Chapter 9 (Figure 9-1: Principal endocrine glands) A Overlies thyroid cartilage below larynx B Thyroid hormones: accelerate cellular reactions in most body cells 1. Thyroxine: stimulates metabolic rate; essential for physical and mental development 2. Triiodothyronine: inhibits anterior pituitary secretion of thyroid-stimulating hormone 3. Calcitonin (thyrocalcitonin): decreases loss of calcium from bone; promotes hypocalcemia; action opposite that of parathormone A Small glands (2 to 12) embedded in posterior part of thyroid B Parathyroid hormone (parathormone) 1. Increases blood calcium concentration a. Breakdown of bone with release of calcium into blood (requires active form of vitamin D) b. Calcium absorption from intestine into blood 2. Decreases blood phosphate concentration by slowing its reabsorption from kidneys, thereby decreasing calcium loss in urine (See Structures of the Male Reproductive System in Chapter 12 and Female Reproductive System in Chapter 23) A Two closely associated structures, adrenal medulla and adrenal cortex, positioned at each kidney’s superior border 1. Adrenal medulla: produces two catecholamines, epinephrine and norepinephrine a. Stimulate liver and skeletal muscle to break down glycogen to produce glucose b. Increase oxygen use and carbon dioxide production c. Increase blood concentration of free fatty acids through stimulation of lipolysis in adipose tissue d. Cause constriction of most blood vessels of body, thus increasing total peripheral resistance and arterial pressure to shunt blood to vital organs e. Increase heart rate and force of contraction, thus increasing cardiac output f. Inhibit contractions of gastrointestinal and uterine smooth muscle g. Epinephrine significantly dilates bronchial smooth muscle 2. Adrenal cortex: secretes the mineralocorticoid aldosterone and the glucocorticoids cortisol and corticosterone (1) Markedly accelerates sodium and water reabsorption by kidney tubules (2) Markedly accelerates potassium excretion by kidney tubules (3) Secretion increases as sodium ions decrease or potassium ions increase b. Cortisol and corticosterone (1) Accelerate mobilization and catabolism of tissue protein and fats (2) Accelerate liver gluconeogenesis (hyperglycemic effect) (3) Decrease antibody formation (immunosuppressive, antiallergic effect) (4) Slow proliferation of fibroblasts characteristic of inflammation (antiinflammatory effect) (5) Decrease adrenocorticotropic hormone (ACTH) secretion (6) Mildly accelerate sodium and water reabsorption and potassium excretion by kidney tubules A Retroperitoneal in abdominal cavity B Pancreatic hormones: regulate glucose and protein homeostasis through action of insulin and glucagon 1. Insulin: secreted by beta cells of islets of Langerhans a. Promotes cellular uptake of glucose b. Stimulates intracellular macromolecular synthesis, such as glycogen synthesis (glyconeogenesis), fat synthesis (lipogenesis), and protein synthesis c. Stimulates cellular uptake of sodium and potassium (latter is significant in treatment of diabetic coma with insulin) 2. Glucagon: secreted by alpha cells of islets of Langerhans a. Induces liver glycogenolysis; antagonizes glycogen synthesis stimulated by insulin b. Inhibits hepatic protein synthesis, which makes amino acids available for gluconeogenesis and increases urea production c. Stimulates hepatic ketogenesis and release of glycerol and fatty acids from adipose tissue when cellular glucose level falls A Located in cranial cavity in sella turcica of sphenoid bone; near optic chiasm B Anterior lobe (adenohypophysis) and posterior lobe (neurohypophysis) 1. Hormones secreted by anterior lobe b. Thyroid-stimulating hormone (TSH): stimulates synthesis and secretion of thyroid hormones (1) Stimulates growth of adrenal cortex (2) Stimulates secretion of glucocorticoids; slightly stimulates mineralocorticoid secretion d. Follicle-stimulating hormone (FSH) (1) Stimulates primary graafian follicle to grow and develop (2) Stimulates follicle cells to secrete estrogen (3) Stimulates development of seminiferous tubules and spermatogenesis (1) Stimulates maturation of follicle and ovum; required for ovulation (2) Forms corpus luteum in ruptured follicle following ovulation; stimulates corpus luteum to secrete progesterone (3) In males, LH is called interstitial cell–stimulating hormone (ICSH); stimulates testes to secrete testosterone 2. Hormones secreted by posterior lobe a. Antidiuretic hormone (ADH, vasopressin) (1) Stimulates contractions by pregnant uterus (2) Stimulates milk ejection from alveoli of lactating breasts into ducts c. Melanocyte-stimulating hormone (MSH): stimulates synthesis and dispersion of melanin in skin, causing darkening 1. Used to treat diabetes mellitus 2. Classified into two types: insulin for parenteral use and oral antidiabetics a. Acts to facilitate transport of glucose and amino acids across cell membrane; promotes glycogenesis and protein synthesis b. Available in three forms: human, pork and beef (no longer available in U.S. because of risk of cow tissue spreading specific infections); human insulin is least antigenic; administered parenterally; brands or forms should not be substituted without medical supervision; nonhuman insulin rarely used since recombinant forms became available c. Insulin administered by syringe, pen, pump, or IV d. Available in rapid-acting, short-acting, intermediate-acting, and long-acting forms; rapid- or short-acting insulin may be premixed with intermediate-acting insulin 1. Insulin (Table 9-1: Types of Insulin) 2. Oral antidiabetics (hypoglycemics) a. Sulfonylureas: stimulate beta cells to produce insulin; second-generation sulfonylureas: glipiZIDE (Glucotrol), glyBURIDE, glimepiride (Amaryl) b. Biguanides: reduce the rate of endogenous glucose production by liver; increase the use of glucose by muscle and fat cells; metformin (Glucophage) c. Thiazolidinediones: improve insulin sensitivity, thus improving peripheral glucose uptake; rosiglitazone (Avandia), pioglitazone (Actos) d. Meglitinides: stimulate quick release of insulin by beta cells; repaglinide (Prandin), nateglinide (Starlix) e. Alpha-glucosidase inhibitors: block digestion of ingested carbohydrates and slow absorption of glucose; acarbose (Precose), miglitol (Glyset) f. Dipeptidyl peptidase 4 (DPP-4) inhibitor: prevents breakdown of glucagon-like peptide-1 (GLP-1) which reduces blood glucose levels in the body; sitagliptin (Januvia), saxagliptin (Onglyza) g. Synthetic analog of human amylin: decreases gastric emptying; pramlintide (Symlin) h. Incretin mimetic: stimulates insulin production in type 2 diabetes; exenatide (Byetta), liraglutide (Victoza); injectable medications for type 2 diabetes i. Combination: glyBURIDE/metformin (Glucovance); sitagliptin/metformin (Janumet); pioglitazone/metformin (Actoplus Met) 1. Parenteral insulin: hypoglycemia (e.g., irritability, tachycardia, hunger, moist skin, tremor, headache, confusion, seizures); lipodystrophy (incidence decreased dramatically since advent of human recombinant insulin) 2. Inhalation insulin: cough, dry mouth, chest discomfort 3. Oral antidiabetics: hypoglycemia; skin rash, allergic reactions, pruritus (hypersensitivity); jaundice (hepatic alterations); thrombocytopenia; lactic acidosis; vitamin B12 deficiency 1. Assess clients for clinical findings of hypoglycemia and side effects of medications a. Use proper medication administration procedure b. Adhere to dietary program, including snacks c. Avoid alcohol, especially when taking metformin (Glucophage) d. Perform self-monitoring of blood glucose (SMBG) levels f. Be prepared for hypoglycemic incidents; administer rapid-acting glucose (e.g., glucose gel or tablets) followed by complex carbohydrate and protein (e.g., cheese and crackers) to stabilize blood glucose level g. Ensure regular laboratory testing (e.g., blood glucose, glycosylated hemoglobin [glycohemoglobin, Hb A1c], liver enzymes) a. Administer all insulin subcutaneously because insulin is destroyed by gastric juices if taken by mouth; rapid-acting insulins can be used in continuous subcutaneous (Sub-Q) insulin infusion devices b. Use regular insulin or glulisine (Apidra) for IV administration c. If premixed insulin is not prescribed and two forms are to be mixed, draw up rapid- or short-acting insulin first so as not to accidentally dilute the vial with NPH insulin; peakless basal insulin cannot be mixed with other insulins because it causes precipitation d. Rotation of sites not necessary with recombinant insulin; abdomen is preferred site because absorption is not influenced by exercise e. Dosage adjustment is necessary when taking nothing by mouth (NPO) and when ill 4. Offer emotional support; therapy is lifelong 5. Metformin (Glucophage): withhold drug before and 48 hours after diagnostic studies requiring iodinated contrast media; increased risk of hypoglycemia when given concurrently with allopurinol (Zyloprim) 6. Instruct to prevent complications of hyperglycemia with frequent glucose monitoring and multiple daily injections of insulin as needed 1. Regulate metabolic rate of body cells; aid in growth and development of bones and teeth; affect protein, fat, and carbohydrate metabolism 2. Replace thyroid hormone when there is a reduction in or absence of thyroid gland function B Examples: levothyroxine (Synthroid) is drug of choice; liothyronine (Cytomel); liotrix (Thyrolar) C Major side effects: increased metabolism (increased serum triiodothyronine [T3], thyroxine [T4]); hyperactivity (increased metabolic rate); cardiac stimulation (increased cardiac metabolism) a. Report occurrence of side effects immediately b. Take medication as scheduled at same time daily; do not stop abruptly c. Take pulse rate; notify health care provider if greater than 100 beats/min 2. Assess for potentiation of anticoagulant effect 3. Offer emotional support; therapy usually is lifelong 1. Interfere with synthesis and release of thyroid hormone; inhibit oxidation of iodides to prevent their combination with tyrosine in formation of thyroxine B Examples: methimazole (Tapazole); propylthiouracil (PTU) C Antithyroid medications such as iodine (e.g., potassium iodide, SSKI) to reduce vascularity of thyroid gland D Major side effects: agranulocytosis (decreased white blood cells [WBCs]); skin disturbances (hypersensitivity); nausea, vomiting (irritation of gastric mucosa); decreased metabolism (decreased production of serum T3, T4); iodine—bitter taste, stains teeth (local oral effect on mucosa and teeth) 1. Interfere with release of factors important in producing inflammatory and immune responses (immunosuppression) 2. Remove fluid accumulation from brain, thereby decreasing cerebral edema 3. Increase glucose and fat formation and promote protein breakdown 4. Used for hormonal replacement therapy 5. Available in oral, parenteral (intramuscular [IM], IV), inhalation, intraarticular, and topical (including ophthalmic) preparations 1. Cushingoid clinical findings (increased glucocorticoid activity causing facial edema, fluid retention) 2. Hypertension (sodium and water retention) 3. Hyperglycemia (increased carbohydrate catabolism; gluconeogenesis) 4. Mood changes (central nervous system [CNS] effect) 5. Gastrointestinal (GI) irritation and ulcer formation (local GI effect) 7. Hypokalemia (potassium excretion) 8. Decreased wound healing; leukopenia 10. Derivatives with 17-ketosteroid properties: masculinization in females 1. Administer oral preparations with food, milk, or antacid 2. Monitor weight, blood pressure, and serum electrolytes 4. Monitor blood glucose level in people with diabetes a. Avoid exposure to infections; notify health care provider if fever or sore throat occurs; avoid immunizations during therapy b. Avoid using salt; encourage foods high in potassium c. Take medications only as directed, and explain why; avoid missing, changing, or withdrawing drug suddenly d. Avoid nonsteroidal antiinflammatory drugs (NSAIDs) and over-the-counter (OTC) medications 6. Withdraw drug therapy gradually to permit adrenal recovery 1. Promotes water reabsorption by distal renal tubules and causes vasoconstriction and increased muscle tone of bladder, GI tract, uterus, and blood vessels B Example: desmopressin (DDAVP) 1. Transient headache, drowsiness, listlessness (CNS effect) 2. Nausea, heartburn, mild abdominal cramps (GI irritation) 3. Nasal irritation, congestion, rhinitis 4. Shortness of breath, facial flushing, pain and swelling at injection site A Etiology and pathophysiology 1. Excessive concentration of pituitary hormones (e.g., GH, ACTH, PRL) in the blood, glandular over activity, an adenoma, or changes in the anterior lobe of the pituitary gland 2. Classification of GH overproduction a. Gigantism: generalized increase in size, especially in children; involves long bones b. Acromegaly: occurs after epiphyseal closing, with subsequent enlargement of cartilage, bone, and soft tissues of body 1. Subjective: headaches, depression, weakness a. Increased soft tissue and bone thickness b. Facial features become coarse and heavy, with enlargement of lower jaw, lips, and tongue e. X-ray examination of long bones, skull (sella turcica area), and jaw demonstrates change in structure g. Clinical findings of increased intracranial pressure (e.g., vomiting, papilledema, focal neurologic deficits) 1. Changes in energy level, sexual function, and menstrual patterns; signs of increased intracranial pressure 2. Face, hands, and feet for thickening, enlargement; changes in the size of hat, gloves, rings, or shoes 4. Presence of hypogonadism as a result of hyperprolactinemia 5. Reaction to changes in physical appearance and sexual function 1. Help to accept altered body image that is irreversible 2. Assist family to understand what client is experiencing 3. Help to recognize that the need for medical supervision will be life-long 4. Help to understand the basis for the change in sexual functioning 5. Encourage to express feelings 6. Teach self-care after a hypophysectomy 7. Provide care after intracranial surgery a. Perform neurologic assessments; monitor for increased intracranial pressure b. Monitor I&O and daily weight to identify complication of diabetes insipidus c. Assess clear nasal drainage for glucose to determine presence of cerebrospinal fluid (CSF); CSF will test positive for glucose d. Encourage deep breathing, but not coughing e. Institute measures to prevent constipation because straining increases intracranial pressure A Etiology and pathophysiology 1. Deficiency of one or more anterior pituitary hormones 2. Total absence of pituitary hormones referred to as panhypopituitarism (Simmonds disease) 3. Occurs with destruction of anterior lobe of pituitary by trauma, tumor, or hemorrhage B Clinical findings (vary with target organs affected)
Nursing Care of Clients with Endocrine System Disorders
Overview
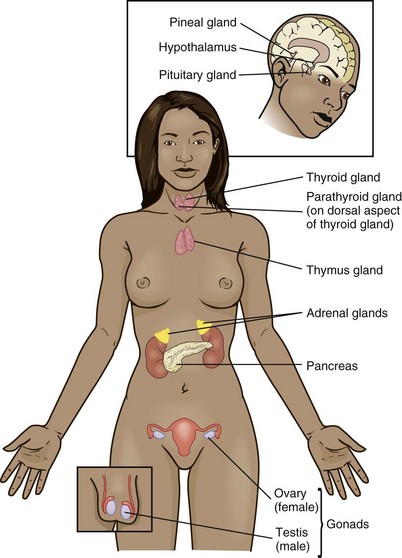
Review of Anatomy and Physiology
Structures of the Endocrine System
Thyroid Gland
Parathyroid Gland
Testes and Ovaries
Adrenal Glands
Pancreas
Pituitary Gland
![]() Related Pharmacology
Related Pharmacology
Antidiabetic Agents
Thyroid Enhancers
Thyroid Inhibitors
Adrenocorticoids
Antidiuretic Hormone
Major Disorders of the Endocrine System
Hyperpituitarism
Data Base
Nursing Care of Clients with Hyperpituitarism
Assessment/Analysis
Planning/Implementation
Hypopituitarism
Data Base
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree