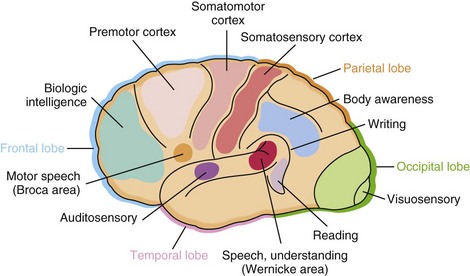
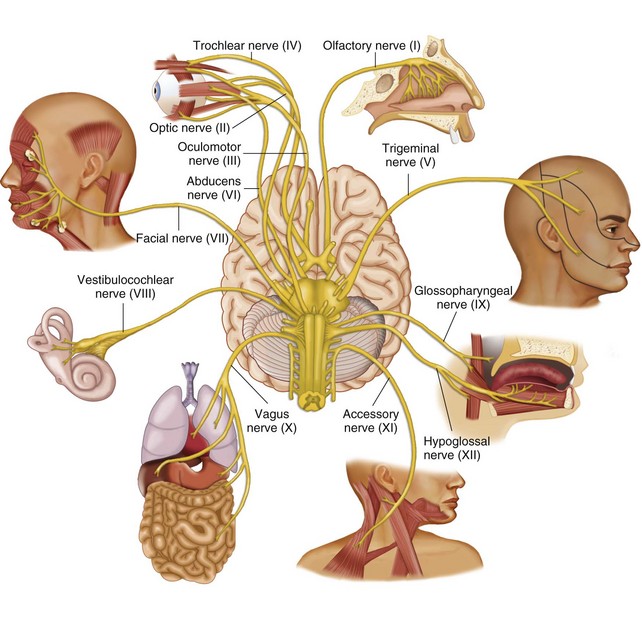
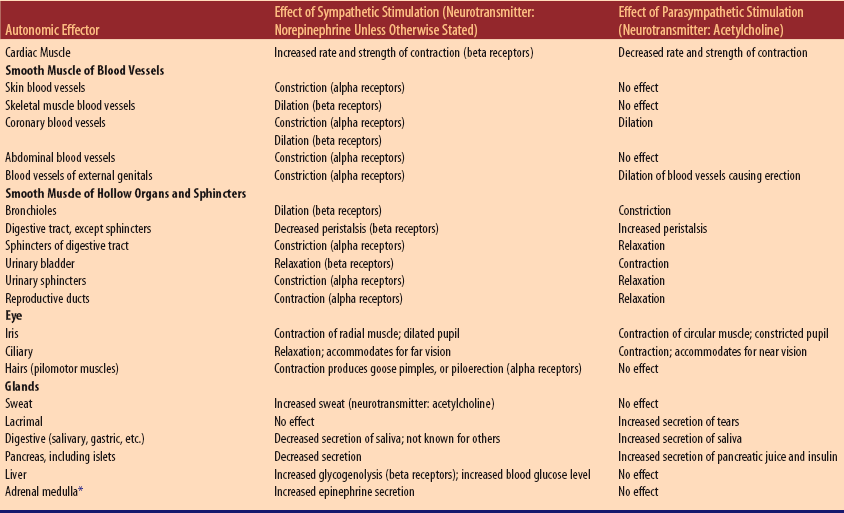
Chapter 11 Nerve cells: basic structural and functional units 1. Sensory (afferent) neurons: transmit impulses to spinal cord or brain 2. Motoneurons (efferent): transmit impulses away from brain or spinal cord to muscles or glands a. Upper motor neurons: located in CNS; destruction causes loss of voluntary control, muscle spasticity, and hyperactive reflexes b. Lower motor neurons: cranial and spinal efferent neurons that lie in gray matter of spinal cord and extend into the peripheral nervous system and end at myoneural junctions in muscles; destruction causes loss of voluntary control, muscle flaccidity, and loss of reflexes 1. Cell body: contains a nucleus and other cytoplasmic matter 2. Dendrite: carry impulses toward cell body 3. Axon: carries impulse away from cell body 4. Myelin: multiple, dense layers of membrane around an axon or dendrite; myelinated nerve fibers transmit nerve impulses more rapidly than nonmyelinated fibers 5. Nerve impulses are excitatory or inhibitory 1. Has large blood supply and high oxygen consumption 2. Uses glucose for energy metabolism, so hypoglycemia can alter brain function 3. Protected by blood-brain barrier, a selective filtration system that isolates the brain from certain substances in the general circulation 4. Basic tissue types: neuron cell aggregations (gray matter) and tracts of myelinated fibers (white matter) 1. Consists of medulla, pons, and midbrain 2. Conducts impulses between spinal cord and brain; most motor and sensory fibers decussate (cross over) in medulla 3. Contains reflex centers for heart, respirations, vomiting, coughing, and swallowing; controls blood vessel diameter C Cerebellum: exerts synergic control over skeletal muscles, producing smooth, precise movements; coordinates skeletal muscle contractions; promotes posture, equilibrium, and balance a. Crudely translates sensory impulses into sensations but does not localize them b. Processes motor information from cerebral cortex and cerebellum and projects it back to motor cortex c. Contributes to emotional component of sensations (pleasant or unpleasant) a. Part of neural path by which emotions and other cerebral functions can alter vital, automatic functions (e.g., heartbeat, blood pressure, peristalsis, and secretion by glands) b. Secretes neuropeptides that influence secretion of various anterior pituitary hormones c. Produces antidiuretic hormone (ADH) and oxytocin, which are secreted by the posterior pituitary d. Contains appetite center and satiety center e. Serves as a heat-regulating center by relaying impulses to lower autonomic centers for vasoconstriction, vasodilation, and sweating, and to somatic centers for shivering f. Maintains waking state; part of arousal or alerting neural pathway 3. Optic chiasm: point of crossing over (decussation) of optic nerve fibers E Cerebral cortex: consists of multiple lobes divided into two hemispheres covered by gray matter forming folds (convolutions) composed of hills (gyri) and valleys (sulci) (Figure 11-1: Cerebral cortex) a. Influences abstract thinking, sense of humor, and uniqueness of personality b. Controls contraction of skeletal muscles and synchronization of muscular movements c. Exerts control over hypothalamus; influences basic biorhythms d. Controls muscular movements necessary for speech (Broca area) a. Translate nerve impulses into sensations (e.g., touch, temperature) b. Interpret sensations; provide appreciation of size, shape, texture, and weight a. Translate nerve impulses into sensations of sound and interpret sounds (Wernicke’s area; usually in dominant hemisphere) F Brain and spinal cord protection 1. Vertebrae around cord; cranial bones around brain a. Dura mater: white fibrous tissue, outer layer b. Arachnoid: “cobwebby” middle layer c. Pia mater: innermost layer; adheres to outer surface of cord and brain; contains blood vessels a. Subarachnoid space: around brain and cord between arachnoid and pia mater b. Subdural space: between dura mater and arachnoid 4. Ventricles and cerebral aqueduct inside brain; four cavities known as first, second, third, and fourth ventricles Twelve pairs. (Table 11-1: Distribution and Function of Cranial Nerve Pairs and Figure 11-2: Cranial nerves) Table 11-1 Distribution and Function of Cranial Nerve Pairs* *NOTE: The first letters of the words in the following sentence are the first letters of the cranial nerves, and many generations of anatomy students have used it as an aid to memorizing the names: “On Old Olympus’ Towering Tops, A Finn and German Viewed Some Hops.” (There are several slightly different versions of the mnemonic.) Figure 11-2 Cranial nerves. (From Patton KT, Thibodeau GA: Anatomy and physiology, ed 7, St. Louis, 2010, Mosby.) 1. Inner core of gray matter shaped like a three-dimensional H 2. Long columns of white matter surround cord’s inner core of gray matter; namely, right and left anterior, lateral, and posterior columns; composed of numerous sensory and motor tracts 1. Sensory tracts conduct impulses up cord to brain (e.g., spinothalamic tracts, two of the six ascending tracts, conduct sensations of pain, temperature, vibration, and proprioception) 2. Motor tracts (pyramidal and extrapyramidal tracts) conduct impulses down cord from brain (e.g., the two corticospinal tracts decussate, controlling voluntary movement on side of body opposite the cerebral cortex from which the impulse initiated; three vestibulospinal tracts are involved with some autonomic functions) 3. Gray matter of cord contains reflex centers for all spinal cord reflexes A Thirty-one pairs, each containing a dorsal root and a ventral root B Branches of spinal nerves form intricate networks of fibers (e.g., brachial plexus), from which nerves emerge to supply various parts of skin, mucosa, and skeletal muscles C All spinal nerves are composed of both sensory dendrites (dorsal root) and motor axons (ventral root) A Conducts impulses from brainstem or cord out to visceral effectors (e.g., cardiac muscle, smooth muscle, and glands) 1. Sympathetic (adrenergic fibers) secretes norepinephrine: influences heart, smooth muscle of blood vessels and bronchioles, and glandular secretion 2. Parasympathetic (cholinergic fibers) secretes acetylcholine: influences digestive tract and smooth muscle to promote digestive gland secretion, peristalsis, and defecation; influences heart to decrease rate and contractility C Autonomic antagonism and summation: sympathetic and parasympathetic impulses tend to produce opposite effects (Table 11-2: Autonomic Functions) Table 11-2 *Sympathetic preganglionic axons terminate in contact with secreting cells of the adrenal medulla. Thus, the adrenal medulla functions, to quote someone’s descriptive phrase, as a “giant sympathetic postganglionic neuron.” (From Patton KT, Thibodeau GA: Anatomy and physiology, ed 7, St. Louis, 2010.) D Under conditions of stress, sympathetic impulses to visceral effectors dominate over parasympathetic impulses; however, in some individuals under stress, parasympathetic impulses via the vagus nerve increase to glands and smooth muscle of the stomach, stimulating hydrochloric acid secretion and gastric motility A Sodium-potassium pump: transports sodium out and potassium into cells; requires adenosine triphosphate (ATP) to function B Resting potential: exists when cells are in an unstimulated or resting state C Action potential: composed of depolarization and repolarization; known as the nerve impulse D Reflex arc: pathway to spinal cord and back to effector organ that elicits a single, specific response; primitive nerve activity E Types of neurotransmitters (there are at least 30 types) 1. Monoamines (e.g., norepinephrine, dopamine, serotonin, acetylcholine); axons that release acetylcholine are called cholinergic; those that release norepinephrine are called adrenergic 2. Amino acids (gamma-aminobutyric acid [GABA], glutamic acid, glycine, taurine); GABA is most common inhibitory transmitter in the brain 3. Neuropeptides (e.g., vasopressin, enkephalins, and endorphins); some influence hormone levels and others affect perception and integration of pain and emotional experience 4. Prostaglandins: some inhibit and some excite; may moderate actions of other transmitters by influencing the neuronal membrane 1. Taste buds consist of receptors connected to cranial nerves VII and IX 2. Responds to sweet at tongue tip; sour and salt at tip and sides; bitter at back 1. Receptors in epithelium of nasal mucosa; odors sensed as chemicals interact with receptors on sensory hairs of olfactory cells 1. Outer layer: sclera and cornea; middle layer: choroid, which includes iris, ciliary body, ciliary muscles, and suspensory ligaments holding the lens; inner layer: retina 2. Anterior cavity contains aqueous humor; posterior cavity contains vitreous humor 3. Extrinsic muscles move eyeball in various directions; intrinsic muscles (e.g., ciliary muscles) control size of pupil and shape of lens, accomplishing accommodation 4. Accessory structures (provide protection): eyebrows, eyelashes, lacrimal apparatus, and eyelids; lined with mucous membrane (conjunctiva) that continues over surface of eyeball; inner and outer canthi at junction of eyelids a. Refraction, accommodation, and constriction of pupils: necessary to focus image on retina b. Binocular vision: visual fields of two eyes overlap; although each eye sees some areas of the environment that the other eye cannot, both eyes see large areas in common; human brain interprets these overlapping fields in terms of depth; optic chiasm is site of crossover of fibers of optic nerves, permitting binocular vision c. Stimulation of retina: rods considered receptors for night vision; cones are receptors for daylight and color vision; macula lutea, center of retina, receives and analyzes light only from center of visual field and contains fovea centralis where cones are concentrated d. Conduction to visual area in occipital lobe of cerebral cortex by fibers of cranial nerve II and optic tract 1. External ear: consists of auricle (or pinna), external acoustic meatus (ear opening), and external auditory canal 2. Middle ear: separated from external ear by tympanic membrane; middle ear contains auditory ossicles (malleus, incus, stapes) and openings from eustachian tubes, mastoid cells, external ear, and internal ear a. Vestibule contains maculae acusticae; vestibular nerve (branch of eighth cranial [acoustic or vestibulocochlear] nerve); provides information about equilibrium, position of head, and acceleration and deceleration b. Semicircular canals contain crista ampullaris, sense organ for sensations of equilibrium and head movements c. Cochlea contains membranous cochlear duct located in organ of Corti, the hearing sense organ; cochlear nerve (branch of eighth cranial nerve) supplies organ of Corti a. Sound waves strike tympanic membrane, causing it to vibrate; vibrations sequentially move the malleus, incus, and stapes b. Movement of stapes against oval window starts a ripple in perilymph, which is transmitted to endolymph inside the cochlear duct; this stimulates organ of Corti c. Cochlear nerve conducts impulses from organ of Corti to brain; hearing occurs when impulses reach the auditory area in temporal lobe of cerebral cortex A Purpose: movement, posture, and heat production B Types of muscles and neural control 1. Striated: controlled by voluntary nervous system 2. Smooth: controlled by autonomic nervous system; not under voluntary control C Bursa: synovial fluid-filled sac situated where friction occurs; facilitates movement of tendons over bone, relieving pressure between moving parts D Tendons: bands of fibrous tissue connecting muscle to bone E Ligaments: bands of fibrous tissue connecting bone to cartilage; support and strengthen joints 1. Muscle fibers coated with fibrous connective tissue (fascia) that binds muscle to surrounding tissues 2. Attached to at least two bones; bone that moves is insertion bone, and bone that is stationary is origin bone 3. Muscle fibers contain myofibrils specialized for contraction; composed of protein myofilaments, containing actin and myosin B Physiology of muscle contraction 1. Basic principles of muscle contraction a. Contract only if stimulated; anything that prevents impulse conduction paralyzes muscles b. Skeletal muscles act in groups; classified as prime movers, synergists, or antagonists c. Contraction of skeletal muscle either shortens the muscle (producing movement) or increases muscle tension (tone) (1) Tonic contractions: produce muscle tone; there are no muscle movements (2) Isometric contractions: increase degree of muscle tone; daily isometric contractions gradually increase muscle strength; there are no muscle movements (3) Isotonic contractions: muscle is shortened, producing movement d. Treppe (staircase phenomenon): when a muscle contracts a few times, subsequent contractions are more powerful e. Shivering: rapid, repetitive, involuntary muscle contractions caused by hypothalamic temperature regulating center; most ATP energy is converted to heat, but a small part goes to muscle contraction; consumes large amounts of oxygen 2. Energy of muscle contraction a. Electrical energy flows along transverse intracellular tubules associated with sarcoplasmic reticulum b. Calcium ions released by electrical energy inactivate troponin, which blocks interaction between actin and myosin c. Myosin releases and uses energy from ATP to cause contraction d. Creatine phosphate replenishes ATP as needed; source of energy is glucose and fatty acids oxidized aerobically to carbon dioxide and water e. Anaerobic breakdown of glucose during prolonged and vigorous muscle contraction results in lactic acid buildup associated with fatigue and pain (lactic acidosis); this oxygen debt is reversed during rest or oxygen administration a. Axon terminal, containing synaptic vesicles, forms a junction with sarcolemma of muscle fiber; tiny synaptic cleft separates presynaptic membrane (axon) from postsynaptic membrane (sarcolemma) b. When a nerve impulse reaches an axon terminal, acetylcholine is released from synaptic vesicles into the synaptic cleft; when acetylcholine binds to receptor sites on the sarcolemma, a channel opens and sodium and potassium ions flow down their concentration gradients; the sarcolemma is depolarized, and electrical energy flows into the muscle fiber; cholinesterase inactivates acetylcholine to prevent static contraction a. Hypertrophy: physical enlargement of muscle resulting from increase in cellular components; muscle fibers do not divide to produce more fibers b. Atrophy: wasting of muscle resulting from a variety of factors (e.g., diminished cellular proliferation, death of cells, decreased activity, hormonal changes) c. Hyperplasia: proliferation of normal cells, increasing the volume of tissue 1. Provides supporting framework; protects viscera and brain 2. Bones serve as levers and joints as fulcrums 3. Hemopoiesis by red bone marrow: formation of all blood cells; some lymphocytes and monocytes are formed in lymphatic tissue B Skeleton: contains 206 bones C Joint: junction of two or more bones 1. Synarthrotic (fibrous): generally nonmovable; no joint cavity or capsule; bones held together by fibrous tissue (e.g., sutures) 2. Amphiarthrotic (cartilaginous): slightly movable; no joint cavity or capsule; bones held together by cartilage and ligaments (e.g., symphysis pubis) 3. Diarthrotic: freely movable; lined by layer of hyaline cartilage covering articular surfaces of joining bones; held together by fibrous capsule lined with synovial membrane and ligaments a. May be ball and socket (e.g., hip), hinge (e.g., elbow), condyloid (e.g., wrist), pivot, gliding, or saddle b. Movement depends on type of joint (1) Flexion: bending one bone on another, decreasing angle between adjacent bones (2) Extension: stretching one bone away from another, increasing angle between adjacent bones (3) Abduction: moving bone away from body’s midline (4) Adduction: moving bone toward body’s midline (5) Rotation: pivoting bone on its axis (6) Internal rotation: turning of a limb toward midline of body (7) External rotation: turning of a limb away from midline of body (8) Circumduction: circular movement of a limb (9) Supination: forearm movement turning palm forward or upward (10) Pronation: forearm movement turning palm backward or downward (11) Inversion: ankle movement turning sole of the foot inward (12) Eversion: ankle movement turning sole of the foot outward (13) Protraction: moving a part forward, such as lower jaw (14) Retraction: pulling a part back; opposite of protraction (15) Plantar flexion: pointing toes downward away from body 1. Male skeleton larger and heavier than female skeleton 2. Male pelvis deep and funnel shaped with narrow, pubic arch; female pelvis shallow, broad, and flaring with wider pubic arch 3. From infancy to adulthood: bones grow and their relative sizes change partly due to stimulation by somatotrophic hormone (e.g., torso becomes proportionately larger to head, pelvis becomes relatively larger, and legs proportionately longer) 4. From young adulthood to old age: bone margins and projections change gradually; marginal lipping and spurs occur, thereby restricting movement 5. Demineralization results in a reduction of bone mass per unit of volume (osteoporosis); mostly occurs in postmenopausal women; related to decreased hormone production, lack of exercise that stresses skeleton, and inadequate intake of calcium, magnesium, and vitamins A, C, and D
Nursing Care of Clients with Neuromusculoskeletal System Disorders
Overview
Review of Anatomy and Physiology
Structures and Functions of the Nervous System
Neurons
Brain
Cranial Nerves
Name and Number
Distribution
Function
Olfactory (I)
Nasal mucosa, high up along the septum especially
Sense of smell (sensory only)
Optic (II)
Retina of eyeball
Vision (sensory only)
Oculomotor (III)
Extrinsic muscles of eyeball, except superior oblique and external rectus; also intrinsic eye muscles (iris and ciliary)
Eye movements; constriction of pupil and bulging of lens, which together produce accommodation for near vision
Trochlear (IV), smallest cranial nerve
Superior oblique muscle of eye
Eye movements
Trigeminal (V) (or trifacial), largest cranial nerve
Sensory fibers to skin and mucosa of head and to teeth; muscles of mastication (sensory and motor fibers)
Sensation in head and face; chewing movements
Abducens (VI)
External rectus muscle of eye
Abduction of eye
Facial (VII)
Muscles of facial expression; taste buds of anterior two thirds of tongue; motor fibers to submaxillary and sublingual salivary glands
Facial expressions; taste; secretion of saliva
Acoustic (VIII) (vestibulocochlear)
Inner ear
Hearing and equilibrium (sensory only)
Glossopharyngeal (IX)
Posterior third of tongue; mucosa and muscles of pharynx; parotid gland; carotid sinus and body
Taste and other sensations of tongue; secretion of saliva; swallowing movements; function in reflex arcs for control of blood pressure and respiration
Vagus (X) (or pneumogastric)
Mucosa and muscles of pharynx, larynx, trachea, bronchi, esophagus; thoracic and abdominal viscera
Sensations and movements of organs supplied; for example, slows heart, increases peristalsis and gastric and pancreatic secretion; voice production
Spinal accessory (XI)
Certain neck and shoulder muscles (muscles of larynx, sternocleidomastoid, trapezius)
Shoulder movements; turns head; voice production; muscle sense
Hypoglossal (XII)
Tongue muscles
Tongue movements, as in talking; muscle sense
Spinal Cord
Spinal Nerves
Autonomic Nervous System
Nerve Impulse Conduction
Sense Organs
Structures and Functions of the Muscular System
Skeletal Muscles
Structures and Functions of the Skeletal System
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree