating events (those that cause or increase the pain), (2) relieving events (those that lessen the pain, e.g., medications), (3) temporal events (times when the pain is relieved or increased), (4) positional events (standing, sitting, lying down), and (5) associated events (meals, stress, coughing). Have parent or child describe pain in terms of interruption of daily activities. |
To evaluate the child’s pain history
To collect pain information data for implementation of appropriate nursing interventions to manage pain |
Occurrence of specific behaviors (e.g., pulling ears, rolling head from side to side, lying on side with legs flexed, limping, refusing to move a body part) that indicate location of body pain
Occurrence of improvement in behavior when pain medication is given (e.g., less irritability, cessation of crying, or playing)
Occurrence of coping strategies child uses during painful procedure (e.g., talking, moaning, lying rigidly still, squeezing hand, yelling) |
|
Use objective, age-appropriate pain assessment scales to promote accurate assessment.
Have child locate pain by marking body part on a human figure drawing or pointing to area with one finger on self, doll, stuffed animal, or “where Mommy or Daddy would put a bandage.”
Be aware of reasons why children may deny or not tell the truth about pain. |
To promote accurate assessment
To ensure accurate assessment, because children as young as toddler age, or even children who have difficulty understanding pain scales, can usually locate pain on a drawing or on their bodies
To decrease fear of receiving an injection if they admit to discomfort; belief that suffering is punishment for some misdeed; lack of trust in telling a stranger (but readily admitting to parent that they are hurting) |
|
|
Use a variety of words to describe pain (e.g., “ouch,” “owie,” “boo-boo,” “hurt,” “ow ow”) and use appropriate foreign-language words. |
To assess pain in a young child who may not know what the word pain means and may need to describe pain using familiar language |
|
|
Select a scale that is suitable to the child’s developmental or cognitive age, abilities, and preference. |
To promote accuracy, because some scales are more appropriate for younger children than other scales |
|
|
Use a pain assessment record or adapt existing form to include pain assessment to document effectiveness of interventions. |
To give practitioners objective documentation of pain, rather than opinion, is more likely to lead to favorable change in analgesic orders. |
|
|
Encourage parents to participate in assessing current pain by using the pain assessment record. |
To involve parents in their child’s care |
|
|
Anticipate administration of analgesic before painful procedure. |
To ensure that the peak effect coincides with painful event |
|
|
Plan preventive schedule of medication around the clock (ATC) or, if analgesic is ordered PRN, administer it at regular intervals when pain is continuous and predictable (e.g., postoperatively). |
To maintain steady blood levels of analgesic |
|
|
Administer analgesia by least traumatic route whenever possible; avoid intramuscular or subcutaneous injections. |
To avoid causing additional pain |
|
|
Prepare child for administration of analgesia by using supportive statements (e.g., “This medicine I am putting in the IV will make you feel better in a few minutes”). |
To minimize fear and anxiety |
|
|
Reinforce the effect of the analgesic by telling the child that he or she will begin to feel better in the appropriate amount of time, according to drug used; use a clock or timer to measure onset of relief with the child; reinforce the cause and effect of pain-analgesic. |
To promote expectations of pain relief |
|
|
If an injection must be given, avoid saying, “I am going to give you an injection for pain”; if the child refuses an injection, explain that the little hurt from the needle will take away the bigger hurt for a long time. |
To minimize fear and anxiety, because an injection causes pain |
|
|
Give the child control whenever possible (e.g., using patient-controlled analgesia, choosing which arm for a venipuncture, taking bandages off, or holding the tape or other equipment). |
To promote participation in self-care |
|
|
Administer prescribed analgesic. |
To treat pain at the peripheral nervous system and at the central nervous system and provide increased analgesia without increased side effects |
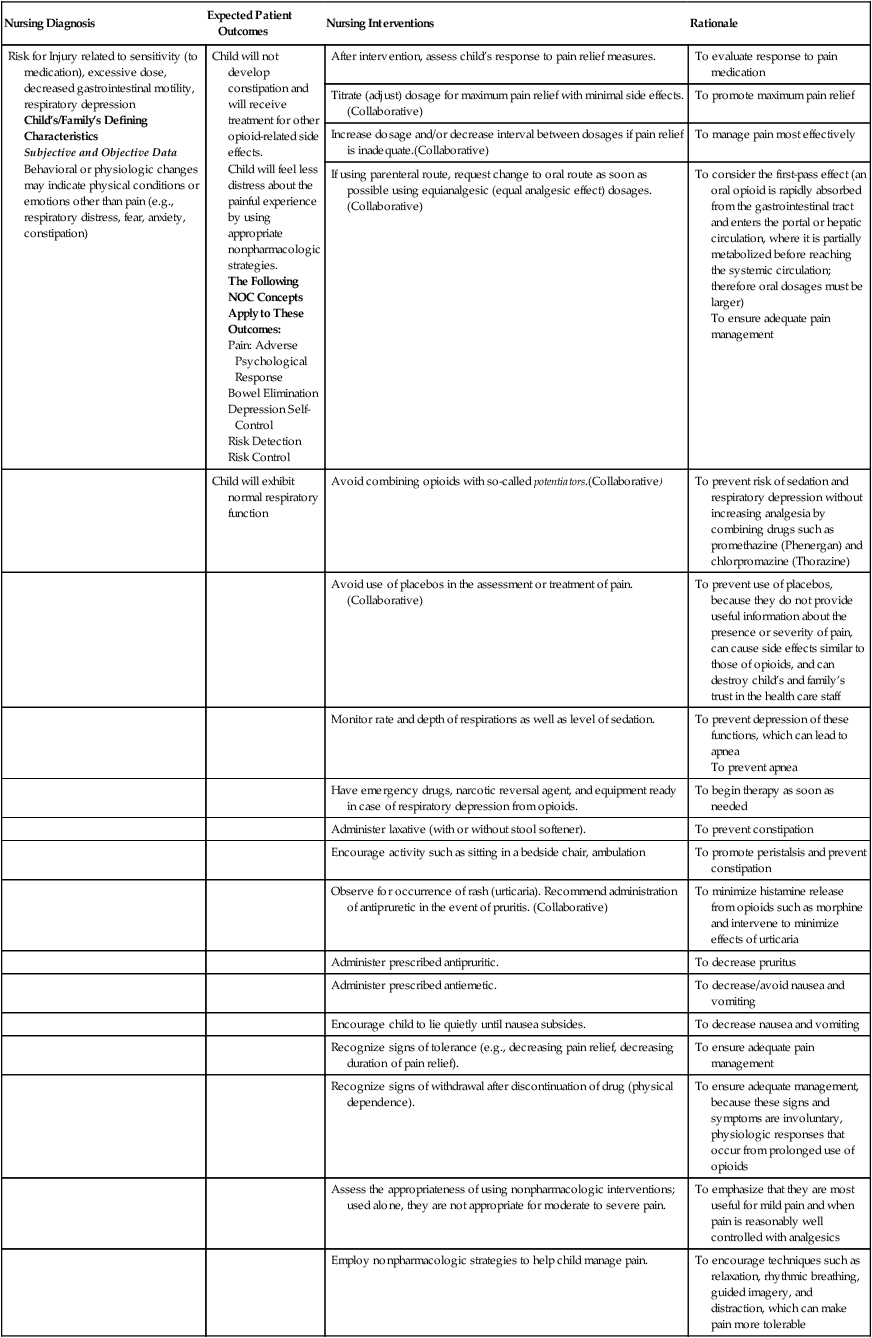
Risk for Injury related to sensitivity (to medication), excessive dose, decreased gastrointestinal motility, respiratory depression
Child’s/Family’s Defining Characteristics
Subjective and Objective Data
Behavioral or physiologic changes may indicate physical conditions or emotions other than pain (e.g., respiratory distress, fear, anxiety, constipation) |
Child will not develop constipation and will receive treatment for other opioid-related side effects.
Child will feel less distress about the painful experience by using appropriate nonpharmacologic strategies.
The Following NOC Concepts Apply to These Outcomes:
|
After intervention, assess child’s response to pain relief measures. |
To evaluate response to pain medication |
Titrate (adjust) dosage for maximum pain relief with minimal side effects.(Collaborative) |
To promote maximum pain relief |
Increase dosage and/or decrease interval between dosages if pain relief is inadequate.(Collaborative) |
To manage pain most effectively |
If using parenteral route, request change to oral route as soon as possible using equianalgesic (equal analgesic effect) dosages. (Collaborative) |
To consider the first-pass effect (an oral opioid is rapidly absorbed from the gastrointestinal tract and enters the portal or hepatic circulation, where it is partially metabolized before reaching the systemic circulation; therefore oral dosages must be larger)
To ensure adequate pain management |
|
Child will exhibit normal respiratory function |
Avoid combining opioids with so-called potentiators.(Collaborative) |
To prevent risk of sedation and respiratory depression without increasing analgesia by combining drugs such as promethazine (Phenergan) and chlorpromazine (Thorazine) |
|
|
Avoid use of placebos in the assessment or treatment of pain. (Collaborative) |
To prevent use of placebos, because they do not provide useful information about the presence or severity of pain, can cause side effects similar to those of opioids, and can destroy child’s and family’s trust in the health care staff |
|
|
Monitor rate and depth of respirations as well as level of sedation. |
To prevent depression of these functions, which can lead to apnea
To prevent apnea |
|
|
Have emergency drugs, narcotic reversal agent, and equipment ready in case of respiratory depression from opioids. |
To begin therapy as soon as needed |
|
|
Administer laxative (with or without stool softener). |
To prevent constipation |
|
|
Encourage activity such as sitting in a bedside chair, ambulation |
To promote peristalsis and prevent constipation |
|
|
Observe for occurrence of rash (urticaria). Recommend administration of antipruretic in the event of pruritis. (Collaborative) |
To minimize histamine release from opioids such as morphine and intervene to minimize effects of urticaria |
|
|
Administer prescribed antipruritic. |
To decrease pruritus |
|
|
Administer prescribed antiemetic. |
To decrease/avoid nausea and vomiting |
|
|
Encourage child to lie quietly until nausea subsides. |
To decrease nausea and vomiting |
|
|
Recognize signs of tolerance (e.g., decreasing pain relief, decreasing duration of pain relief). |
To ensure adequate pain management |
|
|
Recognize signs of withdrawal after discontinuation of drug (physical dependence). |
To ensure adequate management, because these signs and symptoms are involuntary, physiologic responses that occur from prolonged use of opioids |
|
|
Assess the appropriateness of using nonpharmacologic interventions; used alone, they are not appropriate for moderate to severe pain. |
To emphasize that they are most useful for mild pain and when pain is reasonably well controlled with analgesics |
|
|
Employ nonpharmacologic strategies to help child manage pain. |
To encourage techniques such as relaxation, rhythmic breathing, guided imagery, and distraction, which can make pain more tolerable |
|
|
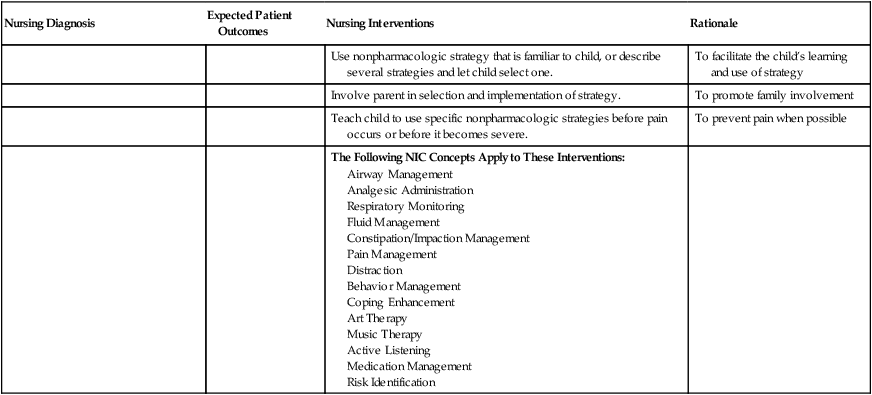
Use nonpharmacologic strategy that is familiar to child, or describe several strategies and let child select one. |
To facilitate the child’s learning and use of strategy |
|
|
Involve parent in selection and implementation of strategy. |
To promote family involvement |
|
|
Teach child to use specific nonpharmacologic strategies before pain occurs or before it becomes severe. |
To prevent pain when possible |
|
|
The Following NIC Concepts Apply to These Interventions:
|
|
![]()