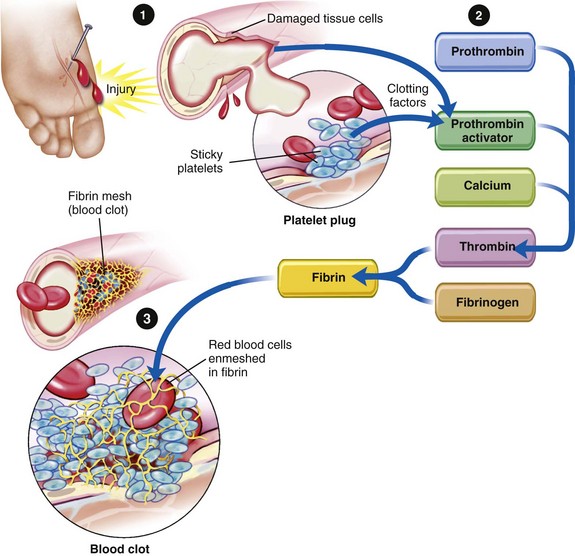
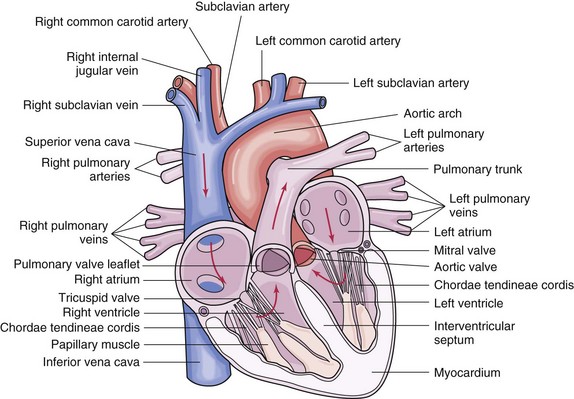
Chapter 6 A Volume: males: 5 to 6 L; females: 4.5 to 5.5 L B Viscosity: about 5.5 times as viscous as pure water; reflected by hematocrit (percentage of blood volume that is made up of red blood cells [RBCs]) 1. Location: red marrow of vertebrae, sternum, ribs, iliac crests, clavicles, scapulae, and skull 2. Pluripotential stem cell differentiates into myeloid and lymphoid stem cells a. Water: 3 L in average adult; 90% of plasma b. Ions: see Fluid, Electrolyte, and Acid-Base Balance in Chapter 3 c. Albumin (major plasma protein) d. Glucose: prime oxidative metabolite (1) Shape: pliable biconcave disk that maximizes surface area proportional to volume for ease of diffusion of gases (2) Number: males: 4.5 to 6.2 × 106/mm3; females: 4.0 to 5.5 × 106/mm3 (3) Formation (erythropoiesis): liver and kidneys secrete proteins that help form erythropoietin, which stimulates erythrocyte production by red bone marrow (4) Principal component is hemoglobin; functions to bind oxygen through iron in heme and carbon dioxide through globulin portion; can carry both simultaneously (5) Erythrocytes live for about 120 days; old or deteriorated ones are removed by reticuloendothelial cells of liver, spleen, and bone marrow; heme is converted to bilirubin, which is excreted from liver as part of bile b. Leukocytes white blood cells [WBCs] (a) Granulocytes (polymorphonuclear): neutrophils, eosinophils, and basophils (b) Agranulocytes (mononuclear): monocytes that become macrophages in tissue spaces and lymphocytes (a) Phagocytosis of bacteria by neutrophils and macrophages; phagocytosis of antigen-antibody complexes by eosinophils (b) Antibody synthesis: B lymphocytes become plasma cells, which produce most circulatory antibodies (c) Destruction of transplanted tissues and cancer cells by T lymphocytes, which form in lymphoid tissue and mature in the thymus (3) Leukocytes live for a few hours or days; some T lymphocytes live for many years and provide long-term immunity 1. Four blood types: A, B, AB, and O; type indicates antigens on or in the RBC membrane (e.g., type A blood has A antigens; type O blood has no antigens) 2. Blood can be either Rh-positive or Rh-negative; usually blood does not contain anti-Rh antibodies. However, Rh-negative blood will contain anti-Rh antibodies if the individual has been transfused with Rh-positive blood or has carried an Rh-positive fetus without treatment; Rh-positive blood never contains anti-Rh antibodies; people with Rh-positive blood can receive blood from an Rh-negative donor; people with Rh-negative blood cannot receive blood from an Rh-positive donor 3. Plasma: usually contains no antibodies against antigens present on its own RBCs, but does contain antibodies against other A or B antigens not present on its RBCs 4. The potential danger in transfusing blood is that the donor’s blood may be agglutinated (clumped) by the recipient’s antibodies F Hemostasis: process to arrest blood loss (Figure 6-1: Blood clotting mechanism) 2. Aggregation of platelets: adhere to damaged blood vessel walls, forming plugs 3. Blood coagulation (clotting): blood becomes gel as soluble fibrinogen is converted to insoluble fibrin a. Extrinsic clotting mechanism: trigger is blood contacting damaged tissue b. Intrinsic clotting mechanism: trigger is release of chemicals (platelet factors such as thromboplastin) from platelets aggregated at site of injury c. Liver cells synthesize prothrombin, fibrinogen, and other clotting factors; adequate amounts of vitamin K must be present in blood for liver to produce prothrombin; calcium acts as a catalyst to convert prothrombin to thrombin d. Prothrombin is converted to thrombin, which converts fibrinogen to fibrin; fibrin is an insoluble protein formed from soluble protein fibrinogen in the presence of thrombin; fibrin appears as a tangled mass of threads in which blood cells become enmeshed e. When new endothelial cells form, the fibrin clot is destroyed by plasmin, which is formed from plasminogen (Figure 6-2: Structures of the heart and course of blood through chambers) 1. Pericardium (protective covering): parietal and visceral (epicardium) layers create a protective sac containing a small amount of lubricating fluid that reduces friction 2. Myocardium (cardiac muscle cells): rhythmic contraction (systole) and relaxation (diastole) pumps blood through systemic and pulmonary circulations 3. Endocardium (endothelial inner lining of inner chambers and valves) 1. Right atrium: receives deoxygenated blood from systemic circulation via the vena cava 2. Right ventricle: pumps deoxygenated blood to the pulmonary circulation via the pulmonary artery 3. Left atrium: receives oxygenated blood from the pulmonary circulation via the pulmonary vein 4. Left ventricle: pumps oxygenated blood to the systemic circulation via the aorta 1. Atrioventricular valves between atria and ventricles: tricuspid on right, mitral (bicuspid) on left; valves consist of three parts: flaps or cusps, chordae tendineae, papillary muscles; closure during early systole prevents backward flow of blood (regurgitation) into atrium and causes first heart sound (S1) 2. Semilunar valves: pulmonic valve between right ventricle and pulmonary arteries, and aortic valve between left ventricle and aorta; closure at end of systole prevents backward flow of blood into ventricles and causes second heart sound (S2) 3. Auscultation for S1, S2, murmurs caused by regurgitation of blood through valves, and snaps/clicks caused by stenosis of valves a. Apical pulse or mitral valve: located at fifth intercostal space near left midclavicular line b. Aortic valve: located at second intercostal space on right of sternum c. Pulmonic valve: located at second intercostal space on left of sternum d. Tricuspid valve: located at fifth intercostal space on left of sternum D Blood supply to myocardium (heart muscle) 1. Left coronary artery branches from the aorta and divides to form left anterior descending artery and circumflex artery, supplying blood to anterior and inferior surfaces of left ventricle 2. Right coronary artery branches from the aorta, mainly supplying right side of heart, but also inferior surface of left ventricle 3. Greatest flow of blood into myocardium occurs when the heart relaxes (diastole), as a result of decreased arterial compression; an increased heart rate shortens diastole, leading to decreased time for myocardial perfusion 4. Relatively few anastomoses exist between the larger branches of the coronary arteries (poor collateral circulation); if one of these vessels becomes occluded suddenly, little or no blood can reach myocardial cells supplied by that vessel; however, collateral circulation can develop slowly over time E Conduction system of heart: cardiac muscle cells have ability to generate impulses that cause contractions (automaticity) 1. Sinoatrial (SA) node: located in right atrial wall; referred to as pacemaker of the heart because it inherently generates impulses at the rate of 60 to 100/min 2. Atrioventricular (AV) node: located in base of the right atrium; capable of generating 40 to 60 impulses per minute if SA node is nonfunctional 3. Bundle of His: lies at the intraventricular septum and bifurcates into the right and left bundle branches; disruption in conduction here is called a bundle branch block 4. Purkinje fibers: extend from the right and left bundle branches, spreading electrical impulses throughout the ventricular walls 5. Usually a nerve impulse begins at the SA node and spreads through both atria to the AV node; after a short delay it is conducted to the bundle of His, bundle branches, and finally Purkinje fibers; the ventricles can generate 20 to 40 impulses per minute if both SA and AV nodes fail as pacemakers F Cardiac output (CO) (CO = heart rate × stroke volume): volume of blood pumped per minute by the ventricles; average for adult at rest is approximately 5 L/min 1. Preload: extent to which left ventricle stretches at end of diastole as a result of left ventricular end-diastolic volume; Frank-Starling law states when the heart is stretched by an increased returning volume of blood, it contracts more strongly, resulting in an increased stroke volume; subject to physiologic limitations 2. Afterload: arterial resistance that heart must overcome to eject contents of the left ventricle during systole; an increased afterload caused by systemic vasoconstriction will decrease stroke volume unless contractility is increased 3. Contractility: force of cardiac muscle contraction; increased by sympathetic nervous system, leading to increased stroke volume; decreased by parasympathetic nervous system; influences ejection fraction (percent of blood volume at the end of diastole that is ejected by ventricular contraction) 4. Heart rate: cardiac contractions per minute; increased by sympathetic nervous system and decreased by parasympathetic nervous system; bradycardia is a rate less than 60 beats/min; tachycardia is a rate greater than 100 beats/min 1. Carry blood away from heart (all arteries except pulmonary artery carry oxygenated blood) 2. Branch into smaller and smaller vessels called arterioles, which branch into microscopic capillaries 3. Structure: lining (tunica intima) of endothelium; middle coat (tunica media) of smooth muscle, elastic, and fibrous tissues, which permits constriction and dilation; outer coat (tunica adventitia or externa) of fibrous tissue; this firmness allows arteries to remain open instead of collapsing when cut 4. Peripheral pulses can be felt wherever an artery lies near the surface of the skin and over a firm background such as bone; sites: radial—at wrist; carotid—along anterior edge of sternocleidomastoid muscle, at level of lower margin of thyroid cartilage; brachial—at bend of the elbow, along inner margin of biceps muscle; femoral—in groin; popliteal—behind knee; posterior tibial—behind medial malleolus; dorsalis pedis—on anterior surface of foot, just below bend of the ankle; volume or amplitude of pulse may be absent, thready, diminished, have an acceptable volume, or bounding (Figure 6-3: Palpation of the arterial pulses) 5. Pulse deficit: difference between apical and radial pulses 6. Blood pressure: systolic—pressure within arteries when heart is contracting; diastolic—pressure within arteries when heart is at rest between contractions; pulse pressure—difference between systolic and diastolic pressures 1. Carry blood toward heart (all veins except pulmonary veins carry deoxygenated blood) 2. Branch into venules, which collect blood from capillaries; veins in cranial cavity formed by dura mater are called sinuses 3. Structure: same three coats as arteries, but thinner and fewer elastic and muscle fibers, allowing veins to collapse when cut; semilunar valves present in most veins more than 2 mm in diameter prevent backward flow of blood 1. Carry blood from arterioles and unite to form small veins or venules, which in turn unite to form veins 2. Exchange of substances between blood and interstitial fluid occurs in capillaries 3. Structure: only lining coat present (intima); wall only one cell thick to allow for diffusion of gases and small molecules 1. Sympathetic nervous system: increases heart rate and cardiac contractility, dilates coronary and skeletal blood vessels, and constricts blood vessels supplying abdominal organs and skin through stimulation of alpha- and beta-adrenergic receptors by catecholamines (epinephrine, norepinephrine, dopamine) 2. Parasympathetic nervous system: decreases heart rate and contractility, and causes vasodilation through cholinergic fibers; stimulation of vagus nerve initiates parasympathetic response 3. Baroreceptors in the aortic arch and carotid sinus respond to changes in BP a. Increased arterial BP baroreceptors, which causes parasympathetic responses (vasodilation and decreased heart rate and contractility) b. Decreased arterial pressure inhibits baroreceptors, which results in increased sympathetic responses (vasoconstriction and increased heart rate and contractility) 4. Chemoreceptors respond to changes in levels of oxygen, carbon dioxide, and blood pH by stimulating the autonomic nervous system B Renin-angiotensin-aldosterone mechanism: when renal perfusion decreases, there is retention of sodium and water, which increases blood volume; vasoconstriction occurs, which increases BP C Intrinsic circulatory regulation: increased BP raises hydrostatic pressure of plasma, leading to increased filtration of plasma from intravascular to interstitial spaces, resulting in reduced venous return, decreased cardiac output, and decreased BP 1. Structure: lymph capillaries similar to blood capillaries in structure; larger lymphatics similar to veins but are thinner-walled, have more valves, and have lymph nodes along their course 2. Functions: return fluid and interstitial proteins to the venous system via thoracic and right lymphatic ducts at the junction between internal jugular and subclavian veins; interference with return of proteins to the blood results in edema 1. Located throughout the body; usually occur in clusters 2. Functions: help defend the body against foreign substances (notably, bacteria and tumor cells) 1. Location: left hypochondrium, above and behind cardiac portion of the stomach a. Reticuloendothelial cells form macrophages that protect the body from antigens through phagocytosis; removes damaged cells from circulation b. Contains B and T lymphocytes essential for humoral and cellular immune responses c. Sequesters newly formed reticulocytes until they become mature erythrocytes; serves as reservoir of erythrocytes and platelets; sympathetic stimulation causes constriction of its capsule, squeezing out an estimated 200 mL of blood into general circulation within 1 minute d. Participates in the formation and development of blood cells (hematopoiesis) if bone marrow fails to function A Streptococcus pyogenes: gram-positive streptococcus; most virulent strain (group A beta hemolytic) causes scarlet fever, septic sore throat, tonsillitis, cellulitis, puerperal fever, erysipelas, rheumatic fever, and glomerulonephritis B Streptococcus viridans: gram-positive streptococcus; distinguishable from S. pyogenes by its alpha hemolysis (rather than beta) of RBCs; common cause of infective endocarditis C Staphylococcus aureus: gram-positive cocci associated with infective endocarditis in IV drug users 1. Increase force of cardiac contraction (positive inotropic effect) by increasing permeability of cardiac muscle membranes to calcium and sodium ions required for contraction of muscle fibrils 2. Decrease rate of cardiac contractions (negative chronotropic effect) by an action mediated through the vagus nerve; this action slows firing of the SA node and slows impulse transmission at the AV node 3. Slow conduction velocity (negative dromotropic effect); occurs by direct action and by increased vagal stimulation 4. Increase cardiac output by increasing effectiveness of heart pump 5. Effective in treating heart failure and atrial flutter and fibrillation 6. Available in oral and parenteral (intramuscular [IM], IV) preparations 7. Digitalization: rapid or slow administration of a loading dose to reach the therapeutic blood level; after desired effect is achieved the dosage is kept at a maintenance level, which replaces amount of drug metabolized and excreted each day 8. Used less often than newer classifications of cardiac medications because of high risk of toxicity B Examples: digitalis; digoxin (Lanoxin) C Major side effects: diarrhea (local effect), nausea, vomiting (malabsorption of all nutrients); bradycardia (increased vagal tone at AV node) D Toxicity: premature ventricular complexes (increased spontaneous rate of ventricular depolarization), xanthopsia/yellow vision (effect on visual cones); muscle weakness (central nervous system [CNS] effect, neurotoxicity, hypokalemia), blurred vision (CNS effect), anorexia and vomiting (local effect stimulates chemoreceptor zone in medulla); toxicity treated with digoxin immune Fab (Digibind) 1. Check apical pulse before administration: withhold dose and contact health care provider if rate is excessively slow (parameter set by health care provider; usually below 50 to 60 beats/min) 2. Encourage intake of potassium-rich foods unless potassium supplement is prescribed 3. Assess for signs of impending toxicity (e.g., anorexia, nausea, vomiting, dysrhythmias, xanthopsia) 4. Monitor for hypokalemia, which potentiates the effects of digitalis; electrocardiogram (ECG) will indicate depressed T waves with hypokalemia 5. Instruct to count radial pulse and record before each administration; notify health care provider of side effects; report any changes in heart rate or rhythm 6. Digoxin—monitor blood level during therapy (therapeutic serum level: 0.5 to 2.0 ng/mL) 1. Class IA antidysrhythmics: suppress ectopic foci by increasing refractory period and slowing depolarization: disopyramide (Norpace), quinidine preparations (e.g., quinidine sulfate, quinidine polygalacturonate [Cardioquin]) 2. Class IB antidysrhythmics: suppress ventricular dysrhythmias by decreasing automaticity and increasing ventricular electrical stimulation threshold; lidocaine, phenytoin (Dilantin) 3. Class IC antidysrhythmics: slow conduction and increase ventricular refractoriness: flecainide (Tambocor) 4. Class II antidysrhythmics (beta blockers or beta-adrenergic blockers): decrease heart rate, contractility, and automaticity by blocking beta-adrenergic receptor sites from catecholamines; decrease myocardial workload and oxygen requirements; indicated for tachydysrhythmias, hypertension, angina; propranolol (Inderal), metoprolol (Lopressor), atenolol (Tenormin), timolol (Blocadren), nadolol (Corgard), sotalol (Betapace) 5. Class III antidysrhythmics: prolong repolarization; amiodarone (Cordarone) for ventricular tachycardia and fibrillation; dofetilide (Tikosyn) and, ibutilide (Corvert) for atrial flutter and fibrillation 6. Class IV antidysrhythmics (calcium channel blockers or calcium antagonists): block calcium influx into muscle cells during depolarization; control atrial dysrhythmias by decreasing cardiac automaticity and impulse conduction; reduce peripheral vascular resistance in treatment of hypertension: diltiazem (Cardizem), NIFEdipine (Procardia), verapamil (Calan), felodipine (Plendil) C Major side effects: hypotension (decreased cardiac output caused by vasodilation); dizziness (hypotension); nausea and vomiting (irritation of gastric mucosa); heart block (direct cardiac toxic effect, cardiac depressant effect); heart failure (decreased contractility); anticholinergic effect (decreased parasympathetic stimulation); blood dyscrasias (e.g., decreased RBCs, WBCs, and platelet synthesis) D Toxicity: diarrhea (gastrointestinal [GI] irritation), CNS disturbances (neurotoxicity), sensory disturbances (neurotoxicity) 1. Assess vital signs during course of therapy; monitor drug blood levels 2. Use cardiac monitoring during IV administration; ensure follow-up ECGs 3. Use infusion-control device for continuous IV administration 4. Administer oral preparations with meals to reduce GI irritation 5. Use safety precautions (e.g., recumbent position, supervised ambulation, side rails) when CNS effects are manifested 6. Instruct to notify health care provider of side effects (e.g., changes in heart rate or rhythm, fatigue, weight gain, bleeding) 7. Instruct to change positions slowly; increase fiber and fluid intake to prevent constipation 8. Use caution when administering beta blockers to clients with diabetes (may mask signs of hypoglycemia), bronchospasms, or heart failure 2. Act by either indirect or direct mechanisms affecting autonomic nervous system 3. Available in parenteral (IM, IV), endotracheal, and intracardiac preparations 1. Atropine (atropine sulfate): suppresses parasympathetic nervous system control at SA and AV nodes by reducing vagal stimulation, thus allowing heart rate to increase 2. EpiNEPHrine (Adrenalin): stimulates rate and force of cardiac contraction via sympathetic nervous system C Major side effects: tachycardia (sympathetic stimulation); headache (dilation of cerebral vessels); CNS stimulation (sympathetic stimulation); cardiac dysrhythmias (cardiovascular system stimulation); atropine causes anticholinergic effects resulting from decreased parasympathetic stimulation (e.g., dry mouth, blurred vision, urinary retention) 1. Decrease cardiac workload and myocardial oxygen requirements by vasodilatory action that decreases preload and afterload 2. Nitrates act directly at receptors in smooth muscles, causing vasodilation, which decreases preload, thus decreasing cardiac workload 3. Calcium channel blockers inhibit influx of calcium ions across cell membranes during depolarization of cardiac and vascular smooth muscle 4. Effective in treatment of angina pectoris 5. Available in oral, sublingual tablets and spray, sustained-release buccal, topical (including transdermal), and IV preparations 1. Nitrates (sublingual): nitroglycerin, isosorbide dinitrate (Isordil, Sorbitrate) 2. Nitrates (oral): isosorbide dinitrate (Isordil, Sorbitrate) 4. Nitrates (IV): nitroglycerin (Nitro-Bid IV, Tridil); nitroprusside (Nitropress) 5. Calcium channel blockers: see Class IV antidysrhythmics C Major side effects: headache (dilation of cerebral vessels); flushing (peripheral vasodilation); orthostatic hypotension (loss of compensatory vasoconstriction with position change); tachycardia (reflex reaction to severe hypotension); dizziness (orthostatic hypotension) 1. Assess for hypotension before administering; if present, withhold drug 2. Encourage to change positions slowly and remain seated after taking sublingual nitroglycerin to avoid orthostatic hypotension 3. Instruct to take sublingual nitroglycerin preparations before angina-producing activities; for chest pain take sublingual preparations every 5 minutes, not to exceed three in 15 minutes; obtain emergency care if pain persists 4. Store in original amber glass container; avoid placing in heat, light, moisture, or plastic 5. Explain that slight stinging, burning, or tingling under the tongue indicates potency of drug; obtain a new supply every 3 months 6. Wear clean gloves when administering topical preparation to prevent absorption through fingers 7. Use glass container and tubing supplied by manufacturer when administering IV nitroglycerin preparations; standard tubing can absorb nitroglycerin; titrate using an infusion control pump; monitor BP every 5 to 15 minutes a. Promote dilation of peripheral blood vessels, thus decreasing BP, peripheral vascular resistance, and afterload b. Reduce cardiac contractility 2. Available in oral, parenteral (IM, IV), and transdermal preparations 1. Angiotensin-converting enzyme inhibitors (ACEIs): stop conversion of angiotensin I to II, blocking vasoconstriction and fluid retention from aldosterone secretion; captopril (Capoten), enalapril (Vasotec), benazepril (Lotensin), lisinopril (Prinivil, Zestril), quinapril (Accupril), fosinopril (Monopril) 2. Angiotensin II receptor blockers (ARBs): block angiotensin II from binding to specific vascular smooth muscle and adrenal gland receptor sites; stop vasoconstriction and fluid retention; similar antihypertensive effect of ACEIs but less likely to cause chronic cough: candesartan (Atacand), irbesartan (Avapro), losartan (Cozaar), valsartan (Diovan) 3. Calcium channel blockers (see Class IV antidysrhythmics) 5. Beta blockers (see Class II antidysrhythmics) 6. Alpha1 blockers: inhibit effects of norepinephrine by blocking receptors that control vasomotor tone; doxazosin (Cardura), prazosin (Minipress), terazosin (Hytrin) 7. Alpha-beta blockers: combine effects of alpha1 and beta blockers, leading to vasodilation, decreased contractility, and decreased heart rate; labetalol (Normodyne), carvedilol (Coreg) 8. Central alpha2 agonists: decrease sympathetic activity from CNS; clonidine (Catapres), methyldopa (Aldomet) 9. Direct vasodilators: relax smooth muscles of arterioles, resulting in decreased peripheral vascular resistance; hydrALAZINE (Apresoline), minoxidil (Loniten), nitroprusside (Nitropress), diazoxide (Hyperstat IV) 1. Orthostatic hypotension (loss of compensatory vasoconstriction with position change) 2. Dizziness (orthostatic hypotension); drowsiness (cerebral hypoxia) 3. Cardiac rate alteration: bradycardia caused by sympatholytics (decreased sympathetic stimulation to heart); tachycardia caused by direct relaxers (reflex reaction to severe hypotension) 4. Sexual disturbances (failure of erection or ejaculation caused by loss of vascular tone) 5. Blood dyscrasias (hemolytic anemia, decreased WBCs, decreased platelet synthesis) 6. Beta blockers can cause bronchospasm and mask hypoglycemia 7. ACEIs may cause a dry cough; small percentage may develop life-threatening angioedema 1. Assess vital signs, especially pulse rate; monitor BP in standing and supine positions; ensure systolic pressure is maintained at greater than 80 mm Hg 2. Monitor urinary output during initial titration 3. Protect nitroprusside IV solution from light during administration 4. Instruct to follow a low-sodium diet; eat foods high in B-complex vitamins 5. Inform to continue taking medication as prescribed because therapy usually is life-long and abrupt cessation may lead to rebound hypertension 6. Teach to avoid engaging in hazardous activities when initially taking antihypertensives; change positions slowly 7. Teach to report side effects; report significant weight loss because dose may need to be adjusted 1. Interfere with sodium reabsorption in kidney 2. Increase urine output, which reduces hypervolemia; decrease preload and afterload 1. Thiazides: interfere with sodium ion transport at loop of Henle and inhibit carbonic anhydrase activity at distal tubule sites; chlorothiazide (Diuril); hydrochlorothiazide (HCTZ, HydroDIURIL); metolazone (Zaroxolyn) which is a thiazide-like diuretic 2. Potassium-sparers: interfere with aldosterone-induced reabsorption of sodium ions at distal nephron sites to increase sodium chloride excretion and decrease potassium ion loss; spironolactone (Aldactone), triamterene (Dyrenium), amiloride (Midamor) 3. Loop diuretics: interfere with active transport of sodium ions in loop of Henle and inhibit sodium chloride and water reabsorption at proximal tubule sites; may be given IV; furosemide (Lasix), bumetanide (Bumex), and torsemide (Demadex) C Major side effects: GI irritation (local effect); hyponatremia (inhibition of sodium reabsorption at the kidney tubule); orthostatic hypotension (reduced blood volume); hyperuricemia (partial blockage of uric acid excretion); dehydration (excessive sodium and water loss); hyperglycemia; furosemide (Lasix) may cause hearing problems when administered rapidly 1. All diuretics except potassium-sparers: hypokalemia (increased potassium excretion); increased urinary excretion of magnesium and zinc 2. Potassium-sparers: hyperkalemia (reabsorption of potassium at kidney tubule); hypomagnesemia (increased excretion of magnesium at kidney tubule); hypocalcemia (increased urinary excretion of calcium) 3. Furosemide (Lasix) competes with aspirin for renal excretion sites and may cause aspirin (ASA) toxicity 4. Thiazides and loop diuretics may cause hyperglycemia in clients with diabetes 1. Monitor intake and output (I&O); weigh daily (same time, scale, clothing); assess for signs of fluid-electrolyte imbalance 2. Administer in the morning so that maximal effect occurs during waking hours 3. Monitor pulse rate and BP; instruct to change position slowly 4. Encourage intake of foods high in calcium, magnesium, zinc, and potassium (except if taking potassium-sparers) 1. Constrict peripheral blood vessels and/or increase cardiac output through alpha- and beta-adrenergic stimulation B Examples: norepinephrine (Levophed), phenylephrine (Neo-Synephrine), DOPamine (Intropin), DOBUTamine (Dobutrex); vasopressin (Pitressin) in high doses is a nonadrenergic vasoconstrictor C Major side effects: hypertension (compression of cerebral blood vessels); headache (increase in BP); GI disturbance (autonomic dysfunction) 1. Prevent fibrin formation by interfering with production of various clotting factors in the coagulation process 2. Prevent platelet aggregation and clot extension 3. Used for prevention and treatment of thrombus and embolus 4. Available in oral and parenteral (subcutaneous [Sub-Q], IV) preparations; may be given concurrently until oral medication reaches therapeutic level 1. Heparin sodium: administered IV or Sub-Q 2. Low-molecular-weight heparin administered Sub-Q: enoxaparin (Lovenox), dalteparin (Fragmin), fondaparinux (Arixtra) 3. Dabigatran (Pradaxa); a direct thrombin inhibiter; benefit is routine blood coagulation studies are unnecessary 4. Lepirudin (Refludan) administered IV; indicated for clients who have heparin-induced thrombocytopenia (HIT) 5. Warfarin (Coumadin) administered orally 6. Antiplatelet drugs administered orally: ASA, ticlopidine (Ticlid), clopidogrel (Plavix) C Major side effects: fever, chills, bronchospasm (hypersensitivity); skin rash (hypersensitivity); petechiae, bruising, hemorrhage (interference with clotting mechanisms); diarrhea (GI irritation); thrombocytopenia and other blood dyscrasias; ASA may cause tinnitus and hearing loss 1. Monitor blood work when client is receiving warfarin (Coumadin) b. International normalized ratio (INR): therapeutic value should be 2.0 to 3.5; change in drug regimen requires more frequent INRs because many drugs have interactive effects 2. Monitor blood work when client is receiving heparin derivatives b. Prothrombin time (PT); therapeutic value should be 1.5 to 2 times the normal value c. Activated partial thromboplastin time (aPTT); therapeutic value should be 1.5 to 2 times normal value when given as a continuous IV drip 3. Monitor blood work if surgery cannot be delayed when client is receiving dabigatran (Pradaxa) to evaluate bleeding risk 4. Administer subcutaneous heparin in the abdomen; do not aspirate or massage the area 5. Have appropriate antidote available: vitamin K for warfarin; protamine sulfate for heparin 6. Assess for signs of bleeding 7. Avoid intramuscular injections and salicylates with the concomitant administration of anticoagulants to prevent bleeding 8. Instruct to carry a medical alert card; immediately report signs of bleeding or injury; avoid alcohol and medications containing aspirin 9. Instruct to avoid interacting herbal supplements (e.g., garlic, ginseng, green tea, and St. John’s wort); avoid excessive intake of dietary sources of vitamin K and cranberry juice when taking warfarin sodium 10. Maintain safety precautions (e.g., use electric razor and soft toothbrush) to prevent bleeding 11. Follow schedule for coagulation studies; may be daily, weekly, monthly, or every 3 months 1. Convert plasminogen to plasmin, which initiates local fibrinolysis 3. Administered intravenously or intraarterially 4. Initial loading dose is administered concomitantly with heparin 5. Therapy must be instituted within hours of the onset of myocardial infarction, pulmonary embolism, or acute ischemic brain attack B Examples: streptokinase (Streptase); tissue plasminogen activator (t-PA) such as alteplase (Activase) C Major side effects: bleeding, especially GI if there is a history of peptic ulcer disease or cerebral if there is a history of uncontrolled hypertension (increased fibrinolytic activity); allergic reactions (introduction of a foreign protein); low-grade fever (resulting from absorption of infarcted tissue); reperfusion dysrhythmias 1. Screen clients for contraindications and complete all venipuncture procedures before initiating therapy; observe for signs of bleeding; monitor PTT and fibrinogen concentration; monitor vital signs and neurologic status 2. Assess for signs of allergic reactions such as chills, urticaria, pruritus, rash, and malaise 3. Keep aminocaproic acid (Amicar), a fibrinolysis inhibitor, available 4. Maintain continuous IV infusion of heparin after thrombolytic therapy 1. Promote RBC production; effective in treatment of anemia caused by chronic kidney disease or chemotherapy, iron deficiency anemia, and inadequate nutrition 2. Colony-stimulating factors stimulate red blood cell production; iron-containing compounds and vitamin replacements needed for the formation of RBCs 3. Available in oral and parenteral (IM, IV, Sub-Q) preparations 1. Colony-stimulating factors: epoetin (Epogen, Procrit) administered Sub-Q or IV three times a week 2. Iron compounds: oral—ferrous gluconate, ferrous sulfate; parenteral—iron dextran 3. Vitamin replacements: cyanocobalamin—vitamin B12, folic acid—vitamin B9 1. Epoetin: seizures, hypertension, thrombotic events 2. Iron replacements: nausea, vomiting (irritation of gastric mucosa); constipation (delayed passage of iron and stool); black stools (presence of unabsorbed iron in stool); stained teeth (liquid preparations that come into contact with enamel); tissue staining (injectable preparations that leak iron into tissue) 3. Vitamin replacements: local irritation (tissue effect at injection site or in mouth); allergic reactions, anaphylaxis (hypersensitivity); diarrhea (GI irritation) a. Monitor BP, hematocrit, patency of dialysis shunt if present b. Institute seizure precautions if there is a precipitous rise in hematocrit level a. Inform about side effects of therapy b. Teach to take liquid preparations diluted with water or fruit juice through a straw on an empty stomach, if possible, for optimum absorption; take ascorbic acid (vitamin C) concurrently because it increases iron absorption; encourage oral hygiene after iron administration to prevent staining of teeth and irritation of oral mucosa c. Encourage intake of foods high in iron, vitamin B12, and folic acid; increase high-fiber foods to reduce potential of constipation d. Have available deferoxamine (Desferal), the antidote for iron toxicity 1. Improve lipid profile by reducing cholesterol or triglyceride synthesis and/or increasing high-density lipoprotein (HDL) level 2. Used to attain recommended goals for low-density lipoprotein (LDL) levels established by the National Cholesterol Education Program’s (NCEP) Adult Treatment Panel (ATP III) (ATP IV will be available in fall 2011) 1. HMG-CoA reductase inhibitors (statins): lower levels of total cholesterol, LDL, and triglycerides; increase HDL levels; pravastatin (Pravachol), lovastatin (Mevacor), simvastatin (Zocor); atorvastatin (Lipitor) 2. Fibrates: decrease levels of total cholesterol, LDL, and triglycerides; gemfibrozil (Lopid), fenofibrate (Tricor) 3. Bile acid sequestrants: bind with intestinal bile, preventing absorption and lowering LDL and total cholesterol levels; cholestyramine (Questran), colestipol (Colestid) 4. Nicotinic acid reduces levels of total cholesterol, triglycerides, and LDL; increases HDL levels 1. Nausea, vomiting, diarrhea (GI irritation) 2. Musculoskeletal disturbances (direct musculoskeletal tissue effect) 3. Hepatic disturbances (hepatic toxicity) 4. Reduced absorption of fat and fat-soluble vitamins (A, D, E, K) as well as vitamin B12 and iron 5. Statins: rhabdomyolysis (potentially fatal skeletal muscle disease) 6. Bile acid sequestrants: constipation 1. Encourage adherence to dietary program a. Low cholesterol, low fat (especially saturated) b. Replace vegetable oils high in polyunsaturated fatty acid with those high in monounsaturated fatty acid (e.g., olive oil, canola oil) c. Eat fish high in omega-3 fatty acids several times per week (e.g., salmon, tuna, halibut) d. Increase intake of high-fiber foods (e.g., fruits, vegetables, cereal grains, legumes); soluble fibers (e.g., oat, bran, legumes) are particularly effective in reducing blood lipid levels
Nursing Care of Clients with Circulatory System (Cardiovascular, Blood, and Lymphatic Systems) Disorders
Overview
Review of Anatomy and Physiology
Blood
Heart
Blood Vessels
Regulatory Mechanisms Affecting Circulation
Lymphatic System
Review of Microorganisms
![]() Related Pharmacology
Related Pharmacology
Cardiac Glycosides
Antidysrhythmics
Cardiac Stimulants
Coronary Vasodilators
Antihypertensives
Diuretics
Medications to Manage Hypotension in Shock
Anticoagulants
Thrombolytics (Fibrinolytics)
Antianemics
Antilipidemics
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



Nursing Care of Clients with Circulatory System (Cardiovascular, Blood, and Lymphatic Systems) Disorders
Get Clinical Tree app for offline access