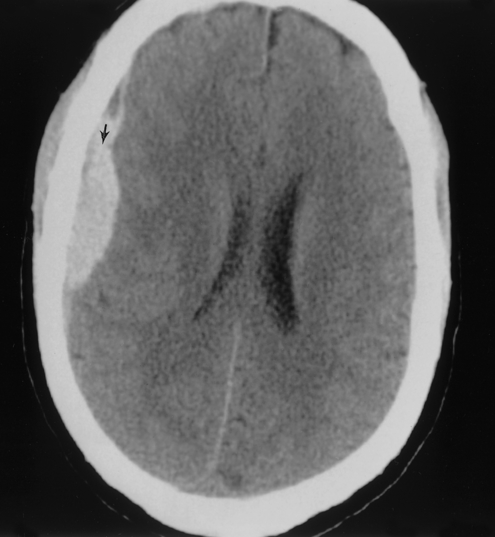
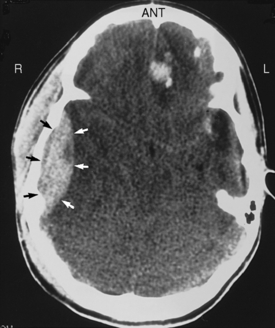
Chapter 24 Subdural hematomas are caused by bleeding from veins that bridge the cortex and dural sinuses. On a computed tomography (CT) scan, the hematoma is crescent-shaped (Fig. 24-1). Subdural hematomas are common in alcoholic patients and victims of head trauma. They may present immediately after trauma or as long as 1 to 2 months later. If the patient has a history of head trauma, always consider the diagnosis of subdural hematoma. If large, expanding, or accompanied by neurologic deficits, treat with surgical evacuation. Epidural hematomas are caused by bleeding from meningeal arteries (classically, the middle meningeal artery). On a CT scan, the hematoma is lenticular in shape (Fig. 24-2). At least 85% of epidural hematomas are associated with a skull fracture (classically, a temporal bone fracture), and many patients have an ipsilateral “blown” pupil (dilated, fixed, nonreactive pupil on the side of the hematoma). The classic history includes head trauma with loss of consciousness, followed by a lucid interval of minutes to hours, then neurologic deterioration. Treatment usually includes surgical evacuation. A subarachnoid hemorrhage is bleeding between the arachnoid and pia mater. The most common cause is trauma, followed by ruptured berry aneurysms. Blood can be seen in the cerebral ventricles and surrounding the brain or brainstem on a CT scan. Classically, the patient describes the “worst headache of my life,” although many die or are unconscious before they reach the hospital. Patients who are awake have signs of meningitis (positive Kernig sign and Brudzinski sign). Remember the association between polycystic kidney disease and berry aneurysms. CT is the test of choice and should be performed before performing lumbar puncture (see question 12). A lumbar puncture shows grossly bloody cerebrospinal fluid (CSF). Intracerebral hemorrhage describes bleeding into the brain parenchyma (Fig. 24-3). The most common cause is hypertension, but it may also be a result of other forms of stroke, trauma, arteriovenous malformations, coagulopathies, or tumors. Two thirds of intracerebral hemorrhages occur in the basal ganglia (especially with hypertension). The patient may come to the hospital with coma or, if awake, contralateral hemiplegia and hemisensory deficits. Blood (which appears white on a CT scan) can be seen in the brain parenchyma and may extend into the ventricles. Surgery is reserved for large, accessible hemorrhages, although usually it is not helpful.
Neurosurgery
2 What causes a subdural hematoma? How do you recognize and treat it?
3 What causes an epidural hematoma? How do you recognize and treat it?
4 Define subarachnoid hemorrhage. What causes it? How is it treated?
5 What causes an intracerebral hemorrhage? How do you recognize and treat it?

![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access




