Chapter 31 2. Walks up and down stairs, one step at a time, holding onto rail 3. Builds tower of six to seven cubes; uses cubes to form a train D Vocalization and socialization A Toilet training: most important integrative task for toddler 1. Physical maturation must be reached before training is possible; approach and attitude of parents play vital role a. Sphincter control adequate when child can walk b. Can retain urine for at least 2 hours c. Usual age for bowel training is 22 to 30 months d. Daytime bowel and bladder control usually after 2 years of age e. Night control usually several months to years after achievement of daytime control; if night wetting persists to 6 years of age, investigation into cause is indicated a. Usually begins with bowel, then bladder; potty chair helpful so feet touch floor b. Intermittent periods of urination and fecal soiling B Need for autonomy: parents should support independence without overprotection A Plays alongside other children but not with them B Mostly free and spontaneous, no rules C Short attention span, requires frequent change of toys D Dangers associated with toys 1. Breaks toy through exploration and ingests small pieces 2. Ingests lead from lead-based paint on toys E Imitation and make-believe play begins by age 3 years 1. Adequate nutrient intake to meet continuing growth and developmental needs 2. Sufficient calories for increasing physical activity and energy needs 3. Consumption of fresh, rather than processed, foods (e.g., fruits, vegetables) 4. Psychosocial development in relation to food patterns, eating behavior, attitudes 1. Reflects patterns and preferences of culture, parents, and siblings 2. Calorie and nutrient requirements increase with age, despite slower growth 3. Increased variety in types and textures of foods; provision of choices to address growing independence 4. Increased involvement in feeding process; stimulation of curiosity about food environment; language learning 2. Prefers sweet drinks; juices should be limited to 4 ounces (120 mL) or less per day to prevent dental caries 3. TV commercials influence selection of foods (e.g., fast foods, “empty-calorie” snacks, high-carbohydrate convenience foods) 1. Anemia: increased need for foods containing iron (e.g., enriched cereals, meat, eggs, green vegetables); chewable iron-fortified vitamins; if liquid, iron supplements should be diluted and sipped through a straw; administer with vitamin C–containing beverage to promote absorption 2. Obesity or underweight: increased or decreased caloric intake; need for nutritional counseling 3. Low intake of calcium, iron, vitamins A and C may need supplementation 4. Mealtime struggles related to increased autonomy and parental attitudes toward food (e.g., “eat everything on plate”; “try new food”; “no dessert unless …”); need for parental counseling A Leading cause of death in children between 1 and 4 years of age B Incidence: children younger than 5 years of age account for more than half of all accidental deaths during childhood; more than half of accidental child deaths related to automobiles and fire C Accidents related to stage of growth and development; curiosity about environment a. Walking or running, especially chasing after objects thrown into street b. Inability to determine speed; lack of experience to foresee danger c. Out of sight because of small size; can be hit by car backing out of driveway or when playing in leaves or snow d. Failure to restrain in car (e.g., sitting in person’s lap; incorrect use of seat belt on car restraint) a. Investigating: pulls pot off stove; plays with matches; inserts object into wall socket b. Climbing: reaches stove, oven, ironing board and iron, objects on tables a. Developing fine motor skills; able to open bottles, cabinets, jars b. Climbing to previously unreachable shelves and cabinets c. Learning new tastes and textures; uses mouth to identify and explore objects; finds and eats/drinks what is within reach (e.g., cleaning products, medications) 5. Interested in body openings A Experiences basic fears of loss of love, of unknown, of punishment B Immobilization and isolation influence physical (particularly neurologic) and psychosocial development C Regression to earlier behaviors may occur D Stages of separation anxiety A Prepare parents and child for hospitalization 1. Promote parent-child relationship by limiting separation (open visiting hours have reduced incidence of separation anxiety) 2. Prepare minimally for hospitalization because of limited cognitive ability to grasp verbal explanation 3. Determine routines and rituals concerning toilet training, feeding, bathing, sleep pattern; incorporate into the plan of care 4. Ask parents to bring child’s favorite items from home (e.g., blanket, toy, bottle, pacifier) 5. Prepare parents for child’s reaction to separation; pounding toys helps release anger associated with temper tantrums or separation 6. Prepare parents for child’s regression to previous modes of behavior and loss of newly learned skills B Minimize separation anxiety and other emotional traumas during hospitalization a. Encourage to stay with child in hospital; if possible, have one parent room-in throughout hospitalization b. If not rooming-in, encourage frequent visits; explain that frequent visits for short periods of time are more therapeutic than one long visit c. Associate visits with familiar events, such as “Mommy is coming after lunch” d. If unable to visit, establish contact by phone and/or computer which enables visualization (e.g., Skype); be alert for behavioral changes when parents cannot stay or visit child 2. Parental involvement with care 1. Plan for consistent caregiver, as much as possible, who can offer individual attention, physical touch, and sensory stimulation 2. Establish routine similar to home routine by continuing rituals and providing favorite items from home 3. Maintain familiarity with home by talking about parents, having child listen to tape recordings of family members’ voices, showing photographs of family members 4. When family members leave, stay to provide comfort to child and to reassure parents 5. Accept regression; avoid teaching new skills 6. Encourage release of tension, especially aggression, through play (e.g., knocking blocks over, scribbling on paper, peg and pounding board) 7. Comfort when sedation is necessary during procedures (e.g., CT scan, MRI) 1. Affects more children in United States than any other chronic infectious disease (five times more common than asthma) 2. By age 17 more than 7% of adolescents have lost at least one permanent tooth to decay B Risk factors: poverty, disability, HIV infection, inadequate diet, inadequate dental hygiene C Clinical finding if untreated 1. Teach parents to start cleaning teeth when they first erupt; use clean, damp cloth 2. Teach parents care of teeth beginning at 2 years of age b. Begin using pea-size amount of toothpaste with fluoride, if needed c. Brush twice a day, beginning at 2 years of age 3. Encourage parents to offer nutritious meals and snacks; limit sweet juices (120 mL per day) 4. Instruct parents to take child for first dental exam between 1 and 2 years of age, then every six months 5. Recommend that parents discuss fluoride supplementation and dental sealants with health care provider (See Chapter 10, Nursing Care of Clients With Integumentary system Disorders, Burns, for additional information) A Incidence: third leading cause of unintentional injury and related death among children 14 years of age and younger B Risk factors: younger than 5 years of age, limited control of environment, minimal ability to act promptly and appropriately (See Chapter 10, Nursing Care of Clients With Integumentary system Disorders, Burns, Data Base) b. Fluid loss from nonprotected skin c. Circulatory stasis usually restored within 24 to 48 hours in partial-thickness burns a. “Burn shock” causes precipitous drop in cardiac output; restored in 24 to 36 hours c. Physiologic stress response d. Paralytic ileus may develop e. Anemia: initially, elevated hematocrit because fluid shifts from intravascular space; later, increased red cell fragility contributes to decreased RBC life span g. Post-burn growth retardation: severe growth delays in height and weight if burn is greater than 40% TBSA; growth lag may last for up to 3 years 2. First aid administered promptly b. Superficial burns: cleansed, sterile dressing soaked in sterile saline applied, if possible; avoidance of creams, butter, or household remedies c. Severe burns (more than 10% of body): oral fluids withheld 3. Transportation to appropriate health care facility as quickly as possible a. Large body surface area in proportion to weight results in greater potential for fluid loss b. Shock: primary cause of death in first 24 to 48 hours 4. Treatment of fluid and electrolyte loss a. Greatest in first 24 to 48 hours because of tissue damage b. Immediate replacement of fluids and electrolytes c. Monitoring of hematocrit, hemoglobin, and blood chemistry levels provide guide for fluid replacement 5. Tetanus prophylaxis as needed 1. Maintain fluids and electrolytes a. Administer prescribed fluids meticulously, both in time and in volume b. Monitor fluid status (e.g., daily weights, I&O, weigh diapers) 2. Maintain NPO if paralytic ileus occurs 4. Maintain standard precautions; use personal protective equipment 5. Meet psychosocial needs of child who is isolated from others a. Recognize that isolation may provoke feelings of guilt and punishment b. Recognize that children younger than 5 years of age are frightened by isolation and personal protective equipment c. Recognize that touch needed for comfort and security may now be painful; reestablish pleasurable touch (e.g., apply lotion to unaffected areas); maximize use of other senses to promote security and comfort d. Encourage child to express feelings verbally, or through play, if possible 6. Provide for adequate nutrition a. Consider that initial hypometabolic state is followed by hypermetabolic state (begins about fifth day post injury), causing decreased lean body mass, muscle weakness, immunodepression, inadequate wound healing b. Offer diet high in protein, vitamins, calories; should be started immediately after paralytic ileus resolves c. Encourage eating; may be anorectic because of discomfort, isolation, depression, fear d. Take advantage of food preferences when feasible; avoid forcing to eat or using food as a weapon; encourage parent participation e. Alter diet as needs change, especially when high-calorie foods are no longer needed f. Provide care related to tube feeding if unable to eat (e.g., assess for gastric return and residual before feeding, ensure tube is cleared after feeding with predetermined amount of water) a. Make moving a game; initiate play that uses affected part (e.g., throwing ball for arm movement) b. Maintain functional body alignment c. Perform passive exercises during bath or whirlpool treatments a. Encourage to play with gown, mask, gloves, bandages b. Prepare for baths and whirlpool treatments, which can be frightening and painful c. Encourage to reenact treatments and care to work through feelings d. Help to cope with changes in body (1) Younger child: support parents whose reactions are communicated (2) Older child, especially during adolescence when body appearance is of great concern: devise ways to conceal affected areas, especially when peers visit; emphasize how to improve looks (e.g., wigs, cosmetics, clothing, eventual plastic surgery) 9. Teach prevention of burn injuries a. Educate children regarding fire safety (1) Teach to leave house as soon as smoke is smelled or flames are seen, without stopping to retrieve pet or toy (2) Involve all family members in fire drills (3) Demonstrate and practice “stop, drop, and roll” rather than running if clothes are on fire b. Educate parents in regard to their child’s growth and development, about specific dangers at each age level c. Educate parents how to prevent burns in the home A Ingestion of/exposure to toxic substance; ingestion of excessive amount of nontoxic substance B Incidence: more than 90% occur in home C Risk factors: younger than 4 years of age; inadequate storage of toxic or potentially toxic substances D Most commonly ingested substances 1. Cosmetics and personal care products (e.g., perfume, aftershave) 2. Cleaning products (e.g., household bleach, disinfectants) 3. Plants (e.g., nontoxic gastrointestinal irritants, oxalates) 4. Medications: prescribed, over-the-counter (OTC) (e.g., acetaminophen, ibuprofen), for pets 5. Foreign bodies, toys, miscellaneous (e.g., thermometer, bubble blowing solution) a. Empty mouth of pills, plant parts, other material b. Flush eyes with tap water if necessary c. Flush skin, wash with soap and soft cloth d. Remove clothing, especially if exposed to pesticide, acid, alkali, or hydrocarbon a. Call poison control center, emergency facility, clinic, or health care provider for immediate advice regarding treatment b. Save all evidence of poison (e.g., container, vomitus, urine) a. Aspiration of low-viscosity hydrocarbon (e.g., gasoline, lighter fluid, mineral seal oil [found in furniture polishes]): vomiting can cause severe chemical pneumonitis b. Ingestion of strong corrosive (e.g., acid or alkali, such as drain cleaners, bleach, electric dishwasher detergent, batteries): emesis of corrosive reinjures mucosa of esophagus and pharynx a. Administer activated charcoal (1 g/kg of body weight), if possible within 1 hour of ingestion; can be effective within 4 hours of ingestion of injurious substance b. Prepare equipment for gastric lavage if within 1 hour of ingestion 5. Prevent aspiration when vomiting 6. Provide care for latent manifestations of poisoning b. Treat appropriately (e.g., institute seizure precautions, keep warm, position for shock; reduce temperature if hyperpyretic) 8. Teach parents prevention of poisoning a. Institute anticipatory guidance based on child’s age and developmental level b. Refer to appropriate agency for evaluation of home environment and need for safety measures c. Provide assistance with environmental manipulation when needed d. Emphasize importance of safe storage of all substances e. Teach children about hazards of ingesting nonfood items f. Caution against keeping large amounts of medicines on hand g. Discourage transferring medications to containers without safety caps 1. First 2 to 4 hours: nausea, vomiting, profuse diaphoresis, pallor 2. Latent period (24 to 36 hours): symptoms subside; slow, weak pulse 3. Hepatic involvement (may last up to 7 days or be permanent): pain in right upper quadrant, jaundice, confusion, stupor, coagulation abnormality 4. Gradual recovery if death does not occur during hepatic coma
Nursing Care of Toddlers
Growth and Development
Developmental Timetable
Fifteen Months
Eighteen Months
Two Years
Major Learning Events
Health Promotion of Toddlers
Play During Toddlerhood (Parallel Play)
Childhood Nutrition
Injury Prevention during Toddlerhood
Hospitalization of Toddlers
Data Base
General Nursing Care of Toddlers
Health Problems Most Common in Toddlers
Tooth Decay (Dental Caries)
Data Base
Nursing Care of Children with Tooth Decay
Planning/Implementation
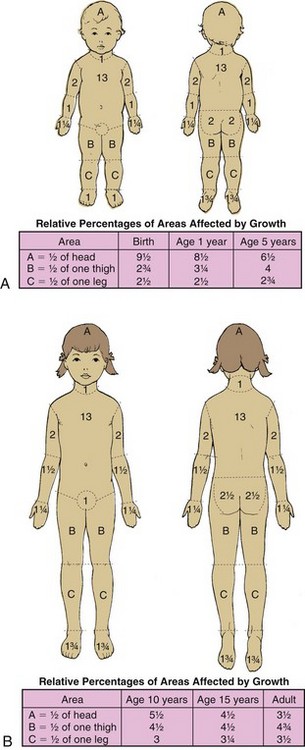
Burns
Data Base
Nursing Care of Children with Burns
Planning/Implementation
Poisoning
Data Base
General Nursing Care of Children with Poisoning
Planning/Implementation
Acetaminophen Poisoning
Data Base
Salicylate Poisoning and Toxicity
Data Base
Nursing Care of Children with Salicylate Poisoning
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nursing Care of Toddlers
Get Clinical Tree app for offline access