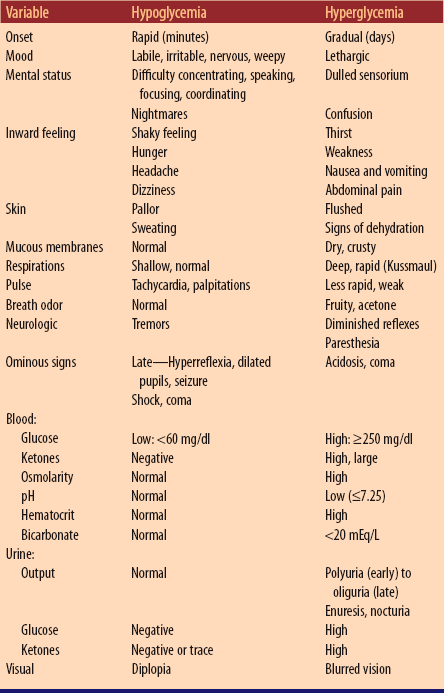
Chapter 33 1. Lanky appearance up to 10 to 12 years: bone development precedes muscular development a. At 6 years: grows 2 inches; gains 2 to 3 kg ( b. At 7 years: grows 2 inches; gains 2.5 kg ( c. At 8 to 9 years: grows 2 inches; gains 3 kg ( 2. Permanent dentition completed: begins with 6-year molars and central incisors at 7 or 8 years of age 1. Refinement of coordination, balance, and control 2. Motor development is primary; necessary for competitive activity C Sensory: visual acuity should be 20/20 1. Readiness for learning, especially in perceptual organization 2. Understands rules and reasons for them 3. Solves trial-and-error problem conceptually rather than through action 4. Greater understanding and use of language 5. Concrete operations (Piaget): knows that quantity remains same when appearance differs (conservation) A Varies with age: number of play activities decreases; amount of time spent in one activity increases C Early school years: boys and girls play together, gradually separate into sex-oriented activities based on cultural influences D Suggested play for 6- to 9-year-olds 1. Housekeeping toys that work; doll accessories; paper-doll sets; simple sewing machine; needlework; building toys 2. Simple word, number, and card games 3. Physically active games (e.g., hopscotch, jump rope, tree climbing, bicycle riding) 4. Collections and hobbies (e.g., stamp collecting, building simple models) E Suggested play for 9- to 12-year-olds 1. Handicrafts (e.g., model kits, pottery clay, hobbies, collections) 2. Skilled and intellectual play (e.g., computer games, chess, puzzles, science sets, magic sets) 1. Usually tolerates separation but prefers parents to be near 2. Fears the unknown, especially when dependency or loss of control is expected 3. Fears bodily harm, especially disfigurement a. 6 to 8 years: personifies death as a “bogeyman” b. 9 to 10 years: has realistic concept, may add to other fears 5. Concerned about self-image when reacting to pain; may use avoidance to cope with physical discomfort 6. Wants scientific rationale for treatments and procedures; willing to participate in self-care B Preparation: age appropriate explanations are associated with increased cognitive and verbal abilities A Begin preparing for hospitalization before admission, if possible 1. Provide explanations that are simple, honest, and at level of understanding 2. Add details about procedures, drugs, surgery, and related issues based on cognitive level and personal experiences B Involve child and parents in planning care 1. Use as outlet for fear, anger, hostility, and as temporary escape from reality 2. Provide diversional play activities that support/challenge mental and motor skills as indicated D Encourage to express feelings, emotions, and fears E Expect and accept regression F Check for loose teeth, especially before surgery G Provide for tutoring if absence from school is more than 2 weeks I Assign age-appropriate roommates who do not compromise physical status J Allow dependency, but foster independence as much as possible; be consistent when enforcing rules A Body Mass Index (BMI): measure of weight in relation to height; plotted on National Center for Health Statistics growth charts 1. Multifactorial (e.g., metabolic, hypothalamic, genetic, social, cultural, psychological) 2. Illness related (e.g., hypothyroidism, adrenal hypercorticoidism, hyperinsulinism); less than 5% 3. Central nervous system (CNS) damage (e.g., injury, infection, brain attack) 4. Complication of illness because of immobility (e.g., muscular dystrophy, paraplegia, Down syndrome, spina bifida) a. During infancy: promote and support breastfeeding for 6 months; encourage mother to continue breastfeeding after introduction of solid food until 12 months of age a. Help to modify diet (e.g., five servings of fruits and vegetables each day; calcium-rich, high-fiber foods; low-calorie dairy products) b. Teach to limit consumption of sugar-sweetened beverages, high-calorie snacks c. Encourage to eat family meals together d. Encourage at least 1 hour of physical activity/day, participation in team sports 3. Structured weight management for BMI between 95th and 98th percentiles 4. Refer for comprehensive multidisciplinary intervention; requires frequent visits to health care provider, dietician, exercise and behavioral specialists (See Chapter 9, Nursing Care of Clients with Endocrine System Disorders, Diabetes Mellitus) a. Based on ethnic origin (e.g., type 1 more frequent among Caucasians, less frequent among African-Americans) b. Gene mutation (maturity-onset diabetes of the young) C Classification (see Table 33-1: Characteristics of Type 1 and Type 2 Diabetes Mellitus) Table 33-1 Characteristics of Type 1 and Type 2 Diabetes Mellitus From Hockenberry M, Wilson D: Wong’s essentials of pediatric nursing, ed 8, St. Louis, 2009, Mosby. 1. Type 1: lack of insulin production 2. Type 2: resistance to insulin action; defective glucose-mediated insulin secretion 3. Other types: pancreatic defects (e.g., cystic fibrosis–related) D Differences between children and obese children/adults 3. Three Ps: Polydipsia; Polyphagia; Polyuria 4. Hyperglycemia, ketoacidosis, diabetic coma b. Characteristics (see Table 33-2: Comparison of Hypoglycemia and Hyperglycemia) Table 33-2 Comparison of Hypoglycemia and Hyperglycemia From Hockenberry M, Wilson D: Wong’s essentials of pediatric nursing, ed 8, St. Louis, 2009, Mosby. 5. Hypoglycemia related to insulin therapy b. Characteristics (see Table 33-2: Comparison of Hypoglycemia and Hyperglycemia) 1. Dietary: calories, carbohydrate, fat, protein intake balanced with physical activity and metabolic needs 2. Insulin (see Chapter 9, Nursing Care of Clients with Endocrine System Disorders, Related Pharmacology, Antidiabetic Agents) 3. Exercise: increased physical activity to reduce need for insulin 4. Hyperglycemia: hospitalization with administration of fluids, electrolytes, insulin 5. Hypoglycemia: immediate supply of readily available glucose followed by complex carbohydrate and protein
Nursing Care of School-Age Children
Growth and Development
Developmental Timetable
 to
to  lb) per year
lb) per year
 lb) per year
lb) per year
 lb) per year
lb) per year
Health Promotion of School-Age Children
Play
Hospitalization of School-Age Children
Database
General Nursing Care of School-Age Children
Health Problems Most Common in School-Age Children
Obesity
Data Base
Nursing Care of the Obese Child
Planning/Implementation
Diabetes Mellitus
Data Base
Characteristic
Type 1
Type 2
Age at onset
<20 years
Increasingly occurring in younger children
Type of onset
Abrupt
Gradual
Sex ratio
Affects males slightly more than females
Females outnumber males
Percentage of diabetic population
5% to 8%
85% to 90%
Heredity:
Family history
Sometimes
Frequently
Human leukocyte antigen
Associations
No association
Twin concordance
25% to 50%
90% to 100%
Ethnic distribution
Primarily Caucasians
Increased incidence in Native Americans, Hispanics, African-Americans
Presenting symptoms
3 P’s common: polyuria, polydipsia, polyphagia
May be related to long-term complications
Nutritional status
Underweight
Overweight
Insulin (natural):
Pancreatic content
Usually none
>50% normal
Serum insulin
Low to absent
High or low
Primary resistance
Minimum
Marked
Islet cell antibodies
80% to 85%
<5%
Therapy:
Insulin
Always
20% to 30%
Oral agents
Ineffective
Often effective
Diet only
Ineffective
Often effective
Chronic complications
>80%
Variable
Ketoacidosis
Common
Infrequent
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



 inches; gains 4.5 kg (10 lb) per year
inches; gains 4.5 kg (10 lb) per year