Chapter 8 A Changes to food in alimentary canal occur so it can be absorbed and metabolized 1. Mechanical digestion: movements of alimentary tract that 2. Chemical digestion: series of hydrolytic processes dependent on specific enzymes and chemicals; an additional substance may be necessary to act as a catalyst to facilitate the process A Passage of small molecules from food sources through intestinal mucosa into blood or lymph B Accomplished mainly through movement of molecules against a concentration gradient because of energy (adenosine triphosphate [ATP]) expenditure (active transport) by intestinal cells; makes it possible for water and solutes to move through intestinal mucosa in a direction opposite that expected with osmosis and diffusion C Majority occurs in small intestine; most water is absorbed from large intestine A Definition: sum of all chemical reactions engaged in energy production and expenditure B Anabolism: synthesis of various compounds from simpler compounds C Catabolism: metabolic process in which complex substances are broken down into simple compounds; energy is liberated for use in movement, energy storage, and heat production 1. Glucose transport through cell membranes and phosphorylation a. Insulin promotes transport of glucose and amino acids through cell membranes b. Glucose phosphorylation: conversion of glucose to glucose 6-phosphate; insulin increases activity of glucokinase and promotes glucose phosphorylation, which is essential before glycogenesis and glucose catabolism 2. Glycogenesis: conversion of glucose to glycogen for storage in liver and muscle cells a. Glycogen is catabolized to glucose 6-phosphate in muscle cells b. Glycogen is converted to glucose in muscle cells; glucagon and epinephrine accelerate liver glycogenolysis a. Glycolysis: breakdown of one glucose molecule into two pyruvic acid molecules, with conversion of about 5% of energy stored in glucose to heat and ATP molecules b. Krebs citric acid cycle with the electron transport chain: breakdown of two pyruvic acid molecules into six carbon dioxide and six water molecules; Krebs cycle releases about 95% of energy stored in glucose 5. Gluconeogenesis: chemical reaction that converts protein or fat compounds into glucose; occurs in liver cells 6. Principles of carbohydrate metabolism a. Preferred energy fuel: most cells catabolize glucose first, sparing fats and proteins; when glucose supply becomes inadequate, most cells catabolize fats next; nerve cells require glucose, thus causing proteins to be sacrificed to provide amino acids needed to produce more glucose (gluconeogenesis); small amounts of glucose can be produced from glycerol portion of fats b. Glycogenesis: glucose in excess of 120 to 140 mg per 100 mL of blood brought to liver cells undergoes glycogenesis and is stored as glycogen c. Glycogenolysis: when blood glucose concentration decreases below midpoint of expected level, liver glycogenolysis accelerates and tends to raise blood glucose concentration back toward midpoint of expected level d. Gluconeogenesis: when blood glucose concentration decreases below expected level or when amount of glucose entering cells is inadequate, liver gluconeogenesis accelerates and raises blood glucose levels e. Glucose storage as fat: when blood insulin content is adequate, glucose in excess of amount used for catabolism and glycogenesis is converted to fat (Figure 8-1: Structures of the digestive system) A Size varies in people and according to degree of distention B Elongated pouch, with greater curve forming lower left border C In epigastric and left hypochondriac portions of abdominal cavity 1. Stomach wall cells secrete gastrin that stimulates flow of gastric juices 3. Parietal cells secrete hydrochloric acid and intrinsic factor A Size: approximately 2.5 cm (1 inch) in diameter; 6.1 m (29 feet) in length when relaxed 1. Duodenum: joins pylorus of stomach; C-shaped 3. Ileum: lower section; no clear boundary between jejunum and ileum C Functions: digestion and absorption; enzymes include sucrase, lactase, and maltase; cholecystokinin stimulates release of bile from gallbladder D Processes: mixing movements; peristalsis; secretion of water, ions, and mucus; receives secretions from the liver, gallbladder, and pancreas A Size: approximately 6.3 cm (2.5 inches) in diameter; 1.5 m (5 to 6 feet) long when relaxed C Functions: water and sodium ion absorption; temporary storage of fecal matter; defecation D Processes: weak mixing movements, peristalsis, and mass movements A Occupies most of right hypochondrium and part of epigastrium B Divided into thousands of lobules 2. Cystic duct: from gallbladder 3. Common bile duct: formed by union of hepatic and cystic ducts; drains bile into duodenum at sphincter of Oddi 1. Carbohydrate metabolism: converts glucose to glycogen by glycogenesis, converts glycogen to glucose by glycogenolysis, and forms glucose from proteins and fats by gluconeogenesis a. Ketogenesis: fatty acids are broken down into molecules of acetyl coenzyme A (acetyl-CoA) (beta oxygenation), which form ketone bodies (acetoacetic acid, acetone, beta-hydroxybutyric acid) c. Synthesis of triglycerides, phospholipids, cholesterol, and B complex factor choline a. Anabolism: synthesis of various blood proteins (e.g., prothrombin, fibrinogen, albumins, alpha and beta globulins, and clotting factors V, VII, IX, and X) b. Deamination: chemical reaction by which amino group splits off from amino acid to form ammonia and a keto acid c. Urea formation: liver converts most of ammonia formed by deamination to urea 4. Secretes bile, substance important for emulsifying fats before digestion and as a vehicle for excretion of cholesterol and bile pigments 5. Detoxifies various substances (e.g., drugs, hormones) 6. Vitamin metabolism: stores vitamins A, D, K, and B12; bile salts needed to absorb fat-soluble vitamins A, D, E, and K 7. Chief source is synthesized by bacteria in large intestine; vitamin K is a fat soluble vitamin that requires bile for its absorption 1. Fish-shaped, with body, head, and tail; extends from duodenal curve to spleen a. Pancreatic cells: secrete pancreatic juice via duct to duodenum; enzymes include trypsin, lipase, and amylase; stimulated by duodenal hormones secretin and pancreozymin and by parasympathetic impulses b. Islets of Langerhans: clusters of cells not connected with pancreatic ducts; composed of alpha and beta cells 1. Pancreatic juice composed of enzymes that help digest carbohydrates, proteins, and fats 2. Islet cells constitute endocrine gland a. Alpha cells secrete the hormone glucagon, which accelerates liver glycogenolysis and initiates gluconeogenesis; tends to increase blood glucose level b. Beta cells secrete insulin, which exerts profound influence on metabolism of carbohydrates, proteins, and fats (1) Accelerates active transport of glucose, along with potassium and phosphate ions, through cell membranes; decreases blood glucose level and increases glucose utilization by cells for either catabolism or anabolism (2) Stimulates production of liver cell glucokinase; promotes liver glycogenesis, which lowers blood glucose concentration (3) Inhibits liver cell phosphatase and therefore inhibits liver glycogenolysis (4) Accelerates rate of amino acid transfer into cells, promoting anabolism of proteins within cells (5) Accelerates rate of fatty acid transfer into cells, promotes fat anabolism (lipogenesis); inhibits fat catabolism A Carbohydrates (4 calories per 1 g): sugars (simple) and starches (complex); help provide basic fuel for energy (see Metabolism of Carbohydrates under Functions of the Gastrointestinal System); food sources: sugars, honey, fruit, milk, syrups, potatoes, rice, legumes, and products made with flour from grain (e.g., bread, cereal, pasta, crackers, cake, and cookies) B Proteins (4 calories per g): basically composed of amino acids; necessary for body growth, development, and healthy functioning; maintains nitrogen balance; food sources: meat, fish, poultry, dry beans, eggs, nuts, milk, and cheese C Fats (9 calories per 1 g): include neutral fats, oils, fatty acids, cholesterol, and phospholipids; contribute to cellular transport; dietary source of fuel and fuel reserve; vitamin absorption and transport; insulation and protection afforded by adipose tissue; food sources: animal fat, coconut and palm oil, dairy products, whole milk, vegetable oils, butter, margarine, mayonnaise, salad dressings, and baked goods and snacks that contain significant fat A Organic compounds needed to catalyze metabolic processes; essential for growth, development, and maintenance of body processes 1. Vitamin A: fat-soluble vitamin needed for night vision, healthy epithelium, skeletal and tooth development, and energy regulation a. Sources: carrots, cantaloupe, sweet potatoes, apricots, squash, broccoli, cabbage, spinach and collards, fortified milk products, egg yolk, liver, and kidney b. Deficiency: slow accommodation to dim light, sinus problems, sore throat, epithelial thickening of tissue over the eye 2. Vitamin D: fat-soluble vitamin that enhances bone mineralization promoting absorption of calcium, muscle contraction a. Sources: sunlight, cod liver oil, fortified milk, most dairy products b. Deficiency: rickets (soft, fragile bones; skeletal deformities), osteomalacia (softening of bone, causing flexible, brittle bones; skeletal deformities), tetany resulting from low serum calcium level (vitamin D necessary for calcium absorption) 3. Vitamin E: fat-soluble vitamin that is an antioxidant a. Sources: vegetable and peanut oils, whole grains, wheat germ, milk, eggs, meats, fish, and leafy vegetables 4. Vitamin K: fat-soluble vitamin associated with blood clotting and bone metabolism; majority is produced by intestinal bacteria a. Sources: liver; green, leafy vegetables (e.g., lettuce, spinach, cabbage, kale, broccoli, Brussels sprouts), cauliflower, asparagus b. Deficiency: prolonged antibiotic therapy and fat absorption problems, which contribute to prolonged blood clotting time 5. Vitamin C: water-soluble vitamin; antioxidant; associated with wound and fracture healing, adrenal gland function, iron absorption, and folic acid conversion a. Sources: citrus fruits, tomatoes, green and red peppers, white potatoes, cabbage, broccoli, kale, asparagus, chard, turnip greens, berries, melons, pineapple, and guavas b. Deficiency (scurvy): tender, sore, bleeding gums; loose teeth; small skin hemorrhages and bleeding around joints, stomach, and heart; ends of long bones soften; delayed wound healing 6. B-complex vitamins: B1 (thiamine), B2 (riboflavin), B3 (niacin), B6 (pyridoxine), folic acid, B12 (cyanocobalamin), B5 (pantothenic acid), and biotin; function as coenzymes a. Sources: enriched grains; each has its own source (e.g., B1—pork, wheat germ; B2—milk; B3—legumes; B6—organ meats; folic acid—orange juice, green leafy vegetables; biotin—egg yolks, liver) b. Deficiency: each has its own clinical findings; often seen in clients who drink an excessive amount of alcohol, experience weight loss, consume excessive sugar; may turn urine bright yellow A Inorganic substances that regulate body functions; help build body tissues; most important minerals: calcium, sodium, potassium, iron, iodine, and fluorine (see Table 3-4: Fluid/Electrolyte Imbalances: Etiology, Assessments, and Treatments) a. Needed for bone and tooth growth, coagulation, nerve conduction, and muscle contraction b. Sources: milk and dairy products, leafy green vegetables, whole grains, nuts, legumes, and seafood a. Major role in fluid balance, transmission of electrochemical impulses along nerve and muscle membrane b. Sources: table salt, processed foods, milk and milk products (for additional foods, see Low Sodium Diet under Review of Diets) a. Regulates fluid balance, conduction of nerve impulses, and muscle contraction, especially the heart b. Sources: oranges, bananas, dried apricots or peaches, cantaloupe, prune juice, baked potato with skins, sweet potato, raisins, pinto beans, winter squash, lima beans, broccoli a. Essential to hemoglobin and myoglobin formation, constituent of enzyme systems b. Sources: liver, lean meat, eggs, spinach, fortified cereals, dried beans a. Component of thyroid hormones, which help regulate metabolism, cell function and growth b. Sources: saltwater fish, shellfish and seaweed, table salt fortified with iodine 6. Fluoride (ionized form of fluorine) A MyPlate dietary guidelines: recommended by the U.S. Department of Agriculture, Center for Nutrition Policy and Promotion (Figure 8-2: MyPlate); includes food groups appropriate for a healthy diet Figure 8-2 MyPlate advocates building a healthy plate by making half of your plate fruits and vegetables and the other half grains and protein. Avoiding oversized portions, making half your grains whole grains, and drinking fat-free or low-fat (1%) milk are additional recommendations for a healthy diet. (From U.S. Department of Agriculture, Center for Nutrition Policy and Promotion; available at www.choosemyplate.gov.) 1. Minimizes stimulation of gastrointestinal (GI) tract; for clients with nausea and vomiting 2. Permitted: clear broth, bouillon, clear juices, plain gelatin, fruit-flavored water, ices, ginger ale, black coffee, tea 1. For client with GI disturbance or inability to tolerate solid or semisolid food; may follow clear liquid diet postoperatively 2. Permitted: all foods on clear liquid diet plus milk and items made with milk, such as cream soups, milk drinks, sherbet, ice cream, puddings, custard, yogurt 1. For clients who have difficulty chewing or swallowing 2. Permitted: all foods on clear and full liquid diets plus soft, refined cereals, pasta, rice, white bread and crackers, eggs, cheese, shredded or chopped meat, potatoes, cooked vegetables, soft cake, bread pudding, cooked fruits, and a few soft, ripe, plain fruits without membranes or skins E Regular diet: full, well-balanced diet of all foods as desired and tolerated; generally 2000 calories or as ordered by health care provider 1. Minimizes fecal volume and residue; used for severe diarrhea, partial bowel obstruction, and during acute episode of inflammation of bowel; can be used in progression to regular diet 2. Excluded: milk and milk products, food with seeds, nuts, grains, and raw or dried vegetables and fruits 1. Foods high in fiber resist digestion, causing bulky stool that increases peristalsis; increases water content of stool 2. Sources: whole grain foods, bran, root vegetables and their skins, prunes, nuts, fruits, beans H Restrictive diets: individually designed to meet specific needs of client 1. Low-sodium diet (e.g., 2 g sodium) b. Permitted: fresh fish, meat and poultry, fresh or frozen vegetables, pasta, unsalted butter, cooking oil, coffee, tea, lemonade, unflavored gelatin, jam, jelly, honey and maple syrup, unsalted nuts and popcorn, unsalted canned foods c. Excluded: salt, monosodium glutamate, soy sauce, milk, cheese, processed luncheon meats and bacon, snack foods (e.g., chips, pretzels, etc.), baked goods containing salt, bouillon, canned or packaged soup, rice/noodles, pickles, olives, sauerkraut, tomato juice, mustard, most bottled and canned drinks, canned vegetables unless low-sodium type, salad dressings, smoked or salted meat or fish, corned beef, powdered milk drinks, buttermilk, highly processed convenience foods, meat extracts, meat tenderizers, sugar substitutes containing sodium, and sauces such as catsup, tartar, horseradish, Worcestershire, and teriyaki a. To reduce saturated fat, reduce cholesterol, and prevent coronary heart disease b. Excluded: candy, ice cream, cake, cookies, and fried foods c. Strategies to reduce dietary fat: grill, bake, broil, or microwave food; eat less meat; eat leaner cuts of meat; remove fat from meat and skin/fat from poultry before cooking; use skim milk; use less butter or margarine; eat more fish, lima beans, and navy beans for protein 3. Calorie restriction: calories are restricted to reduce weight 4. Renal diet: low sodium, potassium, protein, and possibly fluid restriction; specific restrictions indicated by health care provider 5. Nonallergic diet: food causing the allergic response is eliminated from diet 6. Diabetic diet: recommended by the American Diabetic Association to control weight and nutritional intake; balances proteins, carbohydrates, and fats I Consistency modifications (e.g., mechanical soft): foods may be cut up, chopped, or pureed to make them easier for client to ingest A Refraction: total internal reflection in fiberoptics permits viewing of interior walls of stomach (gastroscopy) and intestines (colonoscopy) B X-rays: GI series and barium enemas allow visualization of soft tissues of upper and lower GI tract; barium salts coat inner walls of tract and absorb x-rays, outlining organ surfaces A Uniting oxygen with a substance results in oxidation B Uniting hydrogen with a substance results in reduction C Oxidation of nutrients such as glucose results in formation of high-energy ATP molecules and heat D Some forms of life (anaerobes) can use substances other than oxygen for cellular oxidation (e.g., Clostridium perfringens found in gangrenous tissue) A Fatty acids are important constituents of all lipids except sterols 1. Usually straight-chain carboxylic acids; three fatty acids and one glycerol molecule form a triglyceride 2. Saturated fatty acids: solid at room temperature; mainly animal fats 3. Unsaturated fatty acids: liquid at room temperature 4. Essential fatty acids: cannot be synthesized by body; must be taken in by diet B Cholesterol: sterol found in human and animal tissue; important component of cellular membranes; found in blood at 150 to 200 mg/mL; high cholesterol associated with increased intake of saturated fats and arterial atherosclerosis 1. Albumins: necessary for plasma colloid osmotic pressure (oncotic pressure), which helps control (through osmosis) flow of water between plasma and interstitial fluid; with starvation, decreased serum albumin level causes a decrease in plasma colloid osmotic pressure; results in edema as less fluid is drawn by osmosis into capillaries from interstitial spaces 2. Globulins: necessary to form antibodies (e.g., serum gamma globulin) 1. Lipoproteins: simple proteins combined with lipid substances a. Low-density lipoprotein cholesterol (LDL) b. High-density lipoprotein cholesterol (HDL) 2. Nucleoproteins: proteins complexed with nucleic acids; chromosomes are sometimes referred to as nucleoprotein structures a. Ribonucleic acid (RNA) and deoxyribonucleic acid (DNA) are nucleic acids b. RNA and DNA store and transmit genetic information from one generation to another 3. Metalloproteins: proteins containing metal ions (e.g., ferritin, the iron-transporting compound of plasma) 1. Escherichia coli: small, gram-negative bacilli; part of normal flora of large intestine; certain strains cause urinary tract infections and diarrhea 2. Clostridium difficile: anaerobic, spore-forming bacterial pathogen; produces toxins that affect bowel mucosa; major cause of agency acquired diarrhea 3. Salmonella: genus of gram-negative, rod-shaped bacteria; origin: raw foods of animal origin (e.g., poultry, eggs, dairy products, beef); also vegetables and fruit when irrigated or washed with contaminated water or packed with contaminated ice for transport 4. Shigella: gram-negative bacilli, similar to Salmonella; Shigella dysenteriae causes bacillary dysentery or shigellosis 1. Balantidium coli: ciliated protozoan; causes enteritis 2. Entamoeba histolytica: an amoeba; causes amebiasis (amoebic dysentery) 1. Nematodes (roundworms): include Necator americanus (hookworm), Ascaris lumbricoides, Enterobius vermicularis (pinworm), Trichuris trichiura (whipworm), all may be found in intestine 2. Cestodes (tapeworm): may be found in adult form in intestine; larval stage (hydatid) of some forms may develop and form cysts in liver, lungs, and kidneys 3. Trematodes (flukes): may be found in lungs, liver, and abdominal cavity 1. Diminish sensitivity of chemoreceptor trigger zone (CTZ) to irritants or decrease labyrinthine excitability 2. Alleviate nausea and vomiting 3. Prevent and control emesis and motion sickness 4. Available in oral, parenteral (intramuscular [IM], IV), rectal, and transdermal preparations 1. Centrally acting agents: ondansetron (Zofran); prochlorperazine (Compazine) 2. Agents for motion sickness control: dimenhyDRINATE (Dramamine); meclizine (Antivert, Bonine); promethazine (Phenergan) 3. Agents that promote gastric emptying: metoclopramide (Reglan) C Major side effects: drowsiness (central nervous system [CNS] depression); hypotension (vasodilation via central mechanism); dry mouth (decreased salivation from anticholinergic effect); blurred vision (pupillary dilation from anticholinergic effect); incoordination (extrapyramidal symptom resulting from dopamine antagonism) 1. Observe incidences and characteristics of vomitus, provide oral hygiene 2. Eliminate noxious substances from diet and environment 3. Administer before chemotherapy to limit nausea and vomiting 4. Offer sugar-free chewing gum or hard candy to promote salivation 5. Offer soothing fluids or ice chips in small amounts 6. Instruct to change positions slowly B Examples: amphetamine sulfate; dextroamphetamine sulfate (Dexedrine); phentermine (Adipex); diethylpropion (Tenuate); phendimetrazine C Major side effects: nausea, vomiting (irritation of gastric mucosa); constipation (delayed passage of stool in GI tract); tachycardia (sympathetic stimulation); CNS stimulation (sympathetic activation) 1. Provide protective coating on stomach lining and lower gastric acid pH; allow more rapid movement of stomach contents into duodenum 2. Neutralize gastric acid; effective in treatment of ulcers B Examples: aluminum hydroxide gel (Amphojel); aluminum and magnesium hydroxides (Maalox); famotidine (Pepcid); famotidine plus calcium carbonate and magnesium hydroxide (Pepcid Complete); ranitidine (Zantac, Peptic Relief) 1. Constipation (aluminum compounds: aluminum delays passage of stool in GI tract) 2. Diarrhea (magnesium compounds: magnesium stimulates peristalsis in GI tract) 3. Alkalosis (systemic antacids: absorption of alkaline compound into circulation) 4. Reduced absorption of calcium, iron, and most medications (increase in gastric pH) a. Prevention of overuse of antacids, which can result in rebound hyperacidity b. Need for continued supervision c. Dietary restrictions related to gastric distress d. Foods high in calcium and iron e. Need to take 1 hour before or 2 hours after other oral medications f. Caution client on sodium-restricted diet because many antacids contain sodium 2. Shake oral suspensions well before administration 3. Administer with small amount of water to ensure passage to stomach B Examples: atropine sulfate; dicyclomine (Bentyl); glycopyrrolate (Robinul) C Major side effects (all related to decreased parasympathetic stimulation) 1. Abdominal distention and constipation (decreased peristalsis) 2. Dry mouth (decreased salivation) 3. Urinary retention (decreased parasympathetic stimulation) 4. CNS disturbances: e.g., blurred vision, dizziness (direct CNS toxic effect) 1. Inhibit gastric acid secretion 2. Act at H2 receptors of stomach’s parietal cells to limit gastric secretion (H2 antagonists) 3. Inhibit hydrogen/potassium ATPase enzyme system to block acid production (proton pump inhibitors); used in conjunction with antibiotics to treat Helicobacter pylori infection 1. H2 antagonists: famotidine (Pepcid); ranitidine (Zantac); cimetidine (Tagamet) 2. Proton pump inhibitors: omeprazole (Prilosec); lansoprazole (Prevacid); esomeprazole (Nexium) 1. CNS disturbances (decreased metabolism of drug because of liver or kidney impairment) 2. Blood dyscrasias (decreased red blood cells [RBCs,] white blood cells [WBCs], platelet synthesis) 3. Skin rash (hypersensitivity) 4. Decrease in bone density with long-term use of acid suppression medications; esomeprazole magnesium (Nexium), lansoprazole (Prevacid), and omeprazole (Prilosec); similar but less risk with cimetidine (Tagamet) and famotidine (Pepcid) 1. Do not administer at same time as antacids; allow 1 hour before or 2 hours after other oral drugs 2. Administer oral preparations with meals 3. Assess for potentiation of oral anticoagulant effect 4. Instruct to follow prescription exactly 5. Do not administer for more than 8 weeks without medical supervision 1. Slow passage of stool through intestines 2. Promote formation of formed stools; alleviate diarrhea 1. Fluid adsorbents: decrease fluid content of stool: bismuth subsalicylate (Kaopectate, Pepto-Bismol) 2. Enteric bacteria replacements: enhance production of lactic acid from carbohydrates in intestinal lumen; acidity suppresses pathogenic bacterial overgrowth; Lactobacillus acidophilus (Bacid) and Lactobacillus bulgaricus (Lactinex) 3. Motility suppressants: decrease GI tract motility so more water is absorbed from large intestine; diphenoxylate/atropine (Lomotil); loperamide (Imodium) 1. Fluid adsorbents: GI disturbances (local effect); CNS disturbances (direct CNS toxic effect) 2. Enteric bacteria replacements: excessive flatulence (increased microbial gas production); abdominal cramps (increased microbial gas production) 3. Motility suppressants: constipation; urinary retention (decreased parasympathetic stimulation); tachycardia (vagolytic effect on cardiac conduction); dry mouth (decreased salivation from anticholinergic effect); sedation (CNS depression); paralytic ileus (decreased peristalsis); respiratory depression (depression of medullary respiratory center) 1. Intestinal lubricants: decrease dehydration of feces; lubricate intestinal tract; mineral oil, olive oil 2. Fecal softeners: lower surface tension of feces, allowing water and fats to penetrate; docusate calcium (Surfak), docusate sodium (Colace) 3. Bulk-forming laxatives: increase bulk in intestinal lumen, which stimulates propulsive movements by pressure on mucosal lining; methylcellulose (Citrucel), psyllium (Metamucil) 4. Colon irritants: stimulate peristalsis by reflexive response to irritation of intestinal lumen; bisacodyl (Dulcolax), senna (Senokot) 5. Saline cathartics: increase osmotic pressure within intestine, drawing fluid from blood and bowel wall, thus increasing bulk and stimulating peristalsis; effervescent sodium phosphate (Fleet Phospho-Soda), magnesium hydroxide (Milk of Magnesia), polyethylene glycol (MiraLax) 1. Laxative dependence with long-term use (loss of normal defecation mechanism) 2. GI disturbances (local effect) 3. Intestinal lubricants: inhibit absorption of fat-soluble vitamins A, D, E, K; may cause anal leaking of oil (accumulation of lubricant near rectal sphincter) 4. Saline cathartics: dehydration (fluid volume depletion resulting from hypertonic state in GI tract); hypernatremia (increased sodium absorption into circulation; shift of fluid from vasculature to intestinal lumen) 1. Instruct regarding overuse of cathartics and intestinal lubricants, increasing intake of fluids and dietary fiber, increasing activity level, and adhering to bowel-retraining program 2. Monitor bowel movements for consistency and frequency of stool 3. Administer at bedtime to promote defecation in morning 4. Encourage to develop healthy bowel habits 5. Intestinal lubricants: use peripad to protect clothing 6. Bulk-forming laxatives: mix thoroughly in 8 oz of fluid and follow with another 8 oz of fluid to prevent obstruction 1. Instillation of fluid into lower colon via stoma on abdominal wall to stimulate peristalsis and facilitate expulsion of feces 2. Cleansing colostomy stoma and collection of feces (stool consistency will depend on location of ostomy; colostomy of sigmoid colon will produce formed stools; transverse or ascending colostomy will produce less-formed stools) 1. Irrigate stoma at same time each day to approximate usual bowel habits; provide for uninterrupted bathroom use 2. Insert well-lubricated catheter tip (use a cone) into stoma approximately 7 to 8 cm in direction of remaining bowel 3. Hold irrigating container 12 to 18 inches above colostomy; temperature of irrigating solution should be 105° F (40.5° C) 4. Stop flow of fluid temporarily if cramping occurs 5. Provide privacy while waiting for fecal returns or encourage client to ambulate with collection bag in place to further stimulate peristalsis 6. Cleanse peristomal area with soap and water; apply a protective skin barrier 7. Apply colostomy bag with opening 8. Teach to control odor when necessary by placing commercially available deodorizer in colostomy bag A Definition: visualization of internal organs using hollow tube with lighted end: gastroscopy, stomach; esophagoscopy, esophagus; colonoscopy, entire large colon; sigmoidoscopy, sigmoid colon; proctoscopy, rectum; endoscopic retrograde cholangiopancreatography (ERCP), common bile and pancreatic ducts; capsule endoscopy, swallowed; virtual colonoscopy, series of computed tomography images of the intestine 1. Obtain informed consent for procedure 2. Teach ordered preprocedure protocol: length of time to limit/eliminate food/fluids, laxatives, enemas 3. If rectal examination is indicated, administer cleansing enemas before test 4. Place in knee-chest position for sigmoidoscopy/proctoscopy; left side-lying for colonoscopy 5. After procedure, observe for bleeding, changes in vital signs, or nausea 6. If throat is anesthetized (as for gastroscopy or esophagoscopy), check for return of gag reflex before offering oral fluids 8. Care before capsule endoscopy: instruct to fast for 12 hours before test; apply antenna patch and belt holding battery and data recorder; instruct to hold capsule under tongue for 1 minute as unit verifies that light source is functioning and then swallow capsule with 8 ounces of water 9. Care after ingestion of capsule endoscopic device: teach to notify health care provider immediately if experiencing dysphagia, abdominal or chest pain, nausea/vomiting, or fever (risk for obstruction); avoid strong electromagnetic field source until capsule is defecated; avoid strenuous activity, bending, or stooping during test; check that recorder is working every 15 minutes; return the device after capsule is expelled 1. Tap-water: introduction of water into colon to stimulate evacuation 2. Soapsuds: introduction of soapy water into colon to stimulate peristalsis by bowel irritation; contraindicated as preparation for endoscopic procedure because it may alter appearance of mucosa 3. Hypertonic: commercially prepared small-volume enema that works on principle of osmosis 4. Return flow (Harris flush or drip): repeated alternate introduction of water into colon and drainage of that water from colon through same tubing to facilitate exit of flatus 5. Instillation/retention: introduction of a liquid (usually mineral oil) into colon to facilitate fecal activity through lubricating effect 1. Provide privacy, place in left side-lying or Sims position 2. Obtain correct solution for the enema ordered 3. Lubricate tip of rectal catheter with water-soluble jelly 4. Insert catheter 3 to 4 inches into rectum 5. Allow solution to enter slowly; keep it no more than 12 inches above rectum; solution may be raised 15 to 18 inches for high cleansing enema; temporarily interrupt flow if cramping occurs 6. Allow ample time for expulsion of enema; encourage prolonged retention of instillation/retention enema A Definition: introduction of barium, an opaque medium, into upper GI tract via mouth (upper GI series) or into lower GI tract via rectum for purpose of x-ray visualization for pathologic changes 1. Prepare client for procedure a. Maintain nothing by mouth (NPO) for 8 to 10 hours before test b. Administer cathartics and/or enemas as ordered to evacuate bowel 2. Inspect stool after procedure for presence of barium 3. Administer enemas and/or cathartics as prescribed if stool does not return as expected 1. Nasogastric tube (NGT): tube placed through nose into stomach; has highest risk of aspiration of all types of feeding tubes 2. Intestinal tube: tube placed through nose into small intestine 3. Surgically placed feeding tubes a. Cervical esophagostomy: tube sutured directly into esophagus for clients who have had head and neck surgery b. Gastrostomy (GT): tube placed directly into stomach through abdominal wall and sutured in place; for clients who require tube feeding on long-term basis c. Jejunostomy: tube inserted directly into jejunum for clients with pathologic conditions of upper GI tract 4. Percutaneous endoscopic gastrostomy (PEG) and low-profile gastrostomy device (G-Button) 1. Verify placement of tube before feeding a. Confirm by radiography before initiating tube feedings; test aspirate for acid pH (pH of 1 to 4 confirms gastric placement although the pH can be as high as 6 if client is receiving drugs to reduce gastric acid); inject small amount of air into tube and, with stethoscope placed over epigastric area, listen for passage of air into stomach (less reliable than testing for gastric pH) b. Small-bore tube placement must be verified by radiographic examination 2. Aspirate contents of stomach before feeding to determine residual; follow health care provider’s orders or agency policy regarding holding feeding based on residual amounts; general guidelines: reinstill 300 mL to avoid electrolyte imbalance and call health care provider for orders; if residual is greater than half of last feeding, call health care provider for orders or follow agency policy; some agencies delay tube feedings for 1 hour if residual amount specified is aspirated when volume is assessed a. Position so that head of bed is elevated during feeding c. Introduce 30 mL of water to verify the patency of tube; tube should not be allowed to empty during feeding d. Slowly administer feeding to prevent regurgitation; administer at room or body temperature; observe and question client to determine tolerance e. Administer 30 mL of water to clear tube at completion of feeding f. Clamp tubing and clean equipment g. Place in sitting position for 1 hour after feeding; place infant in right side-lying position a. Place prescribed feeding in gavage bag and prime tubing to prevent excess air from entering stomach b. Check for residual as per agency policy to verify peristalsis c. Set rate of flow; rate of flow can be manually regulated by setting drops per minute or mechanically regulated by using infusion pump d. Keep head of bed elevated throughout feeding e. Verify placement of tube every 4 hours; generally done when adding additional fluid to feeding f. Flush tube intermittently with water to prevent occlusion of tube with feeding; change tubing per protocol g. Monitor for gastric distention and aspiration; gastric distention and subsequent aspiration are less frequent because smaller amounts of feeding are administered within a given period h. Discard unused fluid that has been in gavage administration bag at room temperature for longer than 4 hours 5. Care common for all clients receiving tube feedings a. Elevate head of bed; helps prevent aspiration; facilitates gastric emptying; promotes peristalsis b. Monitor for abdominal distention; changes in bowel sounds; assess for diarrhea caused by high osmolarity of feeding; stop tube feeding if nausea and/or vomiting occur or if bowel sounds are not audible; notify health care provider if client is not tolerating feedings d. When appropriate, encourage client to chew foods that will stimulate gastric secretions while providing psychologic comfort; chewed food may or may not be swallowed e. Provide special skin care; if client has gastrostomy tube sutured in place, skin may become irritated from gastrointestinal enzymes; if client has a nasogastric tube, skin may become excoriated at point of entry because of irritation f. Provide supplemental water to balance hypertonic formula if ordered by health care provider g. Care for site of tube entry; cleanse and use water-soluble jelly on nares for NGT; change dressing daily and clean with sterile saline if exudate is present for surgically implanted tubes and PEG tube 1. Peripheral parenteral nutrition (PPN): short-term use a. Administration of isotonic lipid and amino acid solutions through peripheral vein b. Amino acid content should not exceed 4%; dextrose content should not be greater than 10%; helps maintain positive nitrogen balance 2. Total parenteral nutrition (TPN): long-term use a. Administration of carbohydrates, amino acids, vitamins, and minerals via central vein because of high osmolality of solution b. High-osmolality solutions (25% dextrose) are administered in conjunction with 5% to 10% amino acids, electrolytes, minerals, and vitamins; helps maintain positive nitrogen balance c. Long-term home nutritional therapy may be delivered by atrial catheters (Hickman/Broviac or Groshong) that are surgically inserted a. Infusion of 10% to 20% fat emulsion that provides essential fatty acids b. Provides increased caloric intake to maintain positive nitrogen balance 4. Total nutrient admixture (TNA or 3 in 1) 1. Ensure placement of catheter by chest x-ray examination after insertion; assess for clinical manifestations of accidental pneumothorax, which can occur during insertion (e.g., shortness of breath, unilateral chest pain) 2. Regulate fluid infusion rate; intravenous pump should be used a. Rapid infusion may cause movement of fluid into intravascular compartment, causing dehydration, circulatory overload, and hyperglycemia b. Slow infusion may cause hypoglycemia because body adapts to the high osmolality by secreting more insulin; therefore, therapy is never terminated abruptly but is gradually discontinued; health care provider may order 10% glucose solution to maintain blood glucose level 3. Use filter for TPN; filters not used for lipids 4. Use surgical aseptic technique when changing tubing and applying new dressing 5. Record daily weights and monitor blood glucose levels frequently 6. Check laboratory reports daily, especially glucose, creatinine, blood urea nitrogen (BUN), and electrolytes; check serum lipids and liver function studies if lipids are administered 7. Monitor temperature every 4 hours (infection is most common complication of TPN); if a fever occurs, obtain cultures of blood, urine, and sputum to rule out other sources of infection
Nursing Care of Clients with Gastrointestinal System Disorders
Overview
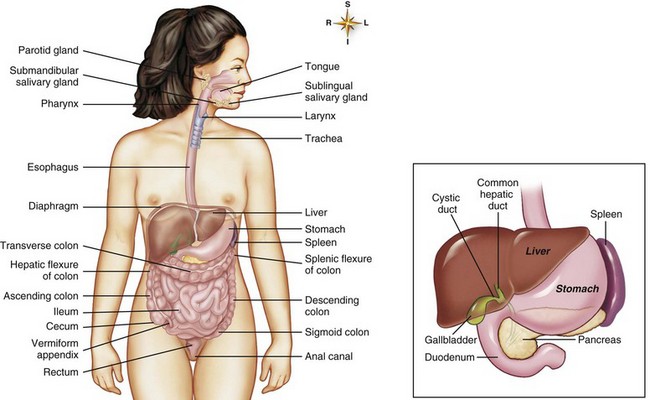
Review of Anatomy and Physiology
Functions of the Gastrointestinal System
Digestion
Absorption
Metabolism
Structures of the Gastrointestinal System
Mouth (Buccal Cavity)
Stomach
Small Intestine
Large Intestine
Liver
Pancreas
Review of Nutrients
Sources of Energy
Vitamins
Minerals
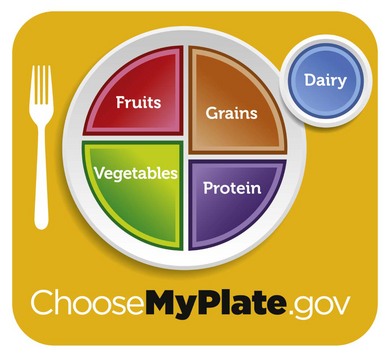
Review of Diets
Review of Physical Principles
Light
Review of Chemical Principles
Oxidation and Reduction
Types of Compounds
Lipids
Proteins
Review of Microorganisms
![]() Related Pharmacology
Related Pharmacology
Antiemetics
Anorexiants
Antacids
Anticholinergics
Antisecretory Agents
Antidiarrheals
Cathartics/Laxatives
Pancreatic Enzymes
Related Procedures
Colostomy Irrigation
 inch away from stoma; use gauze dressing if colostomy is well regulated
inch away from stoma; use gauze dressing if colostomy is well regulated
Endoscopy
Enemas
Gastrointestinal Series
Gavage (Tube Feeding)
Parenteral Replacement Therapy
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree