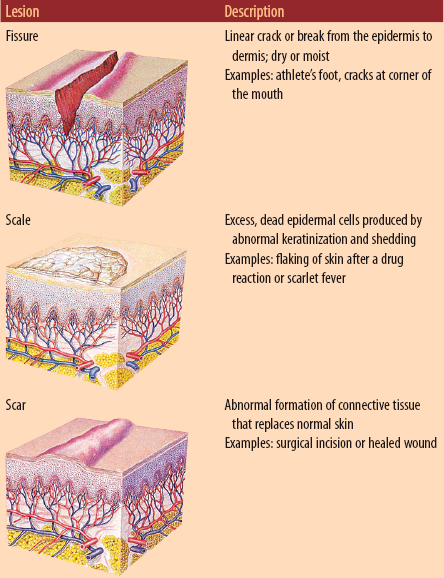
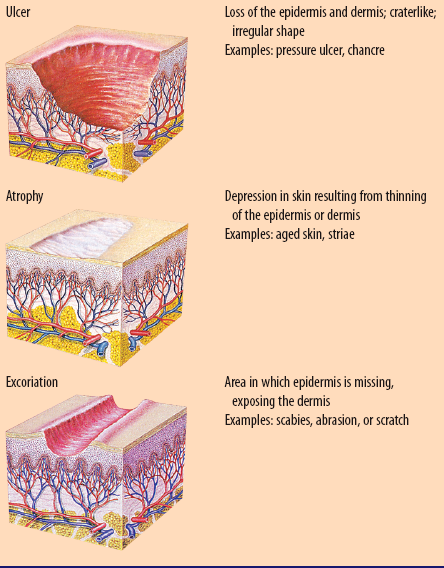
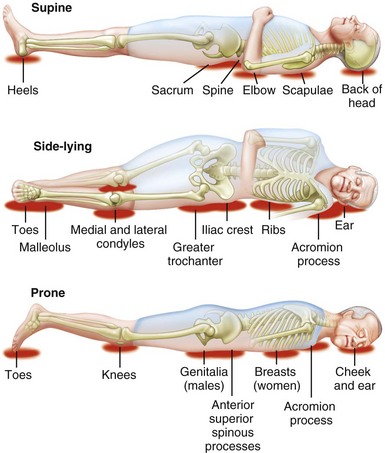
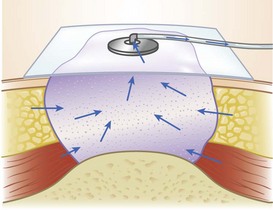
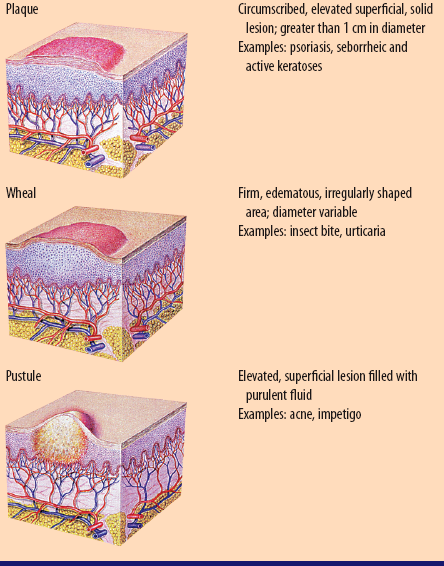
Chapter 10 A Prevents loss of body fluids B Protects deeper tissues from pathogenic organisms, noxious chemicals, and short-wavelength ultraviolet radiation C Helps regulate body temperature D Provides location for sensory reception of touch, pressure, temperature, pain, wetness, tickle, etc. E Assists in vitamin D synthesis 1. Contains no blood or lymphatic vessels; nourished by diffusion from underlying dermal papillae 2. Melanocytes produce melanin, which colors skin 3. Exceptional epidermal regions 4. Protects internal structures from harm and microorganisms 1. Vascular fabric of collagen and elastic fibers woven for strength and flexibility 2. Contains abundant touch receptors 3. Provides fingerprint pattern as unique arrangement of ridges projected to epidermal surface 4. Skin stretched beyond certain limits (e.g., during pregnancy) may rupture dermal collagen and elastic fibers; consequent scar tissue repair produces striae gravidarum 1. Eccrine: sweat glands opening in pores that secrete clear fluid 2. Apocrine: scent glands found in the axillary, mammary, and genital areas 3. Ceruminous: wax glands in external auditory canal 4. Sebaceous: small, saclike glands lacking innervation, usually forming close to hairs and opening into upper portion of hair follicle 5. Mammary: milk-secreting, alveolar glands; develop to full extent only during pregnancy 1. Vascular changes: initial vasoconstriction for hemostasis; vessel walls become lined with leukocytes (margination); vasodilation and increased vessel permeability (effects of histamine from mast cells, kinins, and prostaglandins); platelets clump and lymphatics become plugged with fibrin to wall off damaged area 2. Leukocytes leave vessels (diapedesis) and phagocytize foreign substances 3. Chronic inflammation: macrophages predominate and fibroblasts deposit collagen around each group of macrophages and foreign substances; stage of granuloma formation 1. Epithelialization: epithelial cells of epidermis begin to cover tissue defect 2. Deep in wound, fibroblasts synthesize collagen and ground substance; process begins about fourth or fifth day and continues for 2 to 4 weeks 3. Capillaries regenerate and tissue becomes red (granulation tissue) 1. Collagen fibers rearranged into stronger, more organized pattern 2. Scar remodels, gradually softens, and fades; hypertrophic scar or keloid forms if collagen synthesis exceeds breakdown 3. Contraction of wound margins begins about 5 days after injury; fibroblasts migrate into wound and assist in closing defect; may result in contractures that can be debilitating A Conduction: transfer of heat from one object to another by direct contact B Evaporation: water vapor released by skin (perspiration) cools body surface, which decreases body temperature C Radiation: transfer of heat from one object to another without actual contact D Convection: transfer of heat away from body by air movement 1. Act at the parasite’s nerve cell membrane to produce death of the organism 2. Destroy parasitic arthropods B Examples: permethrin (Nix), pyrethrum extract/piperonyl butoxide (RID), lindane (Kwell) C Major side effects: skin irritation (hypersensitivity); contact dermatitis (local irritation); hepatotoxicity and nephrotoxicity 1. Inspect skin, particularly scalp, for scabies and pediculosis before and after treatment; assess for skin irritation 2. Use gown, gloves, and hair covering to prevent spread of parasitic arthropods because scabies and pediculosis are highly contagious 3. Keep linen of infected client separate to prevent reinfection of client or family 4. Avoid drug contact with eyes and mucous membranes 5. Follow manufacturer’s directions on length of direct exposure to agent (e.g., leave on for 10 minutes and then wash off) and frequency of use, especially with children; explain lice can live up to 30 days or more; avoid use during pregnancy B Examples: mafenide (Sulfamylon); silver nitrate 0.5% solution; silver sulfADIAZINE (Silvadene) 1. Silver sulfADIAZINE: skin irritation; hemolysis in clients with glucose-6-phosphate dehydrogenase (G-6-PD) deficiency; may not be used in presence of renal failure 2. Mafenide: metabolic acidosis; burning sensation when first applied 3. Silver nitrate: electrolyte imbalance; brownish black discoloration of skin 1. Adhere to strict surgical asepsis; cleanse and ensure débridement before application 2. Apply prescribed medications 1. Reduce clinical findings of inflammation 2. Produce vasoconstriction, which decreases swelling and pruritus B Examples: triamcinolone (Kenalog, Triderm) C Major side effects: skin irritation (hypersensitivity); contact dermatitis (local irritation); skin atrophy; adrenal insufficiency if absorbed systemically (suppression of hypothalamic-pituitary-adrenal axis); fungal overgrowth 1. Inhibit keratinization and sebaceous gland function to improve cystic acne and reduce sebum excretion B Examples: isotretinoin (Claravis, Amnesteem, Sotret), vitamin A acid (Retin-A) C Major side effects: visual disturbances such as corneal opacities, decreased night vision (vitamin A toxicity—effect on visual rods); papilledema, headache (pseudotumor cerebri); hepatic dysfunction (hepatotoxicity); cheilitis (vitamin A toxicity); pruritus, skin fragility (dryness); hypertriglyceridemia (increased plasma triglycerides) (Table 10-1: Primary Skin Lesions) Table 10-1 From Lewis SL et al: Medical-surgical nursing: assessment and management of clinical problems, ed 8, St. Louis, 2011, Mosby. A Etiology and pathophysiology 1. Interruption of circulation when pressure on skin exceeds capillary pressure of 32 mm Hg for prolonged periods 2. Pressure compresses capillaries and microthrombi form to occlude blood flow; tissue becomes damaged due to hypoxia 3. Commonly occur over bony prominences: sacrum, greater trochanter, heels, scapulae, elbows, malleoli, occiput, ears, and ischial tuberosities (Figure 10-1: Common sites for pressure ulcers) a. Immobility—results in prolonged pressure b. Aging—decreased epidermal thickness, elasticity, and secretion by sebaceous glands c. Moisture (e.g., perspiration, urine)—causes skin maceration d. Imbalanced nutrition—loss of subcutaneous tissue reduces padding; inadequate protein intake leads to negative nitrogen balance, decreased muscle mass, and impaired wound healing e. Pyrexia—causes increased cellular demand for oxygen f. Inadequate tissue oxygenation—edema, anemia, and circulatory disturbances result in less oxygen delivered to tissues g. Incontinence—substances in urine and feces irritate skin i. Shearing force or friction—exerts excessive tension on skin j. Cognitive impairments—unaware of discomfort; inability to protect self k. Equipment—causes pressure, tension, or shearing forces on skin 5. Staging determined by depth and color (Figure 10-2: Staging of pressure ulcers) (1) Stage I: nonblanchable area of erythema; skin is intact; usually over bony prominence (2) Stage II: partial-thickness ulceration of epidermis and/or dermis; presents as abrasion, blister, or shallow crater; red/pink wound bed; without tissue sloughing; may be intact/open serum-filled blister (3) Stage III: full-thickness ulceration involving epidermis, dermis, and subcutaneous tissue; sloughing may be present; presents as deep crater with or without undermining; bone, tendon, or muscle is not exposed (4) Stage IV: extensive tissue damage involving full-thickness skin loss and damage to muscle, bone, and/or tendon; sloughing or eschar may be present on parts of wound bed; often includes undermining or tunneling 1. Subjective: pain; loss of sensation if there is sensory nerve damage 2. Objective: erythema; tissue damage (see Staging of pressure ulcers); exudate; pyrexia and leukocytosis if systemic infection is present 1. Elimination/minimization of pressure on ulcer through frequent repositioning and use of supportive devices (e.g., air-fluidized beds, low–air-loss beds, or kinetic beds) 2. Administration of protein supplements or total parenteral nutrition (TPN) to prevent negative nitrogen balance if client has serum albumin level less than 3.5 g, is anorexic, or is less than 80% of ideal body weight 3. Administration of vitamin and mineral supplements (particularly vitamin C and zinc) to promote wound healing 4. Débridement of necrotic tissue, which interferes with healing and promotes bacterial growth: mechanical irrigation; chemical débridement with enzyme preparations; surgical débridement; wet-to-damp dressings 5. Application of dressings to promote healing a. Moist gauze: maintains wound humidity, which promotes epithelial cell growth b. Polyurethane film: provides barrier to bacteria and external fluid; promotes moist environment; permits view of wound c. Hydrocolloid dressing: maintains wound humidity, liquefies necrotic debris, and provides a protective cushion d. Absorptive dressing: absorbs drainage e. Negative pressure wound therapy (NPWT); also known as vacuum-assisted wound closure (VAC): negative pressure applied to wound bed to remove exudate and facilitate angiogenesis (Figure 10-3: Wound VAC System)
Nursing Care of Clients with Integumentary System Disorders
Overview
Review of Anatomy and Physiology
Functions of the Integumentary System
Structures of the Integumentary System
Tissue Repair
Review of Physical Principles: Heat
![]() Related Pharmacology
Related Pharmacology
Pediculicides/Scabicides
Antiinfectives
Antipruritics
Antiinflammatory Agents
Dermal Agents
Major Disorders of the Integumentary System
Skin Lesions
Primary Lesions

Pressure Ulcers (Decubitus Ulcers)
Data Base
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



Nursing Care of Clients with Integumentary System Disorders
Get Clinical Tree app for offline access