CHAPTER 3 Definition: Actual or risk for an ineffective breathing pattern NDx or inspiration/expiration that does not provide adequate ventilation. Actual or risk for impaired gas exchange NDx or a deficiency in oxygenation and/or excess in carbon dioxide elimination at the alveolar-capillary membrane level. • Unfamiliar environment and separation from significant others • Anticipated loss of control associated with effects of anesthesia • Lack of understanding of diagnostic tests and planned surgical procedure • Financial concerns associated with the surgery and recovery period • Potential embarrassment or loss of dignity associated with body exposure • Risk of disease if blood transfusions are necessary • Changes in appearance, body functioning, and usual lifestyle and roles DESIRED OUTCOMES: The client will obtain optimal amounts of sleep as evidenced by statements of feeling well rested. DESIRED OUTCOMES: The client will demonstrate beginning progression through the grieving process as evidenced by: Definition: Absence of cognitive information related to a specific topic 2. Tolerate expected level of activity. 3. Have surgical pain controlled. 4. Have clear, audible breath sounds throughout lungs. 5. Have evidence of normal wound healing. 6. Have no signs and symptoms of infection or postoperative complications. 7. Identify ways to prevent postoperative infection. 8. Demonstrate ability to perform wound care. 9. State signs and symptoms to report to health care provider. 10. Share thoughts and feelings about the surgery, diagnosis, prognosis, and treatment plan. 11. Verbalize an understanding of, and a plan for, adhering to recommended follow-up care including future appointments with health care provider, dietary modifications, activity level, treatments, and medications prescribed.
Nursing Care of the Client Having Surgery
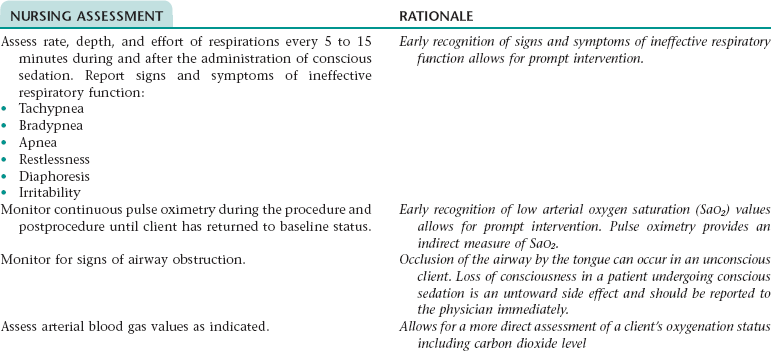
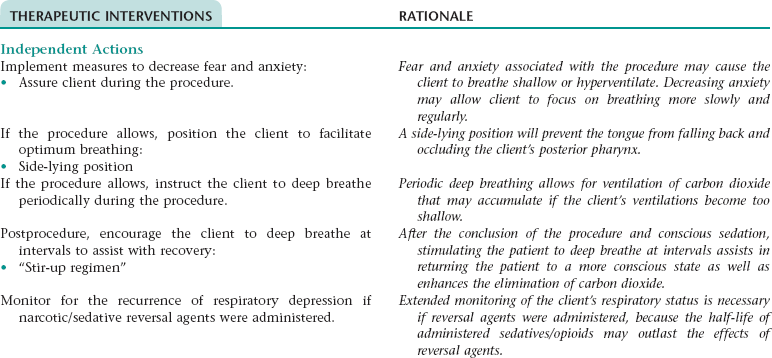
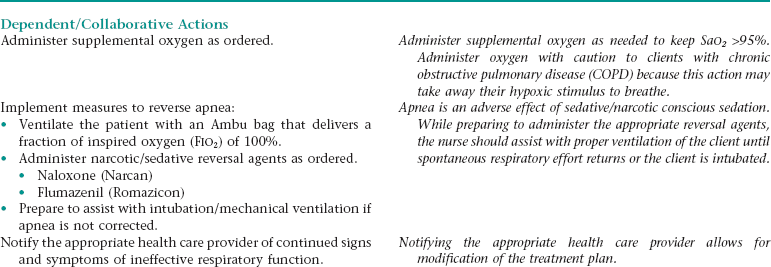
 Nursing Diagnosis ACTUAL/RISK FOR IMPAIRED RESPIRATORY FUNCTION*
Nursing Diagnosis ACTUAL/RISK FOR IMPAIRED RESPIRATORY FUNCTION*
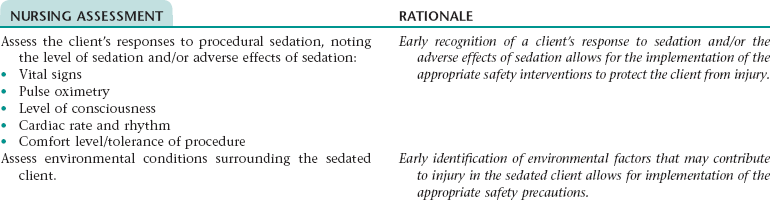
Nursing Diagnosis RISK FOR INJURY NDx
Nursing Diagnosis ACUTE PAIN NDx
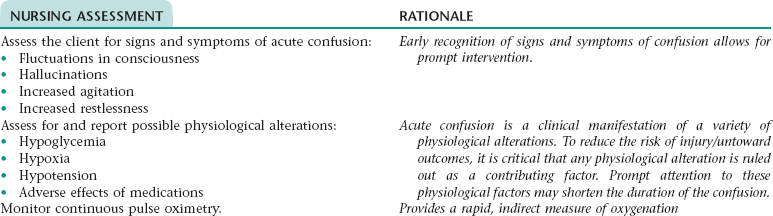
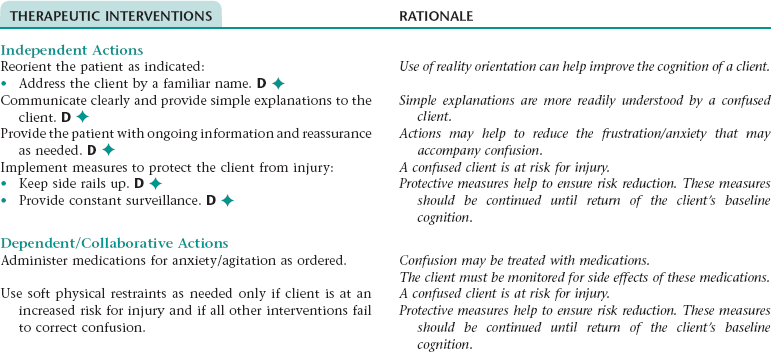
Nursing Diagnosis ACUTE CONFUSION NDx
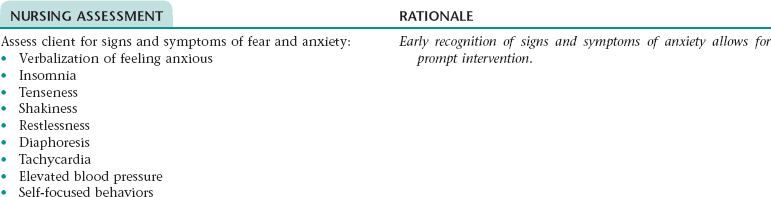
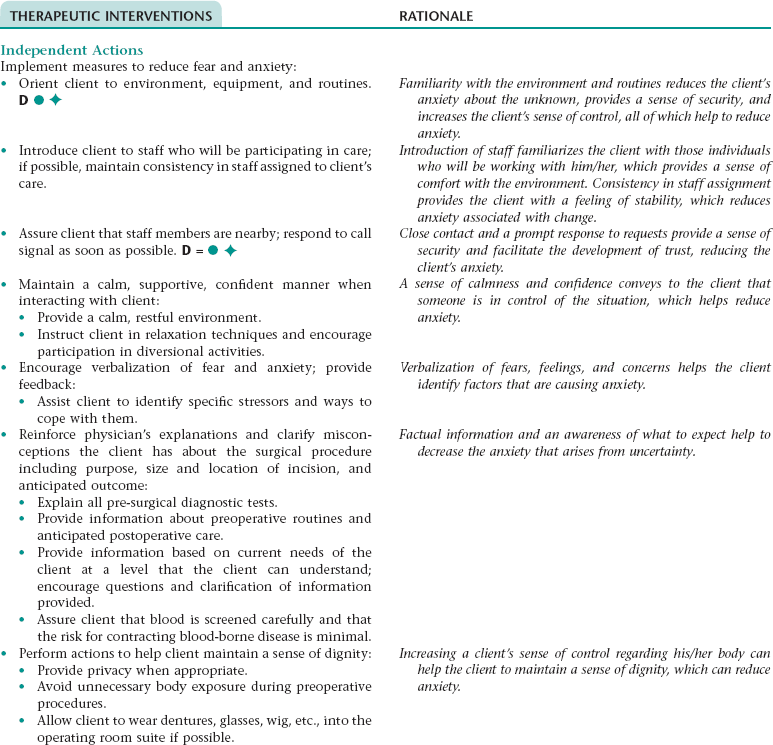
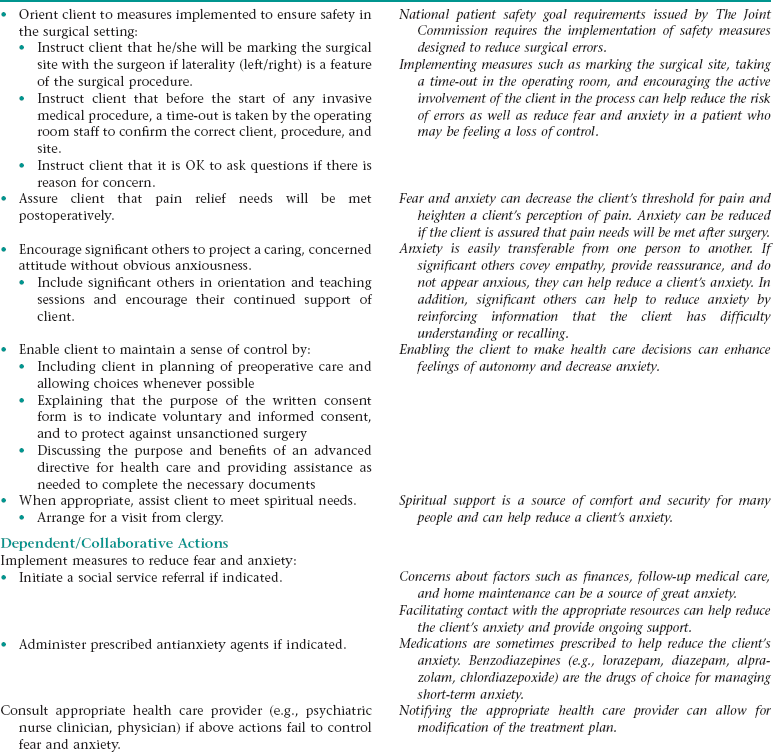
Nursing Diagnosis FEAR NDx/ANXIETY NDx
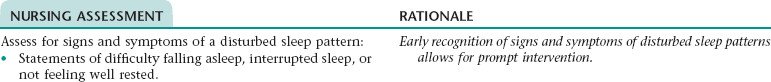
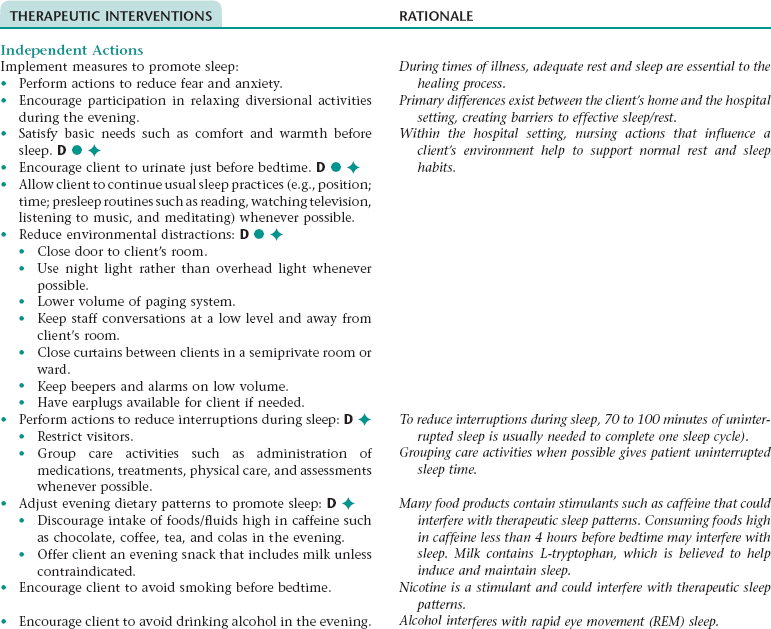
Nursing Diagnosis DISTURBED SLEEP PATTERN NDx
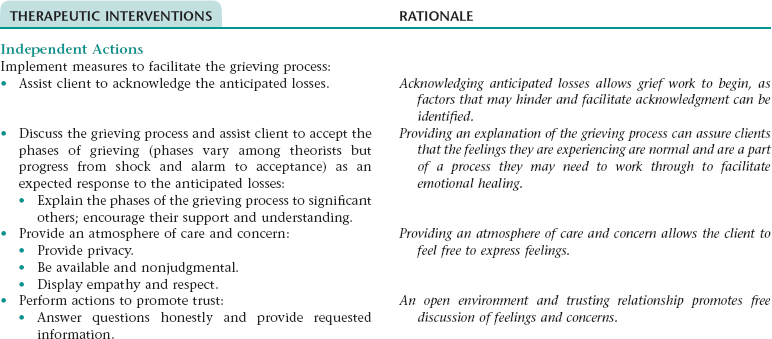
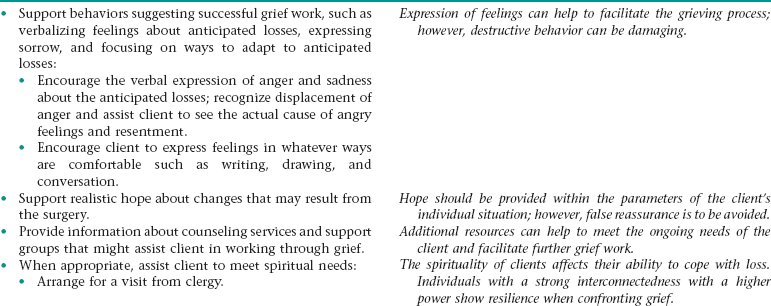
Nursing Diagnosis GRIEVING NDx
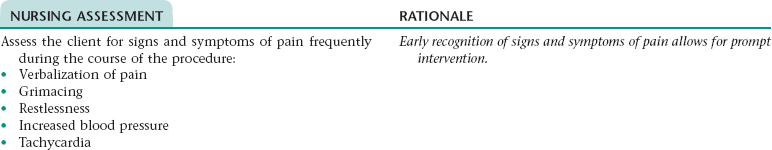
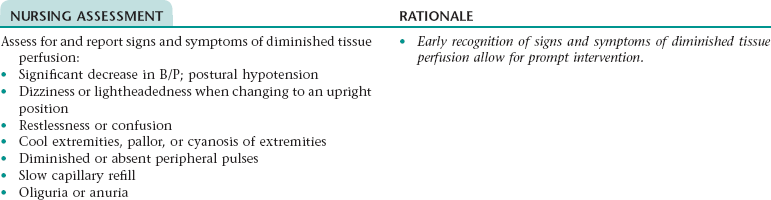
NURSING ASSESSMENT
RATIONALE
Assess for signs and symptoms of anticipatory grieving such as expression of distress about the losses or changes that may occur as a result of the surgery, change in eating habits, inability to concentrate, insomnia, anger, sadness, withdrawal from significant others.
Early identification of signs and symptoms of grieving allows for the implementation of the appropriate interventions.
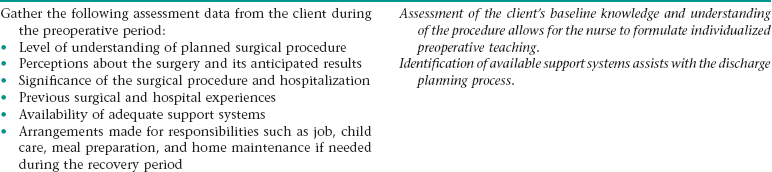
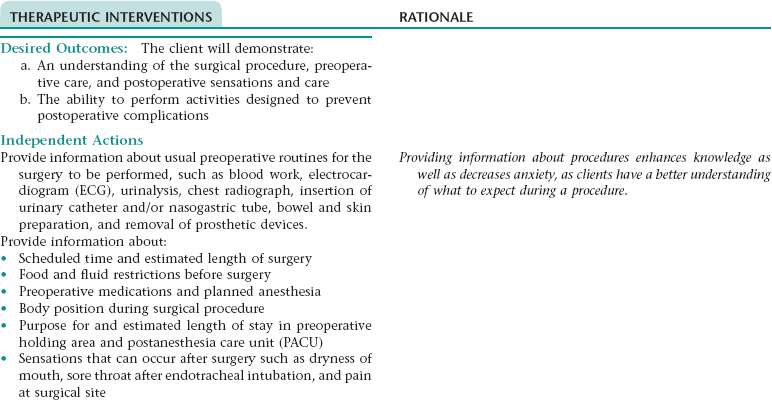
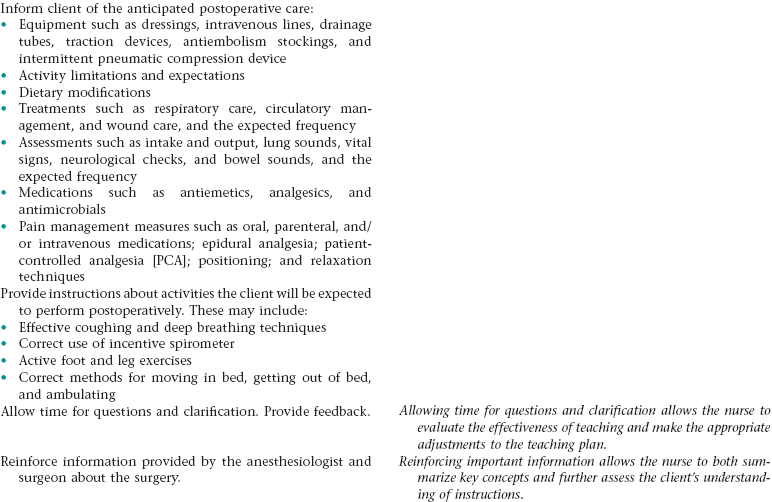
Nursing Diagnosis DEFICIENT KNOWLEDGE NDx
NURSING ASSESSMENT
RATIONALE
Assess the client’s baseline understanding of the surgical procedure, preoperative care, and postoperative sensations and care.
Identifying the client’s baseline knowledge level will allow for the development of the appropriate teaching plan.
Assess the client’s baseline literacy level.
A client’s health literacy level should be assessed before providing instruction so the appropriate teaching plan can be developed. Unless the nurse considers the client’s intellectual abilities when developing the teaching plan, teaching will be unsuccessful.
OUTCOME/DISCHARGE CRITERIA
Nursing Care of the Client Having Surgery
Get Clinical Tree app for offline access