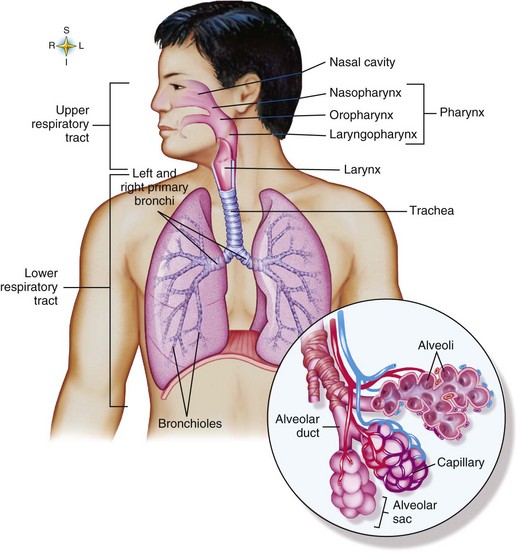
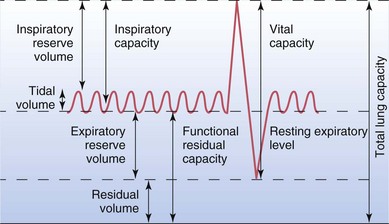
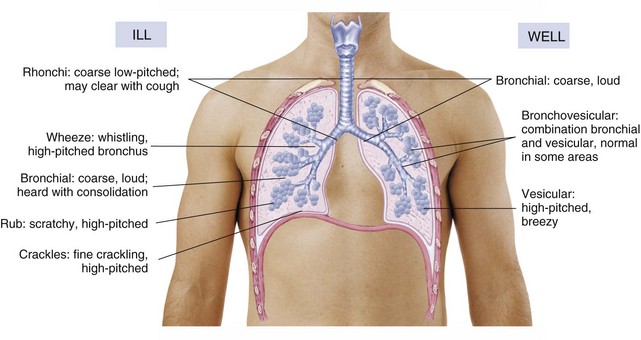
Chapter 7 (Figure 7-1: The respiratory system) A Upper portion of respiratory system filters, moistens, and warms air during inspiration 1. Nose: lining consists of ciliated mucosa; divided by septum; turbinates (conchae) projected from lateral walls; contains olfactory receptors for smell; aids in phonation 2. Paranasal sinuses drain into nose: frontal, maxillary, sphenoidal, ethmoidal; aid in phonation 3. Pharynx: nasopharynx, oropharynx, and laryngopharynx; composed of muscle with mucous lining; contains tonsils, adenoids, and other lymphoid tissue that help destroy incoming bacteria 4. Larynx: formed by cartilage including thyroid cartilage (Adam’s apple), epiglottis (lid cartilage), cricoid (signet ring cartilage), and vocal cords (fibroelastic bands stretched across hollow interior of larynx); paired vocal cords (folds) and posterior arytenoid cartilages form the glottis; voice production—during expiration, air passing through larynx causes vocal cords to vibrate; short, tense cords produce a high pitch; long, relaxed cords, a low pitch 5. Trachea: smooth muscle walls contain C-shaped rings of cartilage that keep it open at all times; lined with ciliated mucosa; extends from larynx to bronchi; 10 to 12 cm long; furnishes open passageway for air going to and from lungs B Lower portion of respiratory system consists of lungs, which enable exchange of gases between blood and air to regulate arterial PO2, PCO2, and pH; left lung has two lobes and right lung has three lobes 1. Bronchi: right and left, formed by branching of trachea; right bronchus slightly larger and more vertical than left; each primary bronchus branches into segmental bronchi in each lung; primary and segmental bronchi contain C-shaped cartilage 2. Bronchioles: small branches off secondary bronchi, distinguished by lack of C-shaped cartilage and a duct diameter of about 1 mm; bronchi further branch into terminal bronchioles, respiratory bronchioles, and then alveolar ducts 3. Alveoli: microscopic sacs composed of a single layer of squamous epithelial cells (type I cell) enveloped by a network of pulmonary capillaries that allow for rapid gas exchange; type II cells produce surfactant to prevent alveolar collapse, and type III cells are macrophages that protect against bacteria by phagocytosis 4. Covering of lung: visceral layer of pleura that joins with parietal pleura lining the thorax and diaphragm; space between these two linings is the pleural space and contains a small amount of fluid to eliminate friction; negative pressure in pleural space relative to atmospheric pressure is essential for breathing 1. Following phrenic nerve stimulation, diaphragm and other respiratory muscles contract 3. Intrathoracic and intrapulmonic pressures decrease 4. Air rushes from positive pressure in atmosphere to negative pressure in alveoli 5. Inspiration is completed with stimulation of stretch receptors 6. Expiration occurs passively as a result of recoil of elastic lung tissue 1. Alveolar stretch receptors respond to inspiration by sending inhibitory impulses to inspiratory neurons in brainstem that prevent lung overdistention (Hering-Breuer reflex) 2. Central and peripheral chemoreceptors stimulate respirations in response to lowered pH, increased PCO2, or decreased PO2 3. Medulla oblongata and pons control rate and depth of respirations C Amount of air exchanged in breathing 1. Directly related to gas pressure gradient between atmosphere and alveoli 2. Inversely related to resistance that opposes airflow 3. Positions such as orthopneic and semi- to high-Fowler lower abdominal organs and reduce pressure against diaphragm 4. Influenced by lung volumes and capacities (pulmonary function evaluated with a spirometer: see Figure 7-2: Lung volumes and capacities) a. Tidal volume: average amount expired after a regular inspiration; expected volume is approximately 500 mL b. Expiratory reserve volume (ERV): largest additional volume of air that can be forcibly expired after a regular inspiration and expiration; expected volume is 1000 to 1200 mL c. Inspiratory reserve volume (IRV): largest additional volume of air that can be forcibly inspired after a regular inspiration; expected volume is 3000 mL d. Residual volume: air that cannot be forcibly expired voluntarily from lungs; expected volume is 1200 mL; increased in chronic obstructive pulmonary disease (COPD) as lungs lose elasticity and ability to recoil, resulting in air trapping e. Vital capacity: amount of air that can be forcibly expired after forcible inspiration; varies with size of thoracic cavity, which is determined by various factors (e.g., size of rib cage, posture, volume of blood and interstitial fluid in lungs, size of heart); expected capacity is about 4600 mL; decreased with COPD, neuromuscular disease, atelectasis f. Forced expiratory volume (FEV): volume of air that can be forcibly exhaled within a specific time, usually 1 second; expected volume is decreased with increased airway resistance (e.g., bronchospasm, COPD) g. Inspiratory capacity: largest amount of air that can be inspired after a regular exhalation; expected capacity is about 3500 mL h. Functional residual capacity: amount of air left in the lungs after a regular exhalation; expected capacity is about 2300 mL; increased with COPD i. Total lung capacity: amount of air in lungs after maximum inhalation; equal to sum of tidal volume, residual volume, and inspiratory and expiratory reserve volumes; expected capacity is about 5800 mL; increased with COPD; decreased with atelectasis and pneumonia D Diffusion of gases between air and blood 1. Occurs across alveolar-capillary membranes (in lungs between air in alveoli and venous blood in lung capillaries); adequate diffusion depends on a balanced ventilation-perfusion (V/Q) ratio a. Oxygen: net diffusion toward lower oxygen pressure gradient (from alveolar air to blood) b. Carbon dioxide: net diffusion toward lower carbon dioxide pressure gradient (from blood to alveolar air) a. Expected: balance between alveolar ventilation and capillary blood flow to facilitate gas exchange b. Low V/Q ratio: alveoli are poorly ventilated, but capillary blood flow is adequate; blood is shunted past alveoli without adequate gas exchange (e.g., atelectasis, pneumonia) c. High V/Q ratio: alveolar ventilation is adequate, but capillary blood flow is not; adequate gas exchange does not take place because of dead space (e.g., pulmonary embolism, cardiogenic shock) d. Absence of ventilation and perfusion: causes a silent unit with no gas exchange (e.g., pneumothorax) E Blood transports oxygen as a solute and primarily as oxyhemoglobin; oxygen saturation of hemoglobin (SaO2) is 95% to 100% F Blood transports carbon dioxide 1. Primarily as a bicarbonate ion (HCO3−) formed by ionization of carbonic acid; in lungs the molecule splits in the presence of carbonic anhydrase to form carbon dioxide (CO2) and water (H2O); CO2 diffuses into the alveoli and the majority of water is retained G Normal breath sounds (Figure 7-3: Breath sounds in the ill and well client) 1. Bronchial sounds (over trachea, larynx): result of air passing through larger airways; sounds are loud, harsh, high-pitched; expiration longer than inspiration 2. Vesicular sounds (over entire lung field except large airways): result of air moving in and out of alveoli; may reflect sound of air in larger passages that is transmitted through lung tissue; sounds are quiet, low-pitched; inspiration longer than expiration 3. Bronchovesicular sounds (near main stem bronchi); result of air moving through smaller air passages; sounds are moderately pitched, breezy; inspiratory and expiratory phases equal H Adventitious breath sounds (see Figure 7-3) a. Result of sudden opening of small airways and alveoli that contain fluid b. Short, high-pitched bubbling sounds; sounds may be simulated by rubbing a few strands of hair between fingers next to the ear c. Most common during height of inspiration a. Rush of air passing through airway intermittently occluded by mucus b. Short, low-pitched bubbling sounds c. Most common on inspiration and at times expiration a. Result of air passing through narrowed small airways b. Sounds are high-pitched and musical (sibilant wheezes), or low-pitched and rumbling (sonorous wheezes or rhonchi) d. Associated with asthma and with conditions that cause partial obstruction of airway by mucus, foreign body, or tumor 1. Bordetella pertussis: small, gram-negative coccobacillus; causes pertussis or whooping cough 2. Streptococcus pneumoniae: gram-positive, encapsulated diplococcus; causes pneumococcal pneumonia; often responsible for sinusitis, otitis media, and meningitis 3. Haemophilus influenzae: small, gram-negative, highly pleomorphic bacillus; causes acute meningitis and upper respiratory tract infections 4. Klebsiella pneumoniae (Friedländer’s bacillus): gram-negative, encapsulated, non–spore-forming bacillus; causes pneumonia and urinary tract infections 5. Mycobacterium tuberculosis (tubercle bacillus): acid-fast actinomycete causes tuberculosis (TB) 6. Pseudomonas aeruginosa: gram-negative, non–spore-forming bacillus; often cause of facility-acquired infections; respiratory equipment can be source; causes pneumonia, urinary tract infections, and sepsis that complicates severe burns 7. Staphylococcus aureus: gram-positive coccus; misuse of antimicrobial agents led to emergence of methicillin-resistant Staphylococcus aureus (MRSA) B Rickettsial pathogen: Coxiella burnetii; only Rickettsia species not associated with a vector; causes Q fever, an infection clinically similar to primary atypical pneumonia 1. DNA viruses: adenoviruses cause acute respiratory tract disease, adenitis, pharyngitis, and other respiratory tract infections, as well as conjunctivitis a. Coronaviruses: frequently associated with a mild upper respiratory tract infection; severe acute respiratory syndrome (SARS) associated coronavirus (SARS-CoV) causes an atypical pneumonia with a high morbidity and mortality b. Picornaviruses: cause poliomyelitis, Coxsackie disease, common cold c. Retroviruses: invade T lymphocytes and are associated with malignancies, human immunodeficiency virus (HIV), and acquired immunodeficiency syndrome (AIDS) d. Orthomyxoviridae (influenza viruses): frequently associated with influenza (flu); a novel strain of influenza A virus (H1N1) was responsible for the 2009 flu pandemic 1. Histoplasma capsulatum: dimorphic fungus producing chlamydospores in infected tissue; causes histoplasmosis 2. Aspergillus fumigatus: rapidly proliferating fungus found in soil; inhalation of spores can cause pneumonia 3. Pneumocystis jiroveci: unicellular organism thought to be transmitted by airborne droplets; causes pneumonia 1. Reverse bronchoconstriction, thus opening air passages in lungs 2. Stimulate beta-adrenergic sympathetic nervous system receptors, relaxing bronchial smooth muscle, or inhibiting inflammation and reducing edema 3. Available in oral, parenteral (intramuscular [IM], subcutaneous [Sub-Q], IV), rectal, and inhalation preparations 1. Beta agonists act at beta-adrenergic receptors in bronchi and bronchioles to relax smooth muscle; this increases respiratory volume and inhibits histamine release from mast cells suppressing reaction to allergens; e.g., albuterol (Proventil); isoproterenol (Isuprel); epiNEPHrine (Adrenalin, Sus-Phrine); metaproterenol (Alupent); terbutaline (Brethine); salmeterol (Serevent), which is long-acting 2. Xanthines act directly on bronchial smooth muscle, decreasing spasm and relaxing smooth muscle of the vasculature; are used less frequently because of side effects and drug interactions; e.g., aminophylline, theophylline (Elixophyllin, Theo-Dur), oxtriphylline (Choledyl), dyphylline (Dilor) 3. Anticholinergics inhibit action of acetylcholine at receptor sites on bronchial smooth muscle and prevent bronchospasm; e.g., ipratropium (Atrovent) 4. Inhaled steroids exert antiinflammatory effect on airways; e.g., fluticasone (Flovent, Flonase); budesonide (Pulmicort Turbuhaler); beclomethasone (Beclovent, Beconase, Vanceril); triamcinolone (Azmacort); combination product—fluticasone and salmeterol (Advair Diskus) 5. Leukotriene receptor antagonists block action of leukotriene to reduce bronchoconstriction and inflammation associated with asthma; e.g., montelukast (Singulair), zafirlukast (Accolate), zileuton (Zyflo) C Major side effects: dizziness (decrease in blood pressure); central nervous system (CNS) stimulation (sympathetic stimulation); palpitations and hypertension (beta-adrenergic stimulation); gastric irritation (local effect) 1. Question if prescribed for clients with hypertension, hyperthyroidism, and cardiovascular dysfunction 2. Question if prescribed concurrently with CNS stimulants (adrenergics) and bronchoconstricting agents (beta blockers) 3. Administer with food during waking hours 4. Assess vital signs, breath sounds, oxygen saturation with pulse oximeter 5. Assess intake and output (I&O) 6. Teach use of metered-dose inhalers (MDIs), spacers, and peak flow meters: rinse mouthpiece, cap, and mouth after each use; oropharyngeal fungal infections are common with inhaled steroids 7. Explain importance of adhering to therapy to decrease need for short-acting beta agonists 8. Explain that stimulants and some over-the-counter medications should be avoided because they may act as antagonists 1. Liquefy secretions in respiratory tract, promoting a productive cough 2. Mucolytics act directly to break up mucus plugs in tracheobronchial passages; available in inhalation preparations (oral form of acetylcysteine is used to treat acetaminophen toxicity) 3. Expectorants act indirectly to liquefy mucus by increasing respiratory tract secretions via oral absorption; available in oral preparations B Examples: mucolytic—acetylcysteine (Mucomyst); expectorants—guaifenesin (Mucinex); potassium iodide (SSKI) C Major side effects: gastrointestinal (GI) irritation (local effect); skin rash (hypersensitivity); oropharyngeal irritation and bronchospasm with mucolytics 2. Inhibit cough reflex either by direct action on medullary cough center or by indirect action peripherally on sensory nerve endings B Examples: opioid—codeine, hydrocodone (Hycodan); dextromethorphan hydrobromide (Robitussin), benzonatate (Tessalon); diphenhydrAMINE (Benadryl) is an antihistamine that may be used for coughs C Major side effects: drowsiness (CNS depression); nausea (GI irritation); dry mouth (anticholinergic effect of antihistamine in combination products) 1. Provide adequate fluid intake 2. Avoid offering fluids immediately after administering liquid preparations 3. Encourage high-Fowler position 4. Question if prescribed postoperatively, concurrently with CNS depressants, or for clients with a head injury or asthma 5. Maintain safety precautions after administration; teach to avoid hazardous activity 1. Block action of histamine at H1 receptor sites via competitive inhibition; exert antiemetic, anticholinergic, and CNS depressant effects 2. Relieve symptoms of the common cold and allergies that are mediated by histamine B Examples: brompheniramine (Dimetane); diphenhydrAMINE (Benadryl); loratadine (Claritin); fexofenadine (Allegra); cetirizine (Zyrtec) 1. Drowsiness and dizziness particularly for first-generation antihistamines (CNS depression); GI irritation (local effect); dry mouth (anticholinergic effect) 1. Treat TB; administered in combination (first-line and second-line drugs) over a prolonged time period to reduce possibility of mycobacterial drug resistance a. Ethambutol (Myambutol): interferes with mycobacterial RNA synthesis b. Isoniazid (INH, Nydrazid): interferes with mycobacterial cell-wall synthesis c. Pyrazinamide (PZA): bacteriostatic; mechanism unknown d. Rifampin (Rifadin), rifabutin (Mycobutin), rifapentine (Priftin): interfere with mycobacterial RNA synthesis e. Streptomycin sulfate: inhibits mycobacterial protein synthesis f. Combination drugs: isoniazid (INH)/rifampin (Rifamate); INH/rifampin/PZA (Rifater) 2. Second-line drugs inhibit mycobacterial cell metabolism: capreomycin (Capastat) and cycloserine (Seromycin) 1. GI irritation (direct tissue irritation) 2. Suppressed absorption of fat and B complex vitamins, especially folic acid and B12; depletion of vitamin B6 by INH 4. CNS disturbances (direct CNS toxic effect) 5. Hepatotoxicity (direct liver toxic effect) 6. Blood dyscrasias (decreased red blood cells [RBCs], white blood cells [WBCs], platelet synthesis) 7. Streptomycin: ototoxicity (direct auditory [eighth cranial] nerve toxic effect); nephrotoxicity 8. Ethambutol: visual disturbances (direct optic [second cranial] nerve toxic effect) 9. Rifampin: orange-red discoloration of all body fluids; increases metabolism of corticosteroids, opioids, warfarin (Coumadin), oral contraceptives, and hypoglycemics 1. Support natural defense mechanisms; encourage intake of foods rich in immune-stimulating nutrients (e.g., vitamins A, C, and E, and the minerals selenium and zinc) 2. Obtain sputum specimens for acid-fast bacillus 3. Monitor blood work during therapy (e.g., liver enzymes) 4. Instruct to take medications as prescribed; reinforce need for medical supervision; when adherence to the therapeutic regimen is an issue, mandated directly observed therapy ensures treatment is ongoing 5. Offer emotional support during long-term therapy 6. Use safety precautions (e.g., supervise ambulation) if CNS effects are manifested 7. Instruct regarding nutritional side effects of medications and encourage foods rich in B complex vitamins 8. Encourage to avoid alcohol during therapy 9. Ethambutol: encourage frequent visual examinations 10. Rifampin: teach that body fluids may appear orange-red; monitor for drug interactions; decreases effectiveness of oral contraceptives 11. Streptomycin: encourage frequent auditory examinations 12. INH: administer pyridoxine as prescribed to prevent neuritis 13. Instruct to avoid exposing others to respiratory droplets from coughing and to dispose of tissues in a moisture-proof container until no longer contagious (2 to 8 weeks) A Definition: short, abrupt pressure against abdomen, two fingerbreadths above umbilicus, to raise intrathoracic pressure; external compression forces out residual lung volume, which will dislodge the obstruction, such as a bolus of food or a foreign body B Signs and symptoms of obstruction 1. Partial: noisy respirations, stridor, dyspnea, light-headedness, dizziness, flushing of face, bulging of eyes, repeated coughing 2. Total: universal choking sign (thumb and forefinger encircling throat), cessation of breathing, inability to speak or cough, extension of head, facial cyanosis, bulging of eyes, panic, unconsciousness 1. Assess no longer than 3 to 5 seconds b. Determine whether person can speak or cough c. Observe for universal choking sign d. Assess respirations: observe for rise and fall of chest; listen for escape of air from nose and mouth on expiration; feel for flow of air from nose and mouth 2. Initiate intervention for a partial obstruction a. Allow individual’s expulsive cough to dislodge obstruction b. Remove foreign bodies coughed up into the mouth c. Assess for signs of total obstruction d. Activate emergency medical service (EMS) system if person is having difficulty breathing 3. Initiate intervention for a total obstruction a. Standing behind the conscious person, encircle waist and thrust upward and inward against diaphragm with intertwined clenched fists; repeat thrusts until object is expelled or the person becomes unresponsive b. If person becomes unconscious, activate EMS system c. Begin cardiopulmonary resuscitation (CPR) d. Determine patency of airway; remove foreign objects from mouth; attempt rescue breathing e. If an airway cannot be established, an emergency cricothyrotomy may be necessary 1. Visualization of tracheobronchial tree via a scope advanced through mouth or nose into bronchi 2. Performed to remove foreign body, remove secretions, or obtain specimens of tissue or mucus for diagnostic study 2. Keep nothing by mouth (NPO) for 6 to 8 hours before procedure 3. Administer prescribed preprocedure medications to produce sedation and decrease anxiety 4. Inform to expect some soreness, dysphagia, and hemoptysis after procedure 5. Advise to avoid coughing or clearing throat 6. Observe for signs of hemorrhage and/or respiratory distress; keep head of bed elevated 7. Monitor vital signs until stable 8. Do not allow fluids until gag reflex returns; protect airway until local anesthetic dissipates A Definition: activities to mobilize respiratory secretions that may lead to atelectasis and/or pneumonia 1. Incentive spirometer: mechanical device that promotes maximum inspiration and loosens secretions; measures air inspired, provides visual feedback 2. Percussion (clapping): cupped hands repeatedly strike chest wall over congested areas; loosens secretions 3. Vibration: palmar surface of hands placed on chest over congested area and vibrated as client exhales; loosens secretions 4. Postural drainage: placed in various positions to permit gravity drainage of congested lung segments 1. Assess baseline breath sounds, oxygen saturation with pulse oximeter (maintain at 90% or more), and ability to tolerate procedure 2. Administer prescribed bronchodilators, mucolytics, analgesics a. Fowler position for incentive spirometry and to drain upper lung segments b. Side-lying and prone positions with head lower than affected segment for postural drainage 4. Teach use of incentive spirometer a. After exhaling, form seal around mouthpiece with lips b. Take slow, continuous deep breath and hold indicator afloat for several seconds before exhaling
Nursing Care of Clients with Respiratory System Disorders
Overview
Review of Anatomy and Physiology
Structures and Functions of the Respiratory System
Physiology of Respiration
Review of Microorganisms
![]() Related Pharmacology
Related Pharmacology
Bronchodilators and Antiasthmatics
Mucolytic Agents and Expectorants
Antitussives
Opioid Antagonist
Antihistamines
Antituberculars
Related Procedures
Abdominal Thrust (Heimlich Maneuver)
Bronchoscopy
Chest Physiotherapy
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



Nursing Care of Clients with Respiratory System Disorders
Get Clinical Tree app for offline access