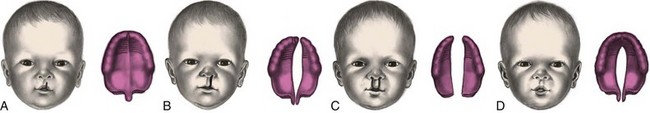
Chapter 30 1. Body: flexed position with pelvis high when prone; asymmetric posture (tonic neck reflex) a. Held parallel with body in prone position b. Turns from side to side when prone; can lift momentarily from flat surface D Socialization and vocalization A Physical: posterior fontanel closed 1. Holds head erect for short time; can raise chest supported on forearms 2. Bears some weight on legs when held in standing position 3. Holds rattle when placed in hand 4. Grasp, tonic neck, and Moro reflexes fading; step or dance reflex disappears D Socialization and vocalization 1. Sits when back is supported; knees flexed and back rounded; balances head 2. Maintains symmetric body position 3. Sustains portion of own weight when held in standing position 4. Reaches for and grasps object with whole hand; misjudges distances 5. Moves own hand or object to mouth at will 6. Rolls over from abdomen to back 7. Lifts head and shoulders at 90-degree angle when prone 8. Early reflexes (e.g., grasp, tonic neck, Moro) have disappeared 1. Recognizes familiar objects and people 2. Eyes move together; developing focus to accommodate different distances D Socialization and vocalization 1. Weight: doubles birth weight by 6 months 2. Height: grows about 1.25 cm ( 3. Head circumference: grows about 0.5 cm (1/5 inch)/month 4. Teething begins with two lower central incisors, followed by upper incisors 1. Turns over from stomach to back and back to stomach 2. Sits unsupported when placed in forward-leaning position 3. Lifts head when supine as if trying to sit up 4. Approaches toy and grasps it with one hand; can transfer toy from hand to hand and from hand to mouth 5. Plays with feet; puts them in mouth a. Landau (6 to 8 months to 12 to 24 months): when suspended in horizontal prone position, head is raised, legs and spine are extended b. Parachute (7 to 9 months, persists indefinitely): when suspended in horizontal prone position and suddenly thrust forward, hands and fingers extend forward as if to protect from falling 1. Has taste preferences; spits out disliked food 2. Develops object permanence: recognizes things are still present even though not seen (e.g., peek-a-boo) D Socialization and vocalization 1. Sits steadily alone; pulls self to standing position; stands holding onto furniture 2. Develops hand-to-mouth coordination 3. Develops pincer grasp, hand preference C Socialization and vocalization 1. Definite social attachment (e.g., stretches arms toward loved ones); stranger anxiety (e.g., turns or pushes away and cries) 2. Responds to own name; begins separating self from caregiver 3. Reacts to adult anger; cries when scolded 4. Develops imitative and repetitive speech; uses vowels and consonants, (e.g., Mama, Dada); comprehends words such as “bye-bye” 1. Weight: birth weight triples 2. Height: birth length increases by 50% 3. Equal head and chest circumference 4. Teeth: upper and lower lateral incisors; total of six to eight 1. Creeps (abdomen supported off floor) 2. Stands alone for short time; walks with help; moves around by holding onto furniture (cruising) 3. Sits down from standing position without help 4. Eats from spoon; drinks from cup with help; prefers using fingers 5. Plays “pat-a-cake” and “peek-a-boo”; holds crayon to mark paper D Socialization and vocalization 1. Exhibits emotions (e.g., jealousy, affection, anger) 2. Enjoys familiar surroundings; explores away from caregiver 3. Fearful in strange situations or with strangers; clings to caregiver 4. May develop attachment to “security” object 5. Can say two meaningful words besides Dada or Mama; understands simple verbal requests, such as “Give it to me” A Narcissistic: revolves around own body B Responses: global, undifferentiated C Dependent; progresses to interdependent, then independent D Directed toward physical, motor, sensory, language, cognitive, and personal-social development F Suggested toys: should be simple because of short attention span (e.g., rattles; soft, stuffed toys; mobiles; push-pull toys; simple musical toys; unbreakable mirrors; weighted or suction toys; squeeze toys; teething toys; books with textures; activity boxes; nested boxes; fitting forms) 1. During first year: should be charted to evaluate proportional gain in length, weight, and head circumference; overweight and underweight indicate malnutrition 1. Optimum nutrition and establishment of appropriate eating habits essential for growth and development 2. Diet should provide nutritional requirements for age and prevent obesity 3. Gastrointestinal disturbances (e.g., vomiting, diarrhea, constipation) interfere with optimum nutrition despite adequate diet 4. Consistency of foods: progress from liquid to semisoft, to soft, to solids as dentition and jaw develop A Birth: full-term infant has sucking, rooting, and swallowing reflexes B Newborn: feels hunger; indicates desire for food by crying; expresses satiety by falling asleep C One month: has strong extrusion reflex D Five to 6 months: uses fingers to eat E Six to 7 months: chews solids F Eight to 9 months: holds spoon; plays with it during feeding H Twelve months: drinks from cup; bottle preferred at times (bedtime) A Breast milk or iron-fortified commercial formula recommended for first year of life; American Academy of Pediatrics states iron-fortified commercial formula is acceptable but not preferred alternative to breastfeeding B Breast milk: most complete diet for first 6 month; may require supplementation 1. Iron supplement: needed by 4 to 6 months 2. Fluoride supplementation: determined by fluoride content of water supply; started between six months and three years; American Academy of Pediatrics and American Dental Association do not recommend fluoride supplementation for first 6 months of life; fluoride supplementation is controversial, but continues to be recommended 3. Vitamin D supplementation: for infants of mothers who are vitamin D deficient or not exposed to adequate sunlight C Whole cow’s milk: should not be introduced until after 1 year of age; difficult to digest; inadequate in iron, vitamin C, and other essential nutrients 1. Infant cereals: first solid food introduced at about 6 months; should be iron-fortified; rice cereal has low allergenic potential; should be continued until 18 months of age 2. Order of introduction varies; vegetables and/or fruits first, then meats; should be strained, puréed, or mashed 3. Finger foods: introduced at 6 to 7 months (e.g., toast, teething cracker, raw fruit) 4. Chopped table food or commercially prepared junior foods: started at 9 to 12 months E Fruit juices: should be offered from cup early to prevent dental caries; can be substituted for milk for one feeding each day F Method for introducing solid foods 1. Feed several sucks of breast milk or formula when hungry, and then offer solid food 2. Introduce one food at a time, usually at intervals of 4 to 7 days, to allow for identification of food allergies 3. Begin spoon feeding by placing food on back of tongue because of tendency to thrust tongue forward (extrusion reflex begins to fade by 3 to 4 months) 4. Use small spoon with straight handle; begin with 1 or 2 teaspoons; gradually increase to several tablespoons per feeding 5. Increase amount of solid food; decrease milk intake to about 900 mL (30 oz) daily; prevent overfeeding 6. Avoid mixing solid foods with formula and bottle feeding the mixture 1. Psychologically significant; requires relinquishing major source of pleasure 2. Readiness: after 6 months; experiences pleasure from spoon feeding (e.g., desire for more freedom, control over body and environment) 3. Gradual replacement of 1 bottle at a time with cup; nighttime bottle last to be relinquished 4. Termination of breastfeeding A Types of immunizations that provide active immunity; see Chapter 3, Integral Aspects of Nursing Care, Infection, Review of Physiology (Immunity), for Figure 3-2 A, B, and C (Recommended Immunization Schedules—United States 2011) 1. Hepatitis B vaccine (Hep B) a. Three doses (at birth to 1 month, 2 months, and between 6 and 18 months); for all adolescents not immunized; for health care providers because of risk of transmission via needle sticks or exposure to blood 2. Hepatitis A vaccine (Hep A) 3. Diphtheria, tetanus, acellular pertussis (DTaP) a. Three doses (at 2, 4, and 6 months); fourth dose between 12 and 18 months; booster dose at 4 to 6 years of age b. Diphtheria toxoid: effective for about 10 years; febrile reaction more common in older children c. Tetanus toxoid: nearly 100% effective; induces immunity for about 10 years; given at 5-year intervals if there is possibility of contaminated wound d. Tetanus and diphtheria (Td) toxoid: for adults; recommended every 10 years after last booster (at about 5 years of age); administered to children older than age 7 years not previously immunized e. Pertussis vaccine: passive immunity not acquired from mother; not given after age 7 years because incidence of disease poses less risk than vaccine’s side effects 4. Inactivated polio vaccine (IPV) a. Three doses (at 2, 4, and 6 to 18 months); fourth dose between 4 and 6 years of age b. Recommended for all children younger than 18 years of age c. Intramuscular route preferred in United States d. Oral polio vaccine (OPV) used for worldwide immunization; rate of polio is now 1 in 2.4 million people e. Administered to infants/children who are asymptomatic HIV-positive or those with immune deficiencies and their siblings 5. Haemophilus influenzae type b vaccine (Hib) a. Four doses (three doses at 2, 4, and 6 months of age; one dose between 12 and 15 months) b. Some formulations do not require a dose at 6 months if doses were received at 2 and 4 months of age a. Four doses (3 doses at 2, 4, and 6 months of age; one dose between 12 and 15 months) b. High-risk children receive additional dose between 2 and 6 years of age 8. Chickenpox (Varicella) vaccine a. First dose at minimum of 12 months of age; second dose between 4 and 6 years of age; second dose before 4 years if at least 3 months have elapsed between the first and second dose b. Two doses at least 28 days apart for children 13 years of age and older who never had chickenpox or received chickenpox vaccine c. Side effects: malaise; pruritic rash that begins on abdomen, progresses to face and proximal extremities 9. Measles (rubeola), mumps, and rubella (German measles) vaccine (MMR); live, attenuated vaccine a. Acquired natural immunity from mother for first 12 to 15 months of age b. First dose at minimum of 12 months of age; second dose between 4 and 6 years of age (can be administered earlier if more than 28 days have elapsed since last dose) c. Rubella vaccine: administered to women not previously immunized during preconception counseling or postpartum; causes a maculopapular rash B Factors influencing administration of immunizations 1. Benefit from being protected by immunization outweighs risk from contracting disease 2. Maternal antibodies acquired in utero from placenta provide passive immunity for first several weeks of life; antibodies acquired from breastfeeding mother after birth provide infant with immunity against most viral, bacterial, and fungal infections during infancy a. Administration of blood transfusion or immune serum globulin that provide passive immunity; MMR and varicella vaccine postponed for 3 months b. High fever, serious illness; common cold not a contraindication c. Impaired immune system or immunosuppressive therapy in child or family member d. Systemic malignancy (e.g., leukemia) e. Neurologic problems (e.g., seizures) f. Allergic reaction to previously administered vaccine or anaphylactic reaction to egg protein A Accidents are a leading cause of death 2. Aspiration of small objects (6 to 12 months) 3. Ingestion of poisonous substances (6 to 12 months) 4. Falls, rolling off elevated surfaces, tumbling down stairs a. Sudden infant death: place on back; avoid soft, moldable bedding (e.g., pillows, quilts) (1) Avoid using plastic bags, plastic covers for mattress (2) Use firm mattress that fits snugly in crib; avoid using pillows, loose blankets (3) Provide sleeping enclosure in which infant sleeps alone (4) Ensure crib and carriage designs meet regulations; use carrying slings cautiously (5) Keep crib and infant seat away from window blinds and cords (6) Offer one-piece pacifiers; avoid tying pacifier to a string, remove bibs after use (2) Never leave on raised, unguarded surface (3) Restrain in infant seat; never leave unattended while seat is on raised surface (4) Avoid using high chair until old enough to sit unsupported (1) Set household hot water heater at temperature lower than 120° F (2) Check temperatures of bathwater and warmed formula in advance (3) Avoid pouring hot liquids nearby when infant is nearby or sitting on lap (4) Keep cigarettes and ashes at a distance; do not allow smoking in home (5) Keep in sun for no more than several minutes; use hats and apply sunscreen (6) Use flame-retardant clothes and wash according to label directions (7) Check surface heat of car restraint; do not leave in car unattended (1) Transport in regulation three- to five-point harness rear-facing infant carrier in back seat of car; anchor via seat belt (2) Secure car seat in back seat of car facing rear until 1 year of age or weighs at least 20 pounds; when older place in convertible seat, strapped in back seat of car f. Environment: keep sharp, jagged-edged objects away from infant’s vicinity (1) Keep buttons, beads, and other small objects out of reach; keep floor free of small objects; inspect toys for removable parts (2) Offer pacifiers with one-piece construction and loop handle (3) Do not feed infant hard candy, nuts, food with pits or seeds, or whole hot dogs; cut foods, such as hot dogs, into small irregularly shaped pieces b. Suffocation: see birth to 4 months c. Falls: restrain in high chair; keep crib rails raised to full height (1) Verify that paint for furniture or toys is lead free (2) Place toxic substances on high shelf and/or in locked cabinet; store toxic substances in original containers; avoid storing large quantities of cleaning fluids, paints, pesticides, and other toxic substances; discard used containers of poisonous substances (3) Place purses/backpacks out of reach (4) Hang plants or place on high surface out of reach (5) Know national toll-free telephone number of Poison Control Center (800-222-1222) e. Burns: see birth to 4 months f. Motor vehicles: see birth to 4 months g. Environment: offer toys that are smooth and rounded, made of wood or plastic; do not allow long, pointed objects as toys a. Aspiration: see 4 to 7 months (1) Keep doors of bathrooms, ovens, dishwashers, refrigerators, clothes washers and dryers closed at all times (2) Remove doors if storing or discarding appliances (e.g., refrigerator, dishwasher) (3) Fence in swimming pools; always supervise when near any source of water (e.g., toilets, filled bathtubs, cleaning buckets) c. Falls: fence stairways at top and bottom if there is access to either end (1) Administer medications as drug, not candy (2) Do not administer adult medications unless prescribed (3) Replace caps to medications and toxic substances immediately after use; use child protector caps (4) Store hazardous materials in locked cabinets or out of reach (e.g., medications, cleaning supplies, paint) (1) Place guards in front of heating appliances, fireplace, or furnace (2) Keep electrical wires hidden or out of reach; do not allow play with electrical appliances (3) Use plastic guards in electrical outlets; place furniture in front of outlets (4) Keep pot handles on stove out of reach A Reactions to parental separation begin in later months (see Chapter 31, Nursing Care of Toddlers, Hospitalization of Toddlers); reactions to procedures begin later (see Chapter 32, Nursing Care of Preschoolers, Hospitalization of Preschoolers) B Pain, although felt, is not localized; requires appropriate analgesia and sedation for painful procedures A Assess physical, physiologic, and behavioral responses (see Chapter 29, Foundations of Child Health Nursing, Age-Related Responses to Pain, Nursing Care Related to Pain Assessment, Table 29-1, [FLACC Scale]) B Meet physical and emotional needs immediately to support development of trust C Provide nonnutritive sucking to meet oral needs D Encourage significant others to stay for comfort and support, especially after 5 months A Fetal/newborn responses to alcohol consumption during pregnancy B Range of lifelong disorders; fetal alcohol syndrome (FAS) most severe form of FASD C Incidence: approximately 0.5 to 2 per 1000 live births 1. Unusual facial features (e.g., smooth ridge between nose and upper lip [hypoplastic philtrum], receding chin [hypoplastic maxilla]) 2. Small head size; lower-than-average height, weight, or both 3. Central nervous system (CNS) problems (e.g., impaired coordination, learning, memory, attention span, communication, vision, or hearing; hyperactivity; difficulties in school and with interpersonal relationships; may include more than one problem) 1. Pharmacologic management depending on clinical findings 2. Reduction of noxious environmental stimuli 3. Encouragement to achieve self-regulation 4. Provision of IV fluids and nutrients until able to maintain feedings 5. Therapy specific to individualized needs; may be similar to needs of preterm infants 2. Observe for signs of withdrawal a. Usually within 6 to 12 hours after birth; persist for about 3 days b. Assess for clinical manifestations related to CNS, GI, respiratory, autonomic nervous system alterations c. Monitor for seizure activity; protect from injury during seizure 3. Maintain protective environment a. Limit environmental stimuli; keep in quiet, dimly lit room c. Touch gently; avoid sudden positional changes a. Use containment devices or swaddle with extremities in flexed position b. Allow hand-to-mouth activity to promote self-soothing c. Provide pacifier for nonnutritive sucking 5. Provide fluid and nutrients a. Allow extra time for feedings b. Offer frequent, small feedings d. Elevate head of mattress after feedings 1. Provide emotional support to parents 2. Assist parents in setting realistic expectations and goals 3. Refer for testing of intellectual functioning (See Chapter 31, Nursing Care of Toddlers, Nursing Care of Children Who Are Cognitively Impaired) 4. Provide specific care for associated congenital malformations 5. Encourage genetic counseling appropriate for type of problem 1. Free trisomy 21: associated with advanced maternal age (older than age 40); can occur in all age groups 2. Translocation 15/21: transmitted most often by mother, who is carrier; not age related 3. Mosaicism: mixture of healthy cells and cells that are trisomic for 21; similar developmental outcome as those with trisomy 21 1. Head: brachycephaly, flat occiput a. Nose: depressed bridge (saddle nose) b. Eyes: inner epicanthic folds; slanted eyes (oblique palpebral fissure); speckling of iris (Brushfield spots) c. Ears: small, usually low set 2. Muscles: hypotonic (e.g., protruding abdomen, umbilical hernia); hyperflexible with lax joints 3. Hands and feet: broad, short, stubby; one transverse palmar crease 4. Sexual development: delayed; incomplete (men usually infertile) 5. Associated problems: cardiac malformation, respiratory difficulty, obesity A Incomplete fusion of embryonic structures surrounding primitive oral cavity (cleft lip) B Failure of primary and secondary palatine plates to fuse (cleft palate) (Figure 30-1: Variations in clefts of lip and palate at birth) 1. Cleft lip: incomplete fusion of maxillary and premaxillary processes; should be completed between 5 and 8 weeks’ gestation; more common in males 2. Cleft palate: incomplete fusion of palatal structures; may involve soft or hard palate; may extend into nose, forming oronasal passageway; fusion completed between 9 and 12 weeks’ gestation; more common in females 1. Evidence of hereditary influence a. Multifactorial inheritance; increased frequency in relatives b. Higher incidence in monozygotic twins than in dizygotic twins D Occurs with other congenital anomalies 1. Bilateral or unilateral; if unilateral, more common on left side 2. Cleft lip: several degrees; complete cleft usually continuous with cleft palate a. Difficult feeding; cannot form vacuum with mouth to suck; may be able to breastfeed (breast may fill cleft, making sucking easier) b. Requires special feeding devices (e.g., Cleft Lip/Cleft Palate Nurser, Medela Haberman feeders, Pigeon bottle) c. Mouth breathing dries mucous membranes, predisposing to infection a. Prone to infection, especially otitis media b. Altered speech; complete palate needed to trap air in mouth c. Malposition of teeth and maxillary arch; extensive orthodontic and prosthodontics needed d. Hearing problems caused by recurrent otitis media (eustachian tube connects nasopharynx and middle ear, transports pathogens to ear) e. Requires special feeding devices similar to those used for cleft lip 1. Surgical repair: may require multiple surgeries throughout childhood a. Cleft lip: repaired in first days after birth; further modification may be necessary; aids ability to suck; helps parents cope by modifying visible aspects of defect b. Cleft palate: surgical intervention and repair as early as neonatal period but not later than between 12 and 18 months; done before speech is fully developed 2. Multidisciplinary team approach: pediatric plastic surgeons, orthodontists, otolaryngologists, speech and language therapists, audiologists, nurses, social workers 3. Cleft palate: temporary or permanent dental prostheses to replace missing teeth; devices applied to mechanically close cleft until ready for surgical closure a. Feed in upright position to prevent aspiration; use adaptive feeding device; encourage breastfeeding b. Feed slowly, burp frequently because of swallowed air c. Perform meticulous oral hygiene to prevent infection d. Teach parents how to perform oral/dental hygiene 2. Postoperative nursing care for cleft lip a. Maintain patent airway because of edema and mouth breathing; keep oral suction equipment available b. Cleanse suture line to prevent crust formation and scarring c. Minimize crying to prevent pressure on suture line; encourage a parent to stay with child d. Use pain rating scale and medicate appropriately e. Place in supine position with arm or elbow restraints; change position to side or sitting up to prevent hypostatic pneumonia; remove restraints when supervised f. Feed (see preoperative care) 3. Postoperative nursing care for cleft palate a. Avoid traumatizing operative site; tell child who can follow directions not to rub tongue on roof of mouth; avoid offering straw, spoon, toothbrush b. Use pain rating scale and medicate appropriately c. Provide liquid or blenderized diet d. Provide emotional support for parents; prolonged recovery 4. See Chapter 29, Foundations of Child Health Nursing, Nursing Care Related to Meeting the Needs of the Family of a Child with Special Needs A Failure of esophagus to develop continuous passage to stomach; failure of trachea and esophagus to develop into separate structures B Risk factors: low birth weight; about 50% associated with other anomalies (e.g., vertebral anomalies, imperforate anus, radial and renal dysplasia, limb anomalies, cardiac malformations) 2. Atresia of esophagus without tracheal fistula 4. Most common: proximal esophageal atresia combined with distal tracheoesophageal fistula 1. Chalasia: incompetent cardiac sphincter 2. Choanal atresia: no opening between one or both nasal passages and nasopharynx 1. Excessive salivation, drooling 2. Choking, sneezing, coughing during feeding, regurgitation of formula through mouth and nose 3. Catheter cannot be passed into stomach (depending on type) F Therapeutic intervention: surgical repair; one procedure or several, depending on health status and severity of defect a. Observe for signs of respiratory distress; suction oropharynx to remove accumulated secretions b. Keep NPO; monitor intake and output; offer pacifier to meet sucking needs c. Change position to prevent pneumonia d. Maintain with head elevated on inclined plane of at least 30 degrees e. Maintain patency of nasogastric tube if used to decompress stomach b. Maintain nasogastric/gastrostomy tube to drainage c. Change position to prevent pneumonia d. Maintain function of chest tubes, if used e. Maintain nutrition by oral, parenteral, or gastrostomy route f. Use pain rating scale and medicate appropriately g. Provide comfort and physical contact; provide a pacifier for nonnutritive sucking until oral feedings are resumed A Thickened circular muscle of pylorus; occurs within first weeks of life 1. Narrow opening between stomach and duodenum 2. Obstruction from inflammation and edema 3. Compensatory dilation, hypertrophy, and hyperperistalsis of stomach 4. May be isolated disorder; may be associated with intestinal malrotation, esophageal and duodenal atresia, anorectal anomalies 1. Palpable olive-shaped mass in right upper quadrant 2. Vomiting: not bile-stained; progressively projectile 3. Dehydration; weight loss; failure to thrive; electrolyte and acid-base imbalances 4. Constipation; distended epigastrium 5. Obstruction within 4 to 6 weeks: visible peristaltic waves across abdomen; colicky pain b. Monitor IV fluid, electrolytes, weight c. Offer prescribed water, glucose, or electrolyte solution for first feeding; progress to half-strength formula/breast milk and then to full-strength formula/breast milk, usually within 24 hours 3. Teach parents specific feeding method A Congenital life-threatening obstruction of intestinal tract 1. Mechanical: constricted or occluded lumen (e.g., incarcerated inguinal hernia progressing to strangulated with interruption of blood supply; intussusception; volvulus) 2. Muscular: interference with regular muscular contractions 1. Abdominal distention, paroxysmal pain 2. Absence of stools, meconium in newborn (meconium ileus) 3. Vomiting of feeding progressing to bile-stained material, may be projectile 4. Weak, thready pulse; cyanosis; weak, grunting respirations from abdominal distention, causing diaphragm to compress lungs
Nursing Care of Infants
Growth and Development
Developmental Timetable
One Month
Two to Three Months
Four to Five Months
Six to Seven Months
 inch)/month
inch)/month
Eight to Nine Months
Ten to Twelve Months
Health Promotion of Infants
Play
Nutrition during Infancy
Nutrition in Relation to Growth and Development
Feeding Milestones
Guidelines for Infant Nutrition
Immunizations
Injury Prevention during Infancy
Hospitalization of Infants
Data Base
General Nursing Care of Infants
Health Problems That Begin in Infancy and May Persist through Childhood (Nursing care includes care of the infant and child)
Fetal Alcohol Spectrum Disorders (FASD)
Data Base
Nursing Care of Alcohol-Exposed Infants
Planning/Implementation
Chromosomal Aberrations
General Nursing Care of Children with Chromosomal Aberrations
Planning/Implementation
Trisomy 21 (Down Syndrome)
Data Base
Gastrointestinal Malformations
Cleft Lip and Cleft Palate
Data Base
Nursing Care of Children with Cleft Lip/Cleft Palate
Planning/Implementation
Nasopharyngeal and Tracheoesophageal Anomalies
Data Base
Nursing Care of Children with Nasopharyngeal and Tracheoesophageal Anomalies
Planning/Implementation
Hypertrophic Pyloric Stenosis (HPS)
Data Base
Nursing Care of Children with Hypertrophic Pyloric Stenosis
Planning/Implementation
Intestinal Obstruction
Data Base
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



 inch)/month
inch)/month