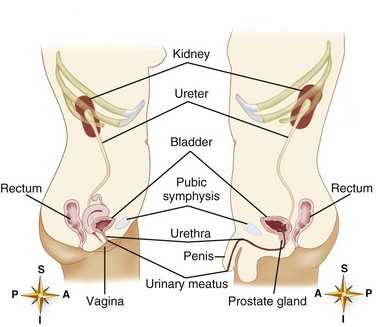
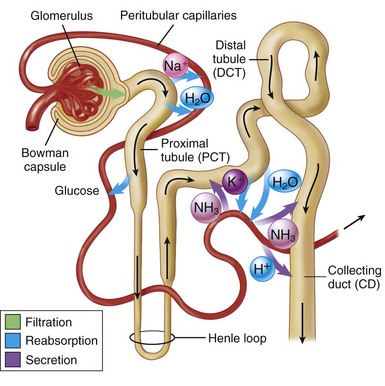
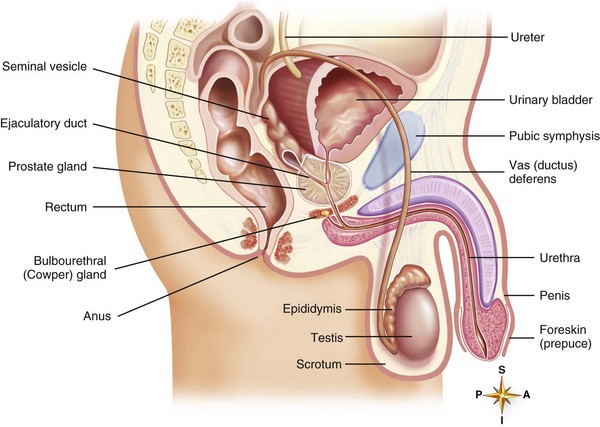
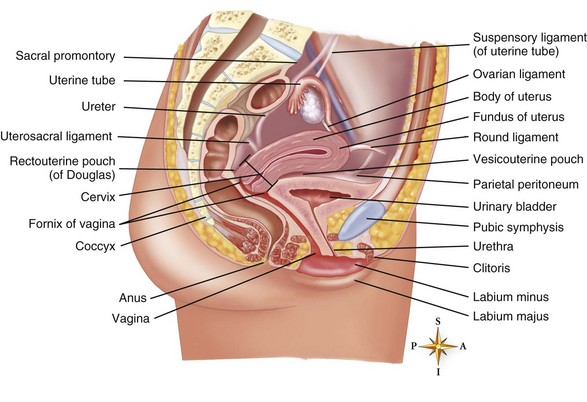
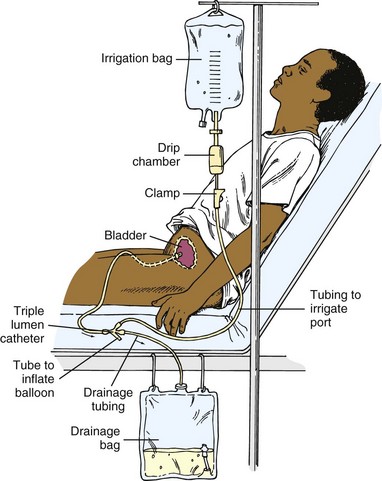
Chapter 12 (Figure 12-1: Structures of the male and female urinary systems) A Located behind peritoneum at level of last thoracic and first three lumbar vertebrae B Receive 20% of cardiac output during rest; reduced to 2% to 4% during physical or emotional stress 1. Anatomic and functional unit of kidney; approximately 1 million per kidney 2. Function via principles of filtration, reabsorption, and secretion (Figure 12-2: Overview of urine formation) a. Glomerulus: urine formation starts with filtration; water and solutes (except cellular elements of blood, albumins, fibrinogen, and other blood proteins) filter out of capillaries through glomerular-capsular membrane into the Bowman capsule b. Bowman capsule: filtrate collects here before flow to tubules c. Tubular reabsorption and secretion (a) Reabsorption of glucose and other nutrients mainly by active transport (b) Reabsorption of electrolytes from tubule filtrate to blood in peritubular capillaries; forms network of capillaries around tubules; cations (notably sodium) reabsorbed by active transport, stimulated by aldosterone; anions (notably chloride and bicarbonate) are reabsorbed by diffusion (c) Reabsorption of about 80% of water from tubular filtrate to blood by osmosis (2) Loop of Henle: osmotic condition promotes water reabsorption and transports chloride ions from filtrate, thus passively removing sodium ions with chloride (a) Reabsorption of electrolytes, particularly sodium; influenced by the mineralocorticoid aldosterone (b) Reabsorption of water into blood by osmosis; controlled by antidiuretic hormone (c) Secretion of hydrogen, potassium, and ammonia from blood in peritubular capillaries to tubular filtrate, via active transport D Collecting tubules: final osmotic reabsorption of most of remaining water in urine; under antidiuretic hormone influence E Urine description/composition 1. 1.5 L/day average (30 mL/hr) 3. Aromatic odor: food and drugs alter odor and color 4. Specific gravity of 1.005 to 1.030; varies depending on fluid intake and quantity of solutes; lower specific gravity the more dilute the urine; higher specific gravity the more concentrated the urine 6. Urea/uric acid: waste products of protein and amino acid metabolism 7. Creatinine: waste product of muscle metabolism 8. Electrolytes: potassium, sodium, calcium, and chloride 9. Hormones and their breakdown products 10. Abnormal constituents: glucose, protein, red blood cells (RBCs), ketone bodies, bilirubin, calculi, and white blood cells (WBCs) 1. Glomerular filtration rate (GFR): usually constant (about 125 mL/min); in certain pathologic conditions GFR may change markedly and alter urine volume (e.g., in shock GFR decreases, causing oliguria; decrease in plasma proteins lowers colloid oncotic pressure, increasing GFR) 2. Solutes in tubular filtrate: increase in tubular solutes causes decreased osmosis of water from proximal tubule into blood resulting in increased urine volume (e.g., with diabetes, excess glucose in tubular filtrate leads to increased urine volume [polyuria, diuresis]) 3. Aldosterone mechanism: stimulates kidney tubules to reabsorb sodium; water follows the sodium 4. Antidiuretic hormone (ADH): produced in hypothalamus and secreted into blood by posterior pituitary gland; secretion stimulated by increase in osmotic pressure of extracellular fluid or decrease in volume of extracellular fluid; ADH acts on distal and collecting tubules, causing water to move via osmosis from tubular filtrate into blood; increased water reabsorption increases total volume of body fluid by decreasing urine volume G Control of amount of blood flow through kidneys (Figure 12-3: Male reproductive organs) A Testes: male sex glands (gonads) 1. Seminal vesicles: secrete fluid that constitutes about 30% of semen 2. Prostate gland: secretes about 60% of semen; secretion is alkaline, which increases sperm motility; contains the enzyme acid phosphatase; this enzyme increases in metastasizing cancer of prostate 3. Bulbourethral glands (Cowper glands): secrete fluid that lubricates urethra before ejaculation A Epididymis: conducts semen from testes to vas deferens; sperm mature while semen is stored before ejaculation B Vas deferens (seminal ducts): conduct sperm and fluid from each epididymis to an ejaculatory duct C Ejaculatory ducts: ejaculate semen into urethra D Urethra: see description under Structures of the Urinary System 1. Scrotum: contains testes, epididymis, and first part of seminal duct; sperm develop at 2 to 3 degrees below body temperature (ideal for sperm development) 2. Penis: contains urethra; contains vascular spaces that when filled with blood cause erection B Internal: fibrous tubes (spermatic cords) located in each inguinal canal; torsion of testes twists cords, destroys sperm, interrupts blood supply, and can result in cell death and gangrene A Enterobacter aerogenes: gram-negative bacillus; causes urinary tract infections B Haemophilus ducreyi: gram-negative bacillus; causes venereal ulcer called chancroid (soft chancre) C Neisseria gonorrhoeae: gram-negative diplococcus; causes gonorrhea; transmitted sexually D Pseudomonas aeruginosa: gram-negative bacillus; infection characterized by blue-green pus; common secondary invader of wounds, burns, outer ear, and urinary tract; transmitted by catheters and other hospital instruments if contaminated E Treponema pallidum: motile spirochete; causes syphilis; transmitted sexually F Chlamydia trachomatis: parasite characterized as bacteria because of cell wall composition and process of reproduction; reproduce only within cells; causes genital infections in men and women; transmitted sexually A Human immunodeficiency virus (HIV): causes acquired immunodeficiency syndrome (AIDS); primarily transmitted sexually and by blood and other body fluids B Herpesvirus hominis: causes herpes genitalis; transmitted via genital or oral-genital routes C Human papillomavirus (genital or venereal warts [condylomata acuminata]): characterized by papillary or cauliflower-like masses in or on genitourinary structures; may be precursor to cancer of cervix; vaccine available 1. Antibacterial effect on renal tissue, ureters and bladder 2. Used to treat local urinary tract infections B Examples: nitrofurantoin (Macrobid, Macrodantin) C Major side effects: anorexia, nausea, vomiting (irritation of gastric mucosa); pseudomembranous colitis; photosensitivity; peripheral neuropathy; blood dyscrasias; hemolytic anemia; hypersensitivity reactions; pneumonitis; chest pain 1. Administer with meals to reduce gastrointestinal (GI) irritation 2. Monitor blood work, cultures, and urinary output 3. Encourage increased fluid intake to promote drug excretion 4. Nitrofurantoins: dilute oral suspensions in milk or juice to prevent staining of teeth; instruct that urine will appear brown 1. Hormones that promote secondary sex characteristics in men; have anabolic properties; stimulate building and repair of body tissue 2. Used in debilitating conditions and inoperable breast cancer; restore hormone levels in males; treat fibrocystic breast disease, dysmenorrhea, and severe postpartum breast engorgement in nonbreastfeeding mothers 3. Available in oral, parenteral (intramuscular [IM], subcutaneous [Sub-Q]), and buccal preparations B Examples: fluoxymesterone, danazol 1. Weight gain, edema (sodium and water retention); changes in libido (androgen effect); hoarseness, deep voice (virilism—androgen effect); gastroenteritis; emotional lability 2. Fluoxymesterone: hepatocellular carcinoma, acne, dyspepsia, jaundice, hypoglycemia, hypercalcemia 1. Assess for virilization in females; gynecomastia in men 2. Encourage diet high in calories and proteins to aid in building body tissues and low in sodium to limit edema 3. Administer with meals to reduce GI irritation 5. Assess for potentiation of anticoagulant effect when receiving concomitant anticoagulant therapy 1. Sterile introduction of catheter through urethra into bladder 2. Intermittent (straight) catheterization: to drain urine, obtain urine specimen, or determine residual volume (amount of urine left in bladder after voiding) 3. Indwelling (retention) catheterization: inflated balloon holds catheter in place; attached to collecting bag; urine is continually emptied by gravity 1. Explain procedure; provide privacy 2. Position client: female—supine with knees flexed and abducted; male—supine with knees slightly abducted 3. Use sterile technique; test balloon by inflating and deflating before insertion 4. Place sterile fenestrated drape over external genitalia, exposing meatus 5. Cleanse urinary meatus using cotton balls saturated with suitable solution a. Female: separate labia minora with thumb and forefinger and cleanse from anterior to posterior using one pledget for each stroke (keep labia separated during cleansing) b. Male: hold penis between thumb and forefinger perpendicular to body and cleanse from meatus to shaft using one pledget for each stroke (retract foreskin during procedure and replace after procedure) 6. Insert lubricated catheter into bladder a. Female: about 3 inches (7.5 cm) or slightly past point at which urine returns b. Male: about 7 to 10 inches (17 to 25 cm) or well past point at which urine returns c. Attempt balloon inflation; if resistance is met, deflate balloon, insert catheter farther, and reattempt inflation 7. Drain urine slowly by gravity a. Intermittent catheterization: remove catheter when bladder is empty b. Retention catheterization: inflate balloon with sterile solution and place closed collection system below level of bladder; hang bag from bed frame, not siderails 8. Assist to comfortable position and document procedure 9. Ensure patency of catheter (e.g., eliminate kinks, dependent loops, and clogs); secure catheter to client’s leg to prevent telescoping action in urethra 10. Wash genital area with soap and water daily and as necessary 11. Keep system closed at all times; collect urine specimen from port along tubing using sterile technique 12. Monitor output hourly if critically ill 13. Prepare for removal of indwelling catheter by intermittently clamping tubing to restore muscle tone; dribbling and incontinence may occur temporarily after catheter is removal due to flaccidity of urinary sphincter; monitor for urinary output of sufficient quantity (200 mL or more) within 6 to 8 hours after removal 1. Instillation of sterile isotonic solution into bladder through triple-lumen catheter: one for instillation of fluid into balloon tip, one for instillation of fluid into bladder, and one for return of fluid and urine from bladder (Figure 12-5: Continuous bladder irrigation) 2. Prevents occlusion of catheter by clots; used to administer local antibiotic treatment 1. Connect catheter port to irrigant via intravenous tubing using sterile technique 2. Set rate of infusion as ordered (e.g., flow should be sufficient to keep drainage pink); if red, bloody drainage or clots occur, CBI should be increased to achieve pink drainage; assess for occlusion if urinary output stops abruptly 3. Maintain infusion continuously, observing color, clarity, and amount of drainage 4. Assess for clinical findings of dilutional hyponatremia 5. Deduct irrigant from total urinary output to calculate actual urine output For additional disorders see Chapter 24, Nursing Care Related to Major Disorders Affecting Women’s Health A Etiology and pathophysiology 1. Cystitis: inflammation of bladder wall usually caused by ascending bacterial infection (Escherichia coli most common) a. Females: more common because of shorter urethra, childbirth, anatomic proximity of urethra to rectum b. Males: secondary to epididymitis, prostatitis, renal calculi 2. Urethritis: inflammation of urethra caused by staphylococci, E. coli, Pseudomonas species, and streptococci a. Although inflammation is present, clinical findings are similar to gonorrheal urethritis, sexual contact is not the cause 3. Urosepsis: caused by gram-negative bacteria 1. Subjective: urgency; frequency; pain when initiating, during, and completion of urination; males—prostate tenderness with rectal exam 2. Objective: nocturia, hematuria, pyuria, cloudy urine, positive urine culture; males—prostate enlargement with rental exam 1. Urine culture: to identify causative organism 2. Pharmacologic therapy: antibiotics, urinary antiseptics, antispasmodics 3. Diet: directed toward altering properties of urine (e.g., cranberry juice—contributes to hostile environment for bacterial growth; elimination of caffeine, which causes bladder irritability) 4. Additional fluids: dilute urine 5. Warm sitz baths: provides comfort 6. Antiseptic solution: installation via urethral catheter 7. Urosepsis: IV therapy with aminoglycosides; beta-lactam antibiotics, aztreonam (Azactam); used with probenecid to increase therapeutic level of drug
Nursing Care of Clients with Urinary/Reproductive System Disorders
Overview
Review of Anatomy and Physiology of the Urinary System
Structures of the Urinary System
Kidneys
Review of Anatomy and Physiology of the Reproductive System
Structures of the Male Reproductive System
Glands
Ducts
Supporting Structures
Review of Microorganisms
Bacterial Pathogens
Viral Pathogens
![]() Related Pharmacology
Related Pharmacology
Kidney-Specific Antiinfectives
Urinary Spasmolytics
Androgens
Related Procedures
Urinary Catheterization
Continuous Bladder Irrigation (CBI)
Major Disorders of Urinary/Reproductive Systems
Urinary Tract Infections (UTIs)
Data Base