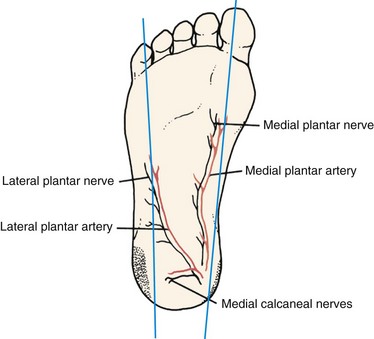
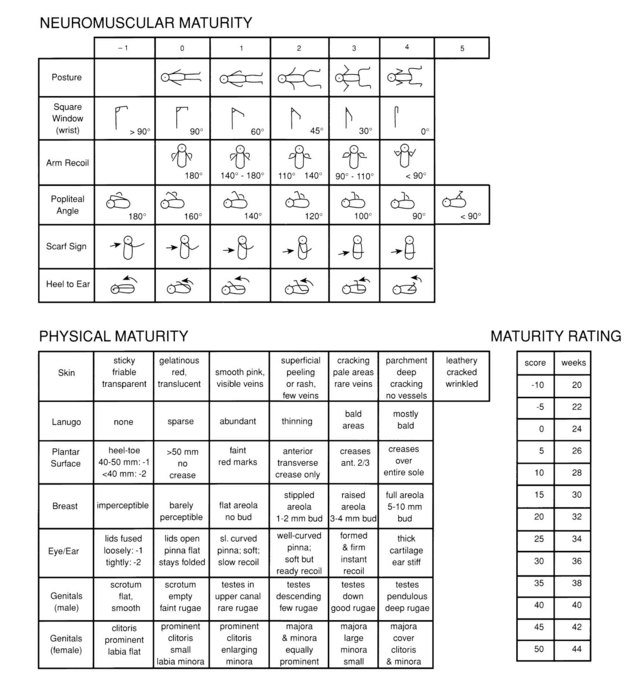
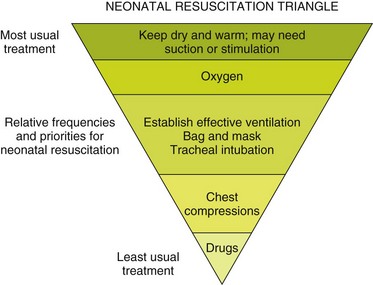
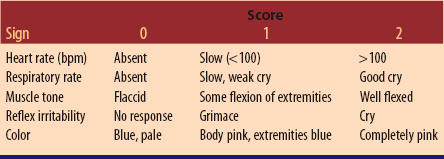
Chapter 27 A Chronic illness in mother’s or father’s family B Previous maternal and paternal illnesses C Ages and present health status of parents D History of previous pregnancies 1. Supervision during pregnancy a. Medications; antibiotics if positive for group beta streptococcus (GBS) b. Illnesses; infections, including sexually transmitted infections c. Ingestion of alcohol, drug use, smoking 5. Type of birth; significant events during initial minutes after birth 6. Newborn responses to birth (Apgar score at 1 and 5 minutes following birth) A Concepts basic to parent-infant relationships 1. Early, frequent parent-infant contact essential for attachment (bonding) a. Biologic changes at puberty and during pregnancy influence development of nurturance b. Interaction between mother and infant begins from moment of conception; can be shared with father c. Childbearing; parenting abilities can be fostered and developed d. Childrearing: parental behavior is learned; frequent parent-infant contact enhances parenting abilities; ambivalence is natural phenomenon as are feelings of resentment 3. Development of parent-infant love 1. Physiologic: food, clothing, hygiene, and protection from environment 2. Emotional: security, comfort, fondling, caressing, rocking, verbalizing, consistent contact with caregiver 1. Biologic inborn desire to reproduce 2. Role concepts that begin with own childhood experiences 3. Primitive emotional relationships D Parent-infant relationships influences b. Health status before pregnancy c. Determinants: age, cultural backgrounds, number in family unit, financial status 3. Characteristics of labor and birth 4. Factors that impede attachment E Reva Rubin Significant Phases of Maternal Adjustment 1. Taking-in phase: mother’s needs must be met before she can meet infant’s needs; talks about self rather than infant; may not touch infant; cries easily; integrates birth experience into reality 2. Taking-hold phase: mother starts to assume responsibility for her infant; lasts from day 2 to day 10; concerned about infant, interested in learning; teachable, reachable, and referable at this time 3. Letting-go phase: mother discards idealized notion of childbirth; may have periods of guilt or grief over childbirth experience F Supportive care to promote attachment 1. Allow time to inspect and identify with infant; encourage parents to touch, fondle, and hold infant 2. Encourage interaction between parents and infant 3. Teach about characteristics of newborn; demonstrate infant care to help parents learn how to meet infant’s and their own needs 4. Evaluate parents’ and infant’s responses; revise plan as necessary; identify disturbed relationships 5. Provide therapeutic environment for various family lifestyle types: nuclear, single parent, gay, blended A Immediate care at time of birth 1. Aspirate mucus to provide an open airway 2. Evaluate with Apgar score 1 and 5 minutes following birth a. Score determined by points for heart rate (most critical), respiration, muscle tone, reflex irritability, and color (Table 27-1: Apgar Score) Table 27-1 (From Lowdermilk DL, Perry SE: Maternity and women’s health care, ed 10, St. Louis, 2012, Mosby.) b. Scores: 7 to 10, good condition; 3 to 6, moderately depressed; 0 to 2, severely depressed; lower scores related to high neonatal morbidity and mortality with need for resuscitative interventions 3. Dry infant and place in skin-to-skin contact with mother or under radiant warmer to maintain body temperature 5. Promote interaction between parents and newborn 6. Identify by applying matching identification bands to infant and mother; may include father and significant others 7. Provide prophylactic eye care; instill prescribed antibiotic (e.g., erythromycin) in each eye to prevent ophthalmia neonatorum caused by gonorrhea or chlamydia infection 8. Administer vitamin K (intramuscularly (IM) in United States, orally in Canada) to prevent hemorrhage 9. Obtain heel-stick blood specimen for laboratory tests to assess adaptation to extrauterine life and presence of congenital conditions; use outer aspect of heel to prevent lancet penetration of bone (Figure 27-1: Heel-stick sites) B Behavioral characteristics during transition period 1. First stage (period of reactivity) d. Heart rate: 160 to 180 beats/min for 15 minutes; declines to baseline of 100 to 120 beats/min e. Respirations: 40 to 60 breaths/min; abdominal; irregular; grunting, flaring of nostrils; intermittent chest retractions 2. Second stage (period of decreased responsiveness) a. Lasts 30 minutes to 2 hours c. Heart rate between 100 and 120 beats/min d. Respirations: rapid, shallow, synchronous; chest shape gradually changes to increase anterior-posterior diameter 3. Third stage (second period of reactivity) C Characteristics and changes during first week of life a. Changes in fetal circulation after umbilical cord is clamped (2) Ductus arteriosus closes; becomes ligamentum arteriosum (3) Umbilical arteries obliterate (4) Circulation becomes similar to adult within 1 hour after birth b. Heart rate regular; 100 to 160 beats/min; variable depending on infant’s activity; soft heart murmur common for first month of life c. Clotting mechanism inadequate because intestinal bacteria necessary for synthesis of prothrombin are lacking; exogenous vitamin K needed d. Liver large but immature; cannot destroy large number of red blood cells (RBCs) that consist of fetal hemoglobin, resulting in physiologic jaundice by third day e. Hemoglobin 14 to 20 g/100 mL; fetal hemoglobin replaced by adult form in 6 weeks 2. Respiratory: 40 to 60 breaths/min during first 2 hours after birth, then 30 to 50 breaths/min; irregular rate; abdominal excursions 3. Temperature: maintained at 97.8° F to 98° F (36.6° C to 36.7° C); environment may cause fluctuations (1) Meconium: first 2 days; black-green; tenacious, (2) Transitional: by third day; mixes with milk stool; green-yellow a. Lanugo: fine, downy hair growth over entire body; preterm infants have more lanugo b. Vernix caseosa; whitish cheesy substance covers body; more abundant in creases; more in preterm infant and less in postterm infant c. Milia: small, whitish, pinpoint spots over nose caused by retained sebaceous secretions that resolve within a month d. Mongolian spots: blue-black discolorations on back, buttocks, and sacral region that disappear by first year; common on dark-skinned infants e. Telangiectatic nevi (stork bites): pink or red areas caused by capillary dilation a. Fetus stores nutrients toward end of third trimester; needs little nourishment during first few days b. Rooting and sucking reflexes active at birth c. Simple carbohydrates, fats, and proteins readily digested d. Inadequately developed cardiac sphincter; regurgitation after feeding e. Swallowing of air when suckling requires being burped during and after feedings a. Attempts to maintain body temperature by flexion of extremities, breaking down of brown fat, and vasoconstriction b. Loses 5% to 10% of body weight by first week of life c. Needs screening for inborn errors of metabolism (1) Phenylketonuria (PKU) testing done 24 to 48 hours after first feeding; test may be done earlier with repeat test at first follow-up visit; infants with excess phenylalanine require special low phenylalanine diet to prevent mental retardation (2) Thyroxine (T4) screening; inadequate thyroxine without replacement therapy leads to cretinism (1) Caused by inadequate glycogen reserve (2) Clinical findings: jitteriness, temperature and respiratory instability (3) Risk factors: small for gestational age (SGA), large for gestational age (LGA), infants of diabetic mothers (IDM), birth trauma, congenital anomalies, endocrine disorders (e.g., hyperinsulism, hypopituitarism, hypothyroidism) a. Related to hormones transmitted by mother b. Males: breast enlargement (gynecomastia); edematous scrotum c. Females: breast enlargement; secretion from nipples (witch’s milk); edematous labia; blood-tinged vaginal discharge (pseudomenstruation) a. Immature central nervous system (CNS) and brain; most responses are reflexive b. Early neural activities: breathing, sucking, crying; necessary for survival 11. Habituation: psychologic or physiologic phenomenon whereby neonate’s response to a repetitive stimulus decreases; promotes environmental selectivity and learning 1. Infant feeding: put to breast or given formula soon after birth; simple proteins, carbohydrates, fats, vitamins, and minerals needed for continued cell growth a. Fluid: 130 to 200 mL/kg or 2 to 3 oz/lb of body weight b. Calories: 110 to 130 calories/kg or 50 to 60 calories/lb of body weight c. Protein: 2.0 to 2.2 g/kg of body weight from birth to 6 months of age; 1.8 g/kg of body weight from 6 to 12 months of age a. Varying degrees of maturity, nutrition needs, and body rhythms b. Schedule modified to meet needs of infant and parents c. Formula-fed infants fed on demand or about every 4 hours d. Breastfed infants fed on demand, approximately every 2 to 3 hours e. Feeding behavior and degree of satisfaction influence psychologic development f. Close mother/father-infant relationship during feeding process meets basic need of trust (Erikson’s stage of trust versus mistrust) 1. Passive immunity in utero: immunoglobulin G (IgG) passes from mother to fetus through placenta 2. Active immunity in utero: fetus produces immunoglobulin M (IgM) by end of first trimester 3. Passive immunity after birth: immunoglobulin A (IgA) passes from mother to infant through colostrum, the precursor to breast milk a. Preterm: birth at less than 37 completed weeks’ gestation b. Term: birth between the 37th and 42nd week of gestation c. Postterm (postmature): birth after 42 weeks’ gestation; subjected to effects of progressive placental insufficiency and diminished amniotic fluid d. Gestational age assessment: new Ballard scale determines gestational age of very low birth weight infants as well as at term. (Figure 27-2: Neuromuscular maturity and physical maturity) a. Appropriate for gestational age (AGA): between 10th and 90th percentile (between 6 and 8.5 lb) b. Large for gestational age (LGA): above 90th percentile c. Small for gestational age (SGA): below 10th percentile d. Low birth weight (LBW): less than 2500 g (6 lb) e. Very low birth weight (VLBW): less than 1500 g (3.5 lb) f. Extremely low birth weight: less than 1000 g (2.2 lb) g. Intrauterine growth restriction (IUGR): fetal growth rate below expected range for gestational age a. Body: pink with cyanosis of hands and feet (acrocyanosis); jaundice during first 24 hours is sign of pathology b. Markings: abrasions, rashes, crackling, birthmarks, forceps marks, ecchymosis, papules 4. Vital signs: moves from least to most invasive a. Respirations, heart rate, temperature b. Respirations: abdominal and irregular; 40 to 60 breaths/min during first 2 hours; then 30 to 50 breaths/min retractions with sternal depression indicate pathology c. Heart rate: 100 beats/min at rest, 180 beats/min when crying; more than 160 beats/min at rest indicates cardiac disorder a. Head and chest circumference: nearly equal with chest slightly smaller than head; if reversed, indicates microcephaly; if head is more than 1 inch (2 to 3 cm) larger than chest it indicates hydrocephaly b. Fontanels: flat; bulging when crying; bulging at rest indicates increased intracranial pressure; sunken indicate dehydration c. Symmetry of face: sides of face should move equally when crying d. Characteristics of head: molding, abrasions, or skin breakdown; caput succedaneum (edema of soft tissue of scalp); cephalohematoma (edema of scalp caused by effusion of blood between skull bone and periosteum) e. Neck: adequacy of range of motion indicated by full head movement in all directions when extended; head lags as infant is raised f. Eyes: discharge or irritation, pupils for reaction to light, equality of eye movements (usually some ocular incoordination), sclerae for clarity, jaundice, or hemorrhage g. Nose: patency of both nostrils; frequent sneezing in an attempt to clear mucus from nose h. Mouth: color and continuity of gums and hard and soft palates; white patches that bleed on rubbing indicate thrush, a monilial infection i. Ears: auricles open; vernix covers tympanic membrane, response when bell is rung close to ear; both eyes at same level as ears (ears lower than eyes indicate congenital anomaly); upper earlobes curved (flatness indicates kidney anomaly) a. Chest auscultation: respiratory sounds audible (noisy crackling sounds are unexpected); regular heart rate b. Breasts and nipples: edematous; witch’s milk is response to maternal hormone stimulation (2) Spleen: tip should be palpable by fingertips under left costal margin (3) Liver: palpation on right side; 1 cm below costal margin (4) Umbilical cord: redness, odor, or discharge; contains one vein and two arteries (two vessels or 2 veins and 1 artery indicate congenital anomalies) (5) Umbilical hernia when crying (6) Femoral pulses: gentle palpation at inner aspect of groin; pulses indicate intact circulation to extremities (1) Testes in scrotum: palpable; one or both may be undescended in preterm infants and some full-term newborns; usually descend during childhood; must descend by puberty or sperm are destroyed by high temperature in abdominal cavity (2) Scrotum: edematous; enlargement indicates hydrocele and diagnosis confirmed by transparent appearance of scrotum when flashlight is held close to scrotal sac (transillumination) (3) Penis: urinary meatus at tip; meatus on upper surface of penis (epispadias); meatus on lower surface (hypospadias) (1) External: labia, urinary meatus, and vaginal opening (3) Vagina: bloody mucoid discharge response to maternal hormones c. Ambiguous genitalia: unclear identification of gender; studies needed to determine gender (e.g., genetic, surgical procedure) a. Hands and arms: thumbs clenched in fist; wrist angle is 0 degrees at term (1) Fingers: number and variation (2) Movement of clavicles and scapulae while putting arms through range of motion: clicking or resistance indicates dislocation or fracture (1) Toes: appearance and number (2) Adduction and abduction of feet during range of motion: resistance or tightness indicate need for further assessment (3) Flexion of both legs onto lower abdomen with abduction of knees: click (Ortolani sign) indicates developmental dysplasia of hip (DDH) (4) Feet placed on flat surface with bent knees: knees of unequal height (Allis sign) indicates DDH 9. Back: dimples, separations, or swellings along spinal column indicates spina bifida 10. Anus: patency confirmed with passage of meconium; imperforate anus ruled out by digital examination 11. Neuromuscular development: reflexes a. Rooting: when cheek is touched with finger, head turns to search for finger; may persist for up to 1 year b. Sucking: object close to mouth elicits sucking movements; persists throughout infancy c. Gag: stimulation of posterior pharynx causes choking; helps prevent aspiration; persists through life d. Grasp: pressure on palm (palmar) or on sole of foot below toes (plantar) elicits flexion; palmar lessens by 3 months, plantar by 8 months e. Babinski: when outer undersurface of foot is stroked in an arc toward inner undersurface, toes separate and flare out; disappears after 1 year f. Moro (startle): sudden jar, noise, or change in equilibrium causes extension and abduction of extremities, followed by flexion and adduction into embrace position; may cry out; disappears by 3 to 4 months g. Crawl: when in prone position on firm surface, crawling movements are elicited; disappears at about 6 weeks h. Step or dance: when supported under both arms with feet on firm surface, stepping movements are elicited; disappears after 3 to 4 weeks i. Tonic neck (fencing): when in supine position, arm and/or leg on side to which head is turned extends with flexion of contralateral limbs; usually disappears by 3 to 4 months
Nursing Care of the Newborn
Foundations of Nursing Care for Newborns
Family and Prenatal History
Parent-Infant Relationships
Adaptation to Extrauterine Life
Nursing Care Common to All Newborns
Assessment/Analysis

Nursing Care of the Newborn
Get Clinical Tree app for offline access