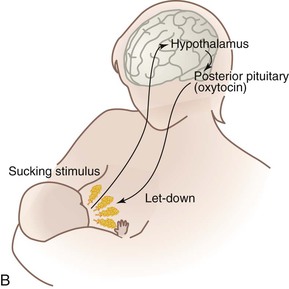
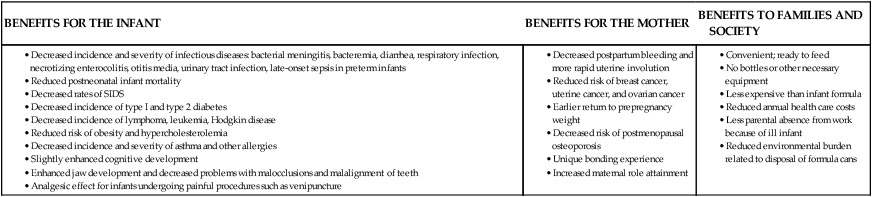
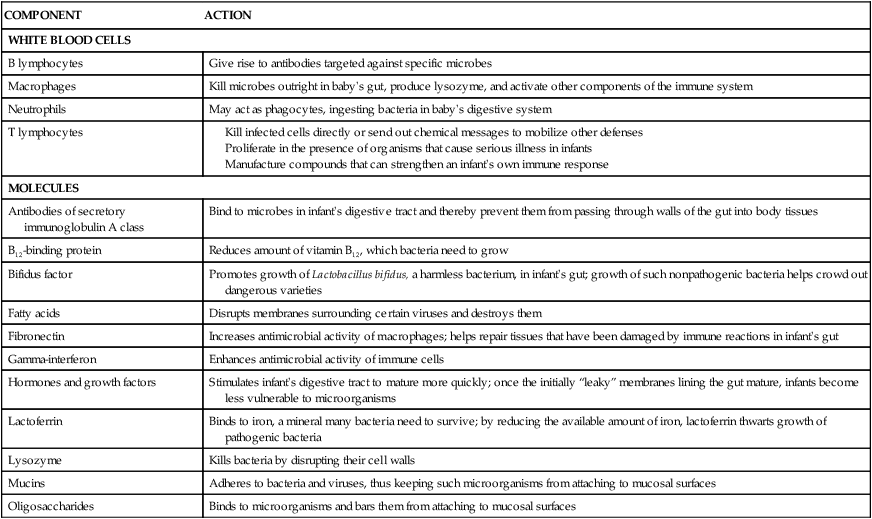
• Describe current recommendations for infant feeding. • Explain the nurse’s role in helping families choose an infant feeding method. • Discuss benefits of breastfeeding for infants, mothers, families, and society. • Describe nutritional needs of infants. • Describe the anatomic and physiologic aspects of breastfeeding. • Recognize newborn feeding-readiness cues. • Explain maternal and infant indicators of effective breastfeeding. • Examine nursing interventions to facilitate and promote successful breastfeeding. • Analyze common problems associated with breastfeeding and nursing interventions to help resolve them. • Compare powdered, concentrated, and ready-to-use forms of commercial infant formula. Additional related content can be found on the companion website at http://evolve.elsevier.com/Lowdermilk/Maternity/ • Critical Thinking Exercise: Breastfeeding • Critical Thinking Exercise: Formula Preparation • Nursing Care Plan: Breastfeeding and Infant Nutrition • Nursing Care Plan: The Newborn with Insufficient Intake of Nutrients • Spanish Guidelines: Breastfeeding: Latching On Through preconception and prenatal education and counseling, nurses play an instrumental role in assisting parents with the selection of an infant feeding method. Scientific evidence is clear that human milk provides the best nutrition for infants, and parents should be strongly encouraged to choose breastfeeding (American Academy of Pediatrics [AAP] Section on Breastfeeding, 2012). Although many health care providers and the general public may consider artificial baby milk (infant formula) to be equivalent to breast milk, this belief is erroneous. Human milk is species specific, uniquely designed to meet the needs of human infants. The composition of human milk changes to meet the nutritional needs of growing infants. It is highly complex, with antiinfective and nutritional components combined with growth factors, enzymes that aid in digestion and absorption of nutrients, and fatty acids that promote brain growth and development. Infant formulas are usually adequate in providing nutrition to maintain infant growth and development within normal limits, but they are not equivalent to human milk. The AAP recommends exclusive breastfeeding or human milk feeding for the first 6 months of life and that breastfeeding or human milk feeding continue as the sole source of milk for the first year. During the second 6 months of life, appropriate complementary foods (solids) are added to the infant diet. If infants are weaned from breast milk before 12 months of age, they should receive iron-fortified infant formula, not cow’s milk (AAP Section on Breastfeeding, 2012). According to the Global Strategy for Infant and Young Child Feeding, endorsed by the World Health Organization (WHO) and United Nations Children’s Fund (UNICEF), infants should be exclusively breastfed for 6 months, and breastfeeding should continue for up to 2 years and beyond (WHO/UNICEF, 2003). Breastfeeding rates in the United States have risen steadily over the past decade. The Centers for Disease Control and Prevention (CDC, 2012) reported that the U.S. breastfeeding initiation rate in 2009 was 76.9%, which is the highest ever reported. Despite increases in breastfeeding rates, the U.S. continues to fall short of the Healthy People 2020 goals (USDHHS, 2010). Trends remain unchanged in breastfeeding rates among minority groups in the United States. The lowest rates are among non-Hispanic black women, although the overall percentage has increased in recent years. The minority group most likely to breastfeed is Hispanic women (Scanlon, Grummer-Strawn, Li, et al, 2010). Numerous research studies have identified the beneficial effects of human milk for infants during the first year of life. Long-term epidemiologic studies have shown that these benefits do not cease when the infant is weaned; instead, these benefits extend into childhood and beyond. Breastfeeding has many advantages for mothers, for families, and for society in general (AAP Section on Breastfeeding, 2012; Lawrence & Lawrence, 2011; Ip et al., 2009). In discussing the benefits of breastfeeding with parents, nurses and other health care professionals must have a thorough understanding of these benefits from both a physiologic and a psychosocial perspective. Table 18-1 lists the benefits of breastfeeding. TABLE 18-1 SIDS, Sudden infant death syndrome. Sources: American Academy of Pediatrics Section on Breastfeeding. (2012). Breastfeeding and the use of human milk policy statement. Pediatrics, 129(3), e827-e841; Ip, S., Chung, M., Raman, G., Trikalinos, T.A., & Lau, J. (2009). A summary of the Agency for Healthcare Research and Quality’s evidence report on breastfeeding in developed countries. Breastfeeding Medicine, 4(Suppl 1), S17-S30. Breastfeeding is a natural extension of pregnancy and childbirth; it is much more than simply a means of supplying nutrition for infants. Women most often breastfeed their babies because they are aware of the benefits to the infant (Nelson, 2012). Many women seek the unique bonding experience between mother and infant that is characteristic of breastfeeding. Women tend to select the same method of infant feeding for each of their children. If the first child was breastfed, subsequent children will likely also be breastfed (Taylor, Geller, Risica, Kirtania, & Cabral, 2008). The support of the partner and family is a major factor in the mother’s decision to breastfeed. Women who perceive their partners to prefer breastfeeding are more likely to choose this method of infant feeding. Women are more likely to breastfeed successfully when partners and family members are positive about breastfeeding and have the skills to support breastfeeding (Clifford & McIntyre, 2008). Breastfeeding is contraindicated in a few situations. Newborns who have galactosemia should not be breastfed. Mothers with active tuberculosis or human immunodeficiency virus infection and those who are positive for human T-cell lymphotropic virus type I or type II should not breastfeed. Breastfeeding is not recommended when mothers are receiving chemotherapy or radioactive isotopes (e.g., with diagnostic procedures). Maternal use of drugs of abuse (“street drugs”) is incompatible with breastfeeding (AAP Section on Breastfeeding, 2012; Lawrence & Lawrence, 2011). The key to encouraging mothers to breastfeed is education and anticipatory guidance, beginning as early as possible during pregnancy and even before pregnancy. Each encounter with an expectant mother is an opportunity to educate, dispel myths, clarify misinformation, and address personal concerns. Prenatal education and preparation for breastfeeding influence feeding decisions, breastfeeding success, and the amount of time that women breastfeed (Rosen, Krueger, Carney, & Graham, 2008). Prenatal preparation ideally includes the father of the baby, partner, or another significant support person, providing information about benefits of breastfeeding and how he or she can participate in infant care and nurturing. Connecting expectant mothers with women from similar backgrounds who are breastfeeding or have successfully breastfed is often helpful. Nursing mothers’ support groups provide information about breastfeeding along with opportunities for breastfeeding mothers to interact with one another and share concerns (Fig. 18-1). Peer counseling programs, such as those instituted by Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) programs, are beneficial. Promoting feelings of competence and confidence in the breastfeeding mother and reinforcing the unequaled contribution she is making toward the health and well-being of her infant are the responsibility of the nurse and other health care professionals. Women who are optimistic, with a sense of breastfeeding self-efficacy, and faith in breast milk as the best nutrition for the infant are likely to breastfeed longer (O’Brien, Buikstra, & Hegney, 2008). The most common reasons for breastfeeding cessation are insufficient milk supply, painful nipples, and problems getting the infant to feed. Early and ongoing assistance and support from health care professionals to prevent and address problems with breastfeeding can help promote a successful and satisfying breastfeeding experience for mothers and infants (Renfrew & Hall, 2008). Many health care agencies have lactation consultants on staff. These health care professionals who are usually nurses have specialized training and experience in assisting breastfeeding mothers and infants. Evidence-based guidelines for supporting breastfeeding are available for use by health care professionals (Association of Women’s Health, Obstetric and Neonatal Nurses [AWHONN], 2007; International Lactation Consultant Association [ILCA], 1999). In general, persons who have immigrated to the United States from poorer countries often choose to formula-feed their infants because they believe it is a better, more “modern” method or because they want to adapt to U.S. culture and perceive that bottle feeding is the custom. However, this notion is not always true. For example, Hispanic women born in the United States are less likely to breastfeed, whereas Hispanic women who have recently immigrated tend to choose the social norm of breastfeeding that is characteristic of their homeland (Ahluwalia, D’Angelo, Morrow, et al., 2012). Breastfeeding beliefs and practices vary across cultures. For example, among the Muslim culture, breastfeeding for 24 months is customary. Before the first feeding, rubbing a small piece of softened date on the newborn’s palate is a ritual practice. Because of the cultural emphasis on privacy and modesty, Muslim women may choose to bottle-feed formula or expressed breast milk while in the hospital (Shaikh & Ahmed, 2006). Because of beliefs about the harmful nature or inadequacy of colostrum, some cultures apply restrictions on breastfeeding for a period of days after birth. Such is the case for many cultures in Southern Asia, the Pacific Islands, and parts of sub-Saharan Africa. Before the mother’s milk is deemed to be “in,” babies are fed prelacteal food such as honey or clarified butter, in the belief that these substances will help to clear out the meconium (Laroia & Sharma, 2006; Shaikh & Ahmed, 2006). Other cultures begin breastfeeding immediately and offer the breast each time the infant cries. A common practice among Latina women is to combine breastfeeding with formula feeding during the first week of life. This practice can potentially result in problems with milk supply and babies refusing to latch on to the breast, which can lead to early termination of breastfeeding (Bartick & Reyes, 2012). During the first 2 days of life the fluid requirement for healthy infants (>1500 g) is 60 to 80 ml of water per kilogram of body weight per day. From day 3 to 7 the requirement is 100 to 150 ml/kg/day and from day 8 to day 30, 120 to 180 ml/kg/day (Dell & Davis, 2011). In general, neither breastfed nor formula-fed infants need to be given water, not even those living in very hot climates. Breast milk contains 87% water, which easily meets fluid requirements. Feeding water to infants may only decrease caloric consumption at a time when infants are growing rapidly. Infants require adequate caloric intake to provide energy for growth, digestion, physical activity, and maintenance of organ metabolic function. Energy needs vary according to age, maturity level, thermal environment, growth rate, health status, and activity level. For the first 3 months the infant needs 110 kcal/kg/day. From 3 months to 6 months the requirement is 100 kcal/kg/day. This level decreases slightly to 95 kcal/kg/day from 6 to 9 months and increases to 100 kcal/kg/day from 9 months to 1 year (AAP Committee on Nutrition, 2009). According to the Institute of Medicine (IOM) (2005), the adequate daily reference intake (DRI) for carbohydrate in the first 6 months of life is 60 g/day and 95 g/day for the second 6 months. Because newborns have only small hepatic glycogen stores, carbohydrates should provide at least 40% to 50% of the total calories in the diet. Moreover, newborns may have a limited ability to carry out gluconeogenesis (the formation of glucose from amino acids and other substrates) and ketogenesis (the formation of ketone bodies from fat), the mechanisms that provide alternative sources of energy. The average recommended DRI of fat for infants younger than 6 months is 31 g/day (IOM, 2005). For infants to acquire adequate calories from human milk or formula, at least 15% of the calories provided must come from fat (triglycerides). The fat content of human milk is composed of lipids, triglycerides, and cholesterol; cholesterol is an essential element for brain growth. Human milk contains the essential fatty acids (EFAs), linoleic acid, and linolenic acid, as well as the long-chain polyunsaturated fatty acids, arachidonic acid (ARA), and docosahexaenoic acid (DHA). Fatty acids are important for growth, neurologic development, and visual function. Cow’s milk contains fewer of the EFAs and no polyunsaturated fatty acids. Most formula companies are now adding DHA and ARA to their products. Studies of infants receiving supplements of DHA and ARA have shown mixed results in terms of visual acuity and cognitive function (Heird, 2007; Simmer, Patole, & Rao, 2008). High-quality protein from breast milk, infant formula, or other complementary foods is necessary for infant growth. The protein requirement per unit of body weight is greater in the newborn than at any other time of life. For infants younger than 6 months the average DRI for protein is 9.1 g/day (IOM, 2005). Human milk contains the two proteins, whey (lactalbumin) and casein (curd), in a ratio of approximately 60 : 40, as compared with the ratio of 80 : 20 in most cow’s milk–based formula. This whey/casein ratio in human milk makes it more easily digested and produces the soft stools seen in breastfed infants. The whey protein lactoferrin in human milk has iron-binding capabilities and bacteriostatic properties, particularly against gram-positive and gram-negative aerobes, anaerobes, and yeasts. The casein in human milk enhances the absorption of iron, thus preventing iron-dependent bacteria from proliferating in the gastrointestinal tract (Lawrence & Lawrence, 2011). Vitamin D facilitates intestinal absorption of calcium and phosphorus, bone mineralization, and calcium reabsorption from bone. According to the AAP, all infants who are breastfed or partially breastfed should receive 400 international units of vitamin D daily, beginning the first few days of life. Nonbreastfeeding infants and older children who consume less than 1 quart per day of vitamin D–fortified milk should also receive 400 international units of vitamin D each day (Wagner, Grier, Section on Breastfeeding, & Committee on Nutrition, 2008). Vitamin K, required for blood coagulation, is produced by intestinal bacteria. However, the gut is sterile at birth, and a few days are required for intestinal flora to become established and produce vitamin K. To prevent hemorrhagic problems in the newborn an injection of vitamin K is given at birth to all newborns, regardless of feeding method (AAP Section on Breastfeeding, 2012). The ratio of calcium to phosphorus in human milk is 2 : 1, an optimal proportion for bone mineralization. Although cow’s milk is high in calcium, the calcium-to-phosphorus ratio is low, resulting in decreased calcium absorption. Consequently, young infants fed unmodified cow’s milk are at risk for hypocalcemia, seizures, and tetany. The calcium/phosphorus ratio in commercial infant formula is between that of human milk and cow’s milk. The average DRI for calcium is 210 mg/day for infants younger than 6 months and 270 mg/day for infants between 7 months and 1 year (IOM, 2005). Iron levels are low in all types of milk; however, iron from human milk is better absorbed than iron from cow’s milk, iron-fortified formula, or infant cereals. Breastfed infants draw on iron reserves deposited in utero and benefit from the high lactose and vitamin C levels in human milk that facilitate iron absorption. Full-term infants have enough iron stores from the mother to last four months. After that time, exclusively breastfed infants are at risk for iron deficiency. They should receive an iron supplement until they are consuming complementary foods that contain iron (e.g., iron-fortified cereals). Formula-fed infants should receive an iron-fortified commercial infant formula until 12 months of age. Infants should not be fed low-iron formula (Baker, Greer, & AAP Committee on Nutrition, 2010). Fluoride levels in human milk and commercial formulas are low. This mineral, which is important in the prevention of dental caries, may cause spotting of the permanent teeth (fluorosis) in excess amounts. Experts recommend that no fluoride supplements be given to infants younger than 6 months. From 6 months to 3 years, fluoride supplements are based on the concentration of fluoride in the water supply (AAP Section on Breastfeeding, 2012). Each female breast is composed of approximately 15 to 20 segments (lobes) embedded in fat and connective tissues and well supplied with blood vessels, lymphatic vessels, and nerves (Fig. 18-2). Within each lobe is glandular tissue consisting of alveoli, the milk-producing cells, surrounded by myoepithelial cells that contract to send the milk forward to the nipple during milk ejection. Each nipple has multiple pores that transfer milk to the suckling infant. The ratio of glandular tissue to adipose tissue in the lactating breast is approximately 2 : 1 compared with a 1 : 1 ratio in the nonlactating breast. Within each breast is a complex, intertwining network of milk ducts that transport milk from the alveoli to the nipple. The milk ducts dilate and expand at milk ejection. Previous thinking held that the milk ducts converged behind the nipple in lactiferous sinuses, which acted as reservoirs for milk. New research based on ultrasonography of lactating breasts has shown that these sinuses do not exist, and, in fact, glandular tissue can be found directly beneath the nipple (Geddes, 2007; Ramsay, Kent, Hartmann, & Hartmann, 2005) (Fig. 18-3). The size and shape of the breast are not accurate indicators of its ability to produce milk. Although nearly every woman can lactate, a small number of women have insufficient mammary gland development to breastfeed their infants exclusively. Typically, these women experience few breast changes during puberty or early pregnancy. In some cases, women may still be able to breastfeed and offer supplemental nutrition to support optimal infant growth. Devices are available to allow mothers to offer supplements while the baby is nursing at the breast (Fig. 18-4). Because of the effects of estrogen, progesterone, human placental lactogen, and other hormones of pregnancy, changes occur in the breasts in preparation for lactation. Breasts increase in size corresponding to growth of glandular and adipose tissue. Blood flow to the breasts nearly doubles during pregnancy. Sensitivity of the breasts increases, and veins become more prominent. The nipples become more erect, and the areola darken. Nipples and areola may enlarge. Around week 16 of gestation the alveoli begin producing colostrum (early milk). Montgomery glands on the areola increase in size and secretion. Secretions from these glands help provide protection against the mechanical stress of sucking and invasion by pathogens. The odor of the secretions may be a means of communication with the infant (Geddes, 2007). After the mother gives birth a precipitous fall in estrogen and progesterone levels triggers the release of prolactin from the anterior pituitary gland. During pregnancy, prolactin prepares the breasts to secrete milk and, during lactation, to synthesize and secrete milk. Prolactin levels are highest during the first 10 days after birth, gradually declining over time but remaining above baseline levels for the duration of lactation. Prolactin is produced in response to infant suckling and emptying of the breasts (NOTE: Lactating breasts are never completely empty; the alveoli constantly produce milk as the infant feeds) (Fig. 18-5, A). Milk production is a supply-meets-demand system; that is, as milk is removed from the breast, more is produced. Incomplete emptying of the breasts can lead to decreased milk supply. Oxytocin is the other hormone essential to lactation. As the nipple is stimulated by the suckling infant the posterior pituitary is prompted by the hypothalamus to produce oxytocin. This hormone is responsible for the milk ejection reflex (MER), or let-down reflex (Fig. 18-5, B). The myoepithelial cells surrounding the alveoli respond to oxytocin by contracting and sending the milk forward through the ducts to the nipple. Many “let-downs” can occur with each feeding session. Thoughts, sights, sounds, or odors that the mother associates with her baby (or other babies), such as hearing the baby cry, can all trigger the MER. Many women report a tingling “pins and needles” sensation in the breasts as milk ejection occurs, although some mothers can detect milk ejection only by observing the sucking and swallowing of the infant. The milk ejection reflex also may occur during sexual activity because oxytocin is released during orgasm. The reflex can be inhibited by fear, stress, and alcohol consumption. Human milk contains immunologically active components that provide some protection against a broad spectrum of bacterial, viral, and protozoan infections. Secretory IgA is the major immunoglobulin in human milk; IgG, IgM, IgD, and IgE are also present. Human milk also contains T and B lymphocytes, epidermal growth factor, cytokines, interleukins, Bifidus factor, complement (C3 and C4), and lactoferrin, all of which have a specific role in preventing localized and systemic bacterial and viral infections (Lawrence & Lawrence, 2011) (Table 18-2). TABLE 18-2 Summary of Immune Properties of Breast Milk From Newman, J. (1995). How breast milk protects newborns. Scientific American, 273(6), 76-79. Human milk composition and volumes vary according to the stage of lactation. In lactogenesis stage I, beginning at approximately 16 to 18 weeks of pregnancy, the breasts are preparing for milk production by producing colostrum. Colostrum, a clear yellowish fluid, is more concentrated than mature milk and is extremely rich in immunoglobulins. It has higher concentrations of protein and minerals but less fat than mature milk. The high protein level of colostrum facilitates binding of bilirubin, and the laxative action of colostrum promotes early passage of meconium. Colostrum gradually changes to mature milk; this transition is called “the milk coming in” or as lactogenesis stage II. By day 3 to 5 after birth, most women have had this onset of copious milk secretion. Breast milk continues to change in composition for approximately 10 days, when the mature milk is established in stage III of lactogenesis (Lawrence & Lawrence, 2011). • Hand-to-mouth or hand-to-hand movements • Rooting reflex—infant moves toward whatever touches the area around the mouth and attempts to suck
Newborn Nutrition and Feeding
Web Resources
![]()
Recommended Infant Nutrition

Breastfeeding Rates

Benefits of Breastfeeding

Choosing an Infant Feeding Method


Cultural Influences on Infant Feeding
Nutrient Needs

Fluids
Energy
Carbohydrate
Fat
Protein
Vitamins
Minerals
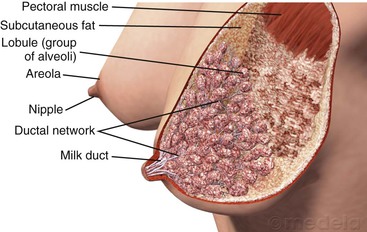
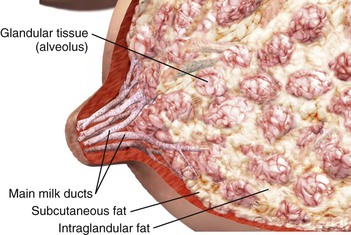
Anatomy and Physiology of Lactation

Anatomy of the Lactating Breast
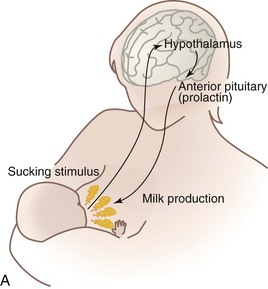
Lactogenesis
Uniqueness of Human Milk
COMPONENT
ACTION
WHITE BLOOD CELLS
B lymphocytes
Give rise to antibodies targeted against specific microbes
Macrophages
Kill microbes outright in baby’s gut, produce lysozyme, and activate other components of the immune system
Neutrophils
May act as phagocytes, ingesting bacteria in baby’s digestive system
T lymphocytes
MOLECULES
Antibodies of secretory immunoglobulin A class
Bind to microbes in infant’s digestive tract and thereby prevent them from passing through walls of the gut into body tissues
B12-binding protein
Reduces amount of vitamin B12, which bacteria need to grow
Bifidus factor
Promotes growth of Lactobacillus bifidus, a harmless bacterium, in infant’s gut; growth of such nonpathogenic bacteria helps crowd out dangerous varieties
Fatty acids
Disrupts membranes surrounding certain viruses and destroys them
Fibronectin
Increases antimicrobial activity of macrophages; helps repair tissues that have been damaged by immune reactions in infant’s gut
Gamma-interferon
Enhances antimicrobial activity of immune cells
Hormones and growth factors
Stimulates infant’s digestive tract to mature more quickly; once the initially “leaky” membranes lining the gut mature, infants become less vulnerable to microorganisms
Lactoferrin
Binds to iron, a mineral many bacteria need to survive; by reducing the available amount of iron, lactoferrin thwarts growth of pathogenic bacteria
Lysozyme
Kills bacteria by disrupting their cell walls
Mucins
Adheres to bacteria and viruses, thus keeping such microorganisms from attaching to mucosal surfaces
Oligosaccharides
Binds to microorganisms and bars them from attaching to mucosal surfaces
Care Management: The Breastfeeding Mother and Infant


Newborn Nutrition and Feeding
Get Clinical Tree app for offline access