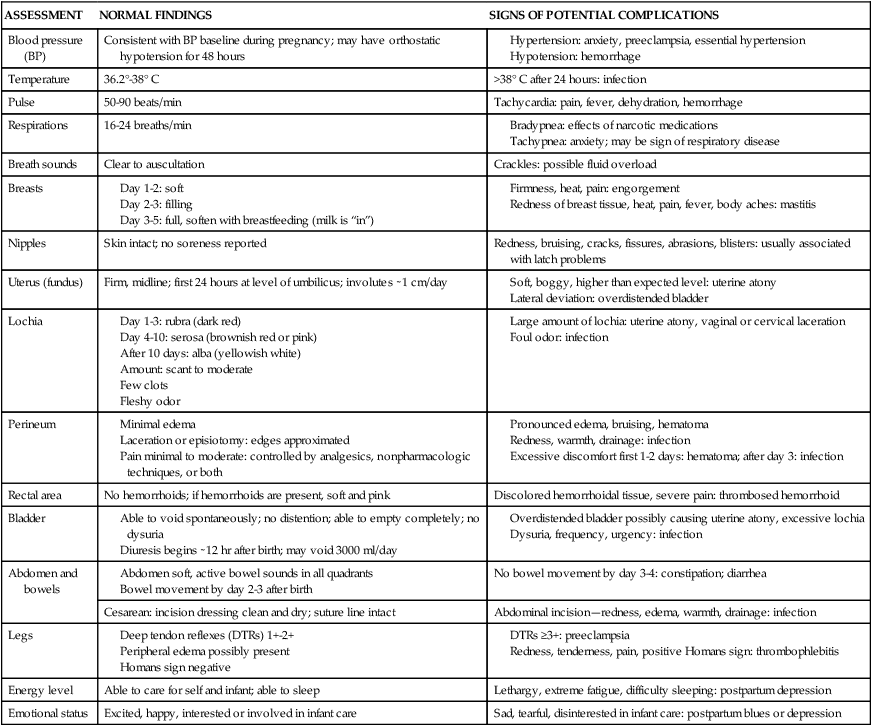
• Describe components of a systematic postpartum assessment. • Recognize signs of potential complications in the postpartum woman. • Identify common selection criteria for safe early postpartum discharge. • Discuss nursing management of women in the postpartum period. • Explain the influence of cultural beliefs and practices on postpartum care. • Discuss postpartum teaching for self-management. • Describe the nurse’s role in these postpartum follow-up strategies: home visits, telephone follow-up, warm lines and help lines, support groups, and referrals to community resources. Additional related content can be found on the companion website at http://evolve.elsevier.com/Lowdermilk/Maternity/ • Case Study: Fourth Trimester • Critical Thinking Exercise: Priority Nursing Care: Postpartum Unit • Nursing Care Plan: Postpartum Care: Vaginal Birth • Spanish Guidelines: Assessing for Hemorrhage • Spanish Guidelines: Assessing for Infection • Spanish Guidelines: Discharge Teaching The approach to the care of women after birth is wellness oriented. Most women in the United States remain hospitalized no more than 1 or 2 days after vaginal birth and some for as few as 6 hours. Because so much important information needs to be shared with these women in a very short time, their care must be thoughtfully planned and provided. Care during the first 1 to 2 hours after birth, also known as the fourth stage of labor, is covered in Chapter 12. This chapter discusses nursing care of the postpartum woman and her family subsequent to the initial recovery period after birth, extending into the fourth trimester—the first 3 months after birth. Women who give birth in birthing centers may be discharged within a few hours, after the woman’s and the infant’s conditions are stable. Mothers and newborns who are at low risk for complications may be discharged from the hospital within 24 to 36 hours after vaginal birth, often called early postpartum discharge, shortened hospital stay, or 1-day maternity stay. The trend of shortened hospital stays is based largely on efforts to reduce health care costs coupled with consumer demands to have fewer medical interventions and more family-focused experiences. Although some advantages to early postpartum discharge can be found, disadvantages also exist (Box 14-1). The trend toward early postpartum discharge in the early 1990s raised serious concerns among health care providers because some medical problems do not show up in the first 24 hours after birth. The greatest risk associated with early discharge is for the infant who may develop jaundice, feeding difficulties, infection, gastrointestinal obstruction, or unrecognized respiratory or cardiac problems. In addition, new mothers have not had sufficient time to learn how to care for their newborns, and breastfeeding may not be well established (AAP Committee on Fetus and Newborn, 2010). The concern for the potential increase in adverse maternal-infant outcomes from early discharge practices led the American College of Obstetricians and Gynecologists (ACOG), the American Academy of Pediatrics (AAP), and other professional health care organizations to promote the enactment of federal and state maternity length-of-stay bills to ensure adequate care for both the mother and the newborn. The passage of the Newborns’ and Mothers’ Health Protection Act of 1996 provided minimal federal standards for health plan coverage for mothers and their newborns. Under this act, all health plans are required to allow the new mother and newborn to remain in the hospital for a minimum of 48 hours after a normal vaginal birth and for 96 hours after a cesarean birth unless the attending provider, in consultation with the mother, decides on early discharge (AAP Committee on Fetus and Newborn, 2010). The American Academy of Pediatrics (2010) recommends that the hospital stay for a mother with a healthy term newborn should be of sufficient length to identify early problems and determine that the mother and family are prepared and able to care for the newborn at home. The health of the mother and newborn should be stable. There should be adequate support systems in place and access to follow-up care (AAP Committee on Fetus and Newborn, 2010). Ideally, hospital stays are long enough to identify problems and to ensure that the woman is sufficiently recovered and is prepared to care for herself and the baby at home. Nurses must consider the medical needs of the woman and her baby and provide care that is coordinated to meet those needs so as to provide timely physiologic interventions and treatment to prevent morbidity and hospital readmission. With predetermined criteria for identifying low risk mothers and newborns (Box 14-2) the length of hospitalization can be based on the medical need for care in an acute care setting or in consideration of the ongoing care needed in the home environment. Early follow-up visits are key to reduce readmissions of newborns. Hospital-based maternity nurses continue to play invaluable roles as caregivers, teachers, and patient and family advocates in developing and implementing effective home care strategies. Postpartum order sets and maternal-newborn teaching checklists (Box 14-3) can be used to accomplish patient care tasks and educational outcomes. With coordination, clinical care and education can be planned and provided throughout pregnancy, during the hospital stay, and in the home after discharge to ensure the family’s continued well-being. Ongoing assessments are performed throughout hospitalization. In addition to vital signs, physical assessment of the postpartum woman focuses on evaluation of breasts, uterine fundus, lochia, perineum, bladder and bowel function, and legs (Table 14-1). TABLE 14-1 Postpartum Assessment and Signs of Potential Complications Once the nursing diagnoses are formulated the nurse plans with the woman what nursing measures are appropriate and which are to be given priority. The nursing plan of care includes periodic assessments to detect deviations from normal physical changes, measures to relieve discomfort or pain, safety measures to prevent injury or infection, and teaching and counseling measures designed to promote the woman’s feelings of competence in self-management and infant care. The spouse or partner and other family members who are present may be included in the teaching. The nurse evaluates continuously and is ready to change the plan if indicated. Almost all hospitals use standardized care plans or care paths as a basis for planning. Nurses individualize care of the postpartum woman and neonate according to their specific needs (see Nursing Care Plan box). Signs of potential problems that may be identified during the assessment process are listed in Table 14-1. Perineal lacerations and episiotomies increase the risk of infection as a result of interruption in skin integrity. Proper perineal care helps to prevent infection in the genitourinary area and aids the healing process. Educating the woman to wipe from front to back (urethra to anus) after voiding or defecating is a simple first step. In many hospitals, a squeeze bottle filled with warm water or an antiseptic solution is used after each voiding to cleanse the perineal area. The woman should change her perineal pad from front to back each time she voids or defecates and should wash her hands thoroughly before and after doing so (Box 14-4).
Nursing Care of the Family during the Fourth Trimester
Web Resources
![]()
Planning for Discharge

Laws Relating to Discharge
Criteria for Discharge
Care Management—Physiologic Needs

ASSESSMENT
NORMAL FINDINGS
SIGNS OF POTENTIAL COMPLICATIONS
Blood pressure (BP)
Consistent with BP baseline during pregnancy; may have orthostatic hypotension for 48 hours
Temperature
36.2°-38° C
>38° C after 24 hours: infection
Pulse
50-90 beats/min
Tachycardia: pain, fever, dehydration, hemorrhage
Respirations
16-24 breaths/min
Breath sounds
Clear to auscultation
Crackles: possible fluid overload
Breasts
Nipples
Skin intact; no soreness reported
Redness, bruising, cracks, fissures, abrasions, blisters: usually associated with latch problems
Uterus (fundus)
Firm, midline; first 24 hours at level of umbilicus; involutes ∼1 cm/day
Lochia
Perineum
Rectal area
No hemorrhoids; if hemorrhoids are present, soft and pink
Discolored hemorrhoidal tissue, severe pain: thrombosed hemorrhoid
Bladder
Abdomen and bowels
No bowel movement by day 3-4: constipation; diarrhea
Cesarean: incision dressing clean and dry; suture line intact
Abdominal incision—redness, edema, warmth, drainage: infection
Legs
Energy level
Able to care for self and infant; able to sleep
Lethargy, extreme fatigue, difficulty sleeping: postpartum depression
Emotional status
Excited, happy, interested or involved in infant care
Sad, tearful, disinterested in infant care: postpartum blues or depression
Plan of Care and Interventions
Prevention of infection

Nursing Care of the Family during the Fourth Trimester
Get Clinical Tree app for offline access



