Neurologic problems
 Just the facts
Just the factsIn this chapter, you’ll learn:
structures of the neurologic system
assessment of patients with problems involving the neurologic system
diagnostic tests for neurologic problems
treatments and nursing interventions for children with neurologic disorders.
Anatomy and physiology
The neurologic system consists of the central nervous system (CNS), the peripheral nervous system, and the autonomic (involuntary) nervous system (ANS). Through complex and coordinated interactions, these three parts integrate all physical, intellectual, and emotional activities. Understanding how each part works is essential to conducting an accurate neurologic assessment.
|
Central nervous system
The CNS is composed of the brain and all its component parts and the spinal cord. Structurally, the CNS is contained within the skull and the vertebral column.
Central command
Integration among all parts of the nervous system enables normal functioning of body parts, both voluntary and involuntary. A person’s perception of himself and his environment, his reactions and interactions with the environment, and his adjustment to development and environmental changes are greatly influenced by the proper integration and functioning of the nervous system.
Brain
The brain, the center of the CNS, collects, integrates, and interprets stimuli and initiates and monitors voluntary and involuntary motor activity.
The incredible expanding brain
Head circumference, which is measured in children up to age 3 years, averages 13″ to 14″ (33 to 35.5 cm) and should be ½″ to 1″ (2 to 3 cm) larger than chest circumference at birth. Fifty percent of brain growth is achieved in the first year of life, 75% by age 3, and 90% by age 6. The brain comprises 12% of body weight at birth, doubles in weight in the first year, and triples by age 5 or 6.
|
Separated at birth
Since the skull protects the brain, the anterior and posterior fontanels are separated at birth to allow for brain expansion. The posterior fontanel closes between ages 4 and 8 weeks, and the anterior fontanel closes between ages 12 and 18 months.
A mass of nerves in a house of bones
Physiologically, the brain is the large, soft mass of nervous tissue housed in the cranium and protected and supported by the meninges and the skull bones. It consists of the:
cerebrum
cerebellum
brain stem.
Other noteworthy figures
Other structures and elements of the brain include the:
neurons
meninges
cerebrospinal fluid (CSF)
ventricles.
Cerebrum
The cerebrum, the largest portion of the brain, is the nerve center that controls sensory and motor activities and intelligence.
The outer layer of the cerebrum, the cerebral cortex, consists of neuron cell bodies (gray matter); the inner layers consist of axons (white matter) and basal ganglia, which control motor coordination and steadiness.
Bridging the hemispheres
A longitudinal fissure divides the cerebrum into two hemispheres connected by a wide band of nerve fibers called the corpus callosum. These hemispheres share information through the
corpus callosum. Because motor impulses descending from the brain cross in the medulla, the right hemisphere controls the left side of the body and the left hemisphere controls the right side of the body.
corpus callosum. Because motor impulses descending from the brain cross in the medulla, the right hemisphere controls the left side of the body and the left hemisphere controls the right side of the body.
Not the piercing kind
Several fissures divide the cerebrum into lobes, each of which is associated with specific functions. (See A look at the lobes.)
Passing the baton
The thalamus, a relay center below the corpus callosum, further organizes cerebral function by transmitting impulses to and from appropriate areas of the cerebrum.
The body’s thermostat
The hypothalamus, which lies beneath the thalamus, is an autonomic center that regulates temperature control, appetite, blood pressure, breathing, sleep patterns, and peripheral nerve discharges that occur with behavioral and emotional expression.
Cerebellum
Beneath the cerebrum, at the base of the brain, is the cerebellum. It’s responsible for smooth-muscle movements, coordinating sensory impulses with muscle activity, and maintaining muscle tone and equilibrium.
Brain stem
The brain stem relays nerve impulses between the spinal cord and other parts of the brain. It houses cell bodies from most of the cranial nerves (CNs) and includes the:
midbrain, which is the reflex center for the third and fourth CNs and mediates pupillary reflexes and eye movements
pons, which helps regulate respirations and mediate chewing, taste, saliva secretion, hearing, and equilibrium
medulla oblongata, which affects cardiac, respiratory, and vasomotor functions.
|
Neurons
The fundamental unit of the nervous system is the neuron, a highly specialized conductor cell that receives and transmits electrochemical nerve impulses. Neurons develop at between 15 and 30 weeks’ gestation.
Delicate and impulsive
Its structure contains delicate, threadlike nerve fibers that extend from the central cell body and transmit signals, or
axons, which carry impulses away from the cell body, and dendrites, which carry impulses to the cell body.
axons, which carry impulses away from the cell body, and dendrites, which carry impulses to the cell body.
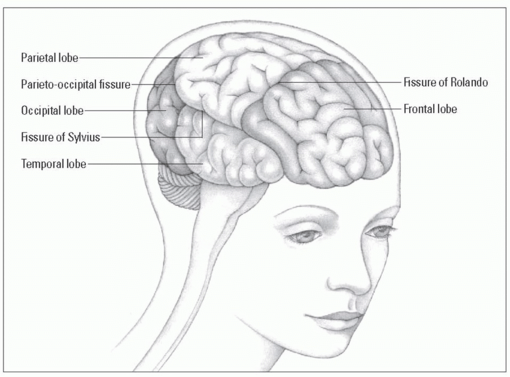
A look at the lobes
Several fissures divide the cerebrum into hemispheres and lobes; each lobe has a specific function.
The great dividers
The fissure of Sylvius (lateral sulcus) separates the temporal lobe from the frontal and parietal lobes. The fissure of Rolando (central sulcus) separates the frontal lobes from the parietal lobe. The parieto-occipital fissure separates the occipital lobe from the two parietal lobes.
Lovely lobes
Each lobe controls specific body functions:
The frontal lobe controls voluntary muscle movements and contains motor areas (including the motor area for speech, or Broca’s area). It’s the center for personality, behavioral, and intellectual functions, such as judgment, memory, and problem solving; for autonomic functions; and for cardiac and emotional responses.
The temporal lobe is the center for taste, hearing, and smell. Also, in the brain’s dominant hemisphere, it interprets spoken language.
The parietal lobe coordinates and interprets sensory information from the opposite side of the body.
The occipital lobe interprets visual stimuli.
|
Meninges
The brain is covered with three thin membranes called meninges:
 The outer membrane is the dura mater, or “hard mother”; it has various folds that separate the brain into compartments.
The outer membrane is the dura mater, or “hard mother”; it has various folds that separate the brain into compartments. The second structure is the arachnoid; it has two layers of fibrous and elastic tissue and, between the layers, a spongy, cobweblike structure containing subarachnoid fluid.
The second structure is the arachnoid; it has two layers of fibrous and elastic tissue and, between the layers, a spongy, cobweblike structure containing subarachnoid fluid. The third structure is the pia mater, or “tender mother,” a very fine membrane that’s rich in minute blood plexuses and follows the brain in all its folds. (See Meningeal layers of the brain.)
The third structure is the pia mater, or “tender mother,” a very fine membrane that’s rich in minute blood plexuses and follows the brain in all its folds. (See Meningeal layers of the brain.)CSF
The ventricles of the brain and the entire subarachnoid space around the brain and spinal cord contain CSF.
Clear liquid with a protein chaser
CSF is a clear liquid containing water and traces of organic materials (especially protein), glucose, and minerals. CSF is formed from blood in capillary networks called choroid plexuses, which are located primarily in the brain’s lateral ventricles. The fluid is eventually reabsorbed into the venous blood through the arachnoid villi, located in dural sinuses on the brain’s surface.
Better than a bubble bath
The brain floats in, and is bathed by, CSF. It acts as a shock absorber and helps reduce forces that jar or shake the brain. CSF is in contact with the entire brain and spinal cord surface as well as the surfaces of the ventricles.
|
Ventricles
The four ventricles are large, CSF-filled cavities within the brain. There are two lateral ventricles, one in each cerebral hemisphere. A third ventricle (located directly above the midbrain of the brainstem) communicates with both the lateral ventricles and the fourth ventricle (located in the posterior brain fossa).
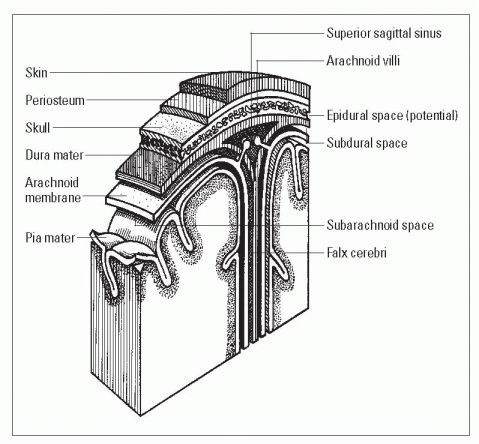
Meningeal layers of the brain
Three primary membranes, or meninges, help protect the CNS: the dura mater, the arachnoid membrane, and the pia mater.
Dura mater
The dura mater is a fibrous membrane that lines the skull and forms folds (reflections) that descend into the brain’s fissures and provide stability. The dural folds include the:
falx cerebri, which lies in the longitudinal fissure and separates the hemispheres of the cerebrum
tentorium cerebelli, which separates the cerebrum from the cerebellum
falx cerebelli, which separates the two cerebellar lobes.
The arachnoid villi (projections of the dura mater into the superior sagittal and transverse sinuses) serve as the exit points for CSF drainage into venous circulation.
Arachnoid membrane
A fragile, fibrous layer with moderate vascularity, the arachnoid membrane lies between the dura mater and the pia mater. Injury to its blood vessels during head trauma, lumbar puncture, or cisternal puncture may cause hemorrhage.
Pia mater
An extremely thin and highly vascular membrane, the pia mater closely covers the brain’s surface and extends into its fissures. It contains minute arteries and veins that supply the brain.
Additional layers
Three layers of space further cushion the brain and spinal cord against injury:
The epidural space (a potential space) lies over the dura mater.
The subdural space lies between the dura mater and the arachnoid membrane and is commonly the site of hemorrhage after head trauma.
The subarachnoid space, which is filled with CSF, lies between the arachnoid membrane and the pia mater.
|
Spinal cord
The spinal cord extends downward from the brain, through the vertebrae, to the level of approximately the second lumbar vertebra. It functions as a conductive pathway to and from the brain. It’s also the reflex center for activities that don’t require
brain control such as deep tendon reflexes (the jerking reaction elicited by tapping with a reflex hammer).
brain control such as deep tendon reflexes (the jerking reaction elicited by tapping with a reflex hammer).
Can you hear me now?
Within the spinal cord, connections are made between incoming and outgoing nerve fibers. Thirty-one pairs of spinal nerves are connected to the cord. The sensory, or ascending, tracts carry sensory impulses up the spinal cord to the brain; the motor, or descending, tracts carry motor impulses down the spinal cord and out to the peripheral nervous system.
Peripheral nervous system
The part of the nervous system outside of the skull and vertebral column is considered the peripheral nervous system. It’s composed of 31 spinal nerves and 12 CNs and is divided into two functional systems: the somatic nervous system and the ANS.
Spinal nerves
Messages transmitted through the spinal cord reach outlying areas through 31 pairs of segmentally arranged spinal nerves attached to the spinal cord. Spinal nerves are numbered according to their point of origin in the cord:
eight cervical nerves—C1 to C8
12 thoracic nerves—T1 to T12
five lumbar nerves—L1 to L5
one coccygeal nerve.
It’s rude to interrupt
After leaving the vertebral column, each spinal nerve separates into rami (branches), distributed peripherally, with extensive but organized overlapping. This overlapping reduces the risk of lost sensory or motor function from interruption of a single spinal nerve.
Cranial nerves
The 12 pairs of CNs transmit motor or sensory messages (or both) primarily between the brain or brain stem and the head and neck. All CNs except the olfactory and optic nerves exit from the midbrain, pons, or medulla oblongata of the brain stem. (See Exit points of the cranial nerves.)
Somatic nervous system
The somatic (voluntary) nervous system is activated by will but can function independently. It’s responsible for all conscious and
higher mental processes as well as subconscious and reflex actions such as shivering.
higher mental processes as well as subconscious and reflex actions such as shivering.
Exit points of the cranial nerves
As this illustration reveals, 10 of the 12 pairs of CNs exit from the brain stem. The remaining two pairs—the olfactory and optic nerves—exit from the forebrain.
|
Autonomic nervous system
The ANS regulates unconscious processes to control involuntary body functions, such as digestion, respiration, and cardiovascular function. It’s usually divided into two antagonistic systems that balance each other’s activities to support homeostasis under normal conditions:
The sympathetic nervous system controls energy expenditure, especially in stressful situations, by releasing adrenergic catecholamines.
The parasympathetic nervous system helps conserve energy by releasing the cholinergic neurohormone acetylcholine.
Neurologic assessment
A complete assessment of the neurologic system includes evaluation of:
mental and emotional status
CN function
sensory function
motor function
reflexes.
Knowledge of the pediatric patient’s physical, psychomotor, and cognitive developmental milestones is an essential assessment tool for detecting significant deviations. For toddlers and preschoolers, make a game of the assessment process when possible. Have older children assist with the assessment.
|
Mini-assessment
Because there isn’t always enough time to completely assess neurologic function, a bedside assessment might focus on level of consciousness (LOC), pupillary response, motor function, reflexes, sensory functions, and vital signs.
Glasgow Coma Scale
The Glasgow Coma Scale (GCS), which assesses eye opening as well as verbal and motor responses, provides a quick, standardized account of neurologic status. A pediatric version of the scale considers the preverbal child. (See Pediatric coma scale.)
Pediatric coma scale
To quickly assess a patient’s LOC and to uncover changes from baseline, use the pediatric coma scale. This assessment tool grades consciousness in relation to eye opening and motor response, and responses to auditory or visual stimuli. A decreased reaction score in one or more categories warns of an impending neurologic crisis. A patient scoring 7 or lower is comatose and probably has severe neurologic damage.
| |||||||||||||||||||||||||||||||||||||||||||||||||||
In this exam, each response receives a numerical value; the final score is the sum total of the values.
A total score of 15 for all three parts is normal.
A score of 7 or lower indicates coma.
A score of 3, the lowest possible score, usually (but not always)
indicates brain death.
Motor function
Motor function is also a good indicator of LOC and can point to central or peripheral nervous system damage.
Myelination mastery
The mastery of gross and fine motor skills is related to the myelination of the nervous system and follows the concept of cephalocaudal-proximodistal development. Cephalocaudal development is the sequence in which the greatest growth always occurs at the head and gradually works its way toward the “tail.” Proximodistal development proceeds from the center toward the extremities.
Reflex rules
Infant activities are primarily driven by reflex but, with myelination and development, a growing child progressively performs complex tasks requiring coordinated movements.
How strong are you?
To evaluate muscle strength, follow these steps:
Have the patient grip your hands and squeeze.
Ask him to push against your palm with his foot.
Compare muscle strength on each side to ensure the results are the same bilaterally.
|
Pupillary response
Brain damage is indicated by a lack of change in pupil size in response to light. Use a flashlight to assess pupillary response at the bedside. While shining the outer edge of the light into the patient’s eye, observe the initial size of the pupil and the speed of the pupil’s response to the light. Compare both eyes to ensure an equal bilateral response.
Diagnostic tests
Several invasive and noninvasive tests are used to diagnose neurologic disorders.
Minimizing emotional trauma
Tests performed to diagnose neurologic disorders can be extremely frightening to a child. Children may have misconceptions related to what will happen and why a test is being performed. Preparing a child helps allay fears and misconceptions and gives him the tools to cope effectively with a frightening experience. The timing of the preparation depends on the age/developmental
level of the child. For the younger child, the preparation should be closer to the occurrence of the procedure, sometimes just prior to. The older child can be given information about a procedure more in advance.
level of the child. For the younger child, the preparation should be closer to the occurrence of the procedure, sometimes just prior to. The older child can be given information about a procedure more in advance.
Before a test is performed, follow these steps:
Tell the child what to expect in simple, age-appropriate terms (what he’ll see, hear, and feel) and explain why the test is being performed.
Be honest about pain or discomfort the child might experience and suggest coping strategies (for example, “Count to 5 and the hurting part will be over”).
Big boys do cry
Tell the child that it’s OK to be afraid, and reassure him that everyone involved is there to help him and keep him safe.
Whenever possible, allow the child to see the equipment (for example, the scanning machine) before the test. Pictures may be used, if necessary.
Encourage the child to ask questions and express his concerns.
Allow the parents to remain with the child during testing whenever possible; when this isn’t possible, tell the child where his parents will be waiting for him.
A job well done
Give the child a “job” to do during the test (for example, “Your job is to hold very still.”) to give him a sense of control.
After the test, praise the child for doing a good job, and encourage him to talk about the test or draw a picture that depicts his experience (to help the child master the experience and put it in perspective).
Specialist to the rescue
Most hospitals have one or more child life specialists who will meet with the child and his parents before a test, explain the procedure, and accompany and support the child and his parents during the test.
CT scan
Computed tomography (CT) scan is indicated when CNS disease is suspected. The scan produces three-dimensional images that can identify congenital abnormalities, fractures, brain tumors, infarction, bleeding, and hematomas as well as provide information about the ventricular system of the brain. CT scan may be done with or without contrast.
Nursing considerations
A child who knows what to expect will be less fearful and more cooperative during a CT scan. To help the child know what to expect, consider these steps:
Explain the procedure to the child. Cooperation is necessary because the patient must lie still during the procedure.
Show the child a picture of the CT machine to help alleviate fears. (It may be necessary to premedicate the patient.)
Tell the child that he may hear a clicking noise as the scanner moves around his head but that the machine won’t touch him.
Explain that the child won’t be able to eat or drink for 4 hours before the scan (depending on age); contrast dye may cause nausea.
Assess the patient for allergy to iodinated dye or shellfish.
Encourage the child to drink fluids after the scan (because dye is excreted by the kidneys).
|
EEG
Electroencephalogram (EEG) is a graphic recording of the electrical activity of the brain. It’s performed to identify and evaluate patients with seizures. Pathologic conditions involving the brain cortex (such as tumors and infarctions) can also be detected. EEG is also used to confirm brain death.
Nursing considerations
After explaining the procedure to the child and his parents:
Reassure the child that he won’t feel anything during the test.
Make sure the child continues to eat and drink before the test because fasting may cause hypoglycemia, which could alter the test results.
Make sure the child doesn’t drink anything with caffeine on the morning of the test because of caffeine’s stimulating effect.
Tell the patient that he needs to remain still during the test; any movement will create interference and alter the EEG recording.
Lumbar puncture
By placing a needle in the subarachnoid space of the spinal column, one can measure the pressure of that space and obtain CSF
for examination and diagnosis. The needle is commonly placed between L3 and L4 (or L4 and L5). This examination may assist in the diagnosis of metastatic brain or spinal cord neoplasm, meningitis, cerebral hemorrhage, and encephalitis.
for examination and diagnosis. The needle is commonly placed between L3 and L4 (or L4 and L5). This examination may assist in the diagnosis of metastatic brain or spinal cord neoplasm, meningitis, cerebral hemorrhage, and encephalitis.
Nursing considerations
The procedure should be explained, and written informed consent should be obtained. In addition, follow these steps:
Apply eutectic mixture of local anesthetics (EMLA) cream to puncture site 30 to 60 minutes before procedure to reduce pain if ordered.
Instruct the child to empty his bladder and bowels before the procedure.
Monitor the child’s vital signs during and after the procedure because sedation is used to complete the procedure.
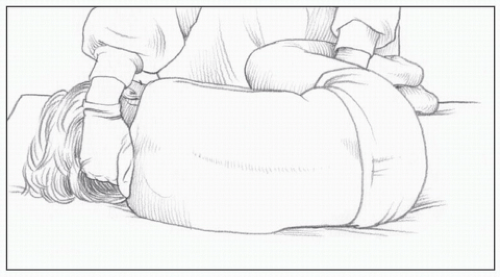
Explain the importance of remaining still throughout the procedure in the side-lying knee-chest position. (See Lumbar puncture positioning, page 220.)
Gently hold even a cooperative child during the procedure to prevent injury from unexpected or involuntary movement.
Maintain, encourage, assess
Keep the child flat for 1 hour after procedure.
Keep the child in a reclining position for up to 12 hours after the procedure to avoid the discomfort of potential postprocedure spinal headache.
Encourage the child to drink increased amounts of fluid with a straw to replace the CSF removed during the puncture. (Drinking with a straw allows the patient to keep his head flat.)
Assess the child for numbness, tingling, and decreased movement of the extremities; pain at the injection site; drainage of blood or CSF at the injection site; and inability to void.
MRI
Magnetic resonance imaging (MRI) is a noninvasive diagnostic procedure that provides valuable information about the body’s anatomy in greater detail than a CT scan does. It doesn’t require exposure to ionizing radiation. MRI is indicated for the evaluation of headache or neurologic signs of CNS lesions; it’s also used to assess neck and back pain as well as lesions of the bones and joints.
Lumbar puncture positioning
When positioning a child for a lumbar puncture, follow these steps:
 Have the child lie on his side at the edge of the bed, with his chin tucked to his chest and his knees drawn up to his abdomen.
Have the child lie on his side at the edge of the bed, with his chin tucked to his chest and his knees drawn up to his abdomen. Make sure the child’s spine is curved and his back is at the edge of the bed (as shown below); this position widens the spaces between the vertebrae, easing insertion of the needle.
Make sure the child’s spine is curved and his back is at the edge of the bed (as shown below); this position widens the spaces between the vertebrae, easing insertion of the needle. To help the child maintain this position, place one of your hands behind his neck; place the other hand behind his knees, and pull gently.
To help the child maintain this position, place one of your hands behind his neck; place the other hand behind his knees, and pull gently. Hold the child firmly in this position throughout the procedure to prevent accidental needle displacement. (Typically, the doctor inserts the needle between the third and fourth lumbar vertebrae.)
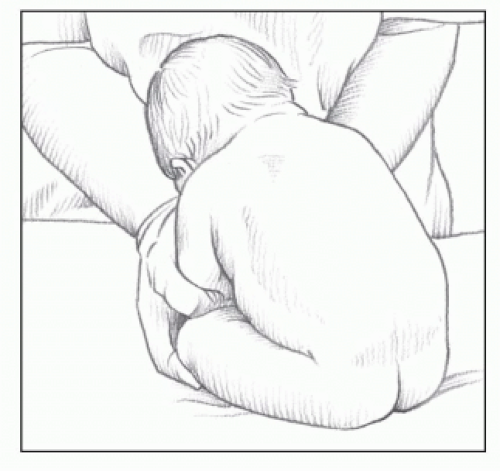
Hold the child firmly in this position throughout the procedure to prevent accidental needle displacement. (Typically, the doctor inserts the needle between the third and fourth lumbar vertebrae.)The sitting position may be used for infants. However, because the flexed position may interfere with the infant’s breathing, monitor his color and respiratory status closely during the procedure.
Nursing considerations
Begin by explaining the procedure to the patient and his family and telling them that there’s no exposure to radiation during MRI. In addition, follow these steps:
Tell the parents that, because no radiation is used, they may read or talk to their child in the imaging room during the procedure.
Inform the parents that young children may need to be sedated because of the need to remain motionless during the procedure.
Tell the child that he may eat or drink as usual before and after the procedure. (No food or fluid restrictions are necessary before MRI, unless sedation is given.)
PET scan
In positron emission tomography (PET) scanning, radioactive chemicals are administered to the patient. These chemicals are used in the normal metabolic process of the particular organ being studied. Positrons emitted from the radioactive chemicals in the organ are sensed by a series of detectors positioned around the patient.
PET scanning can help detect cerebral dysfunction caused by tumors, seizures, head trauma, and some mental illnesses. It’s most commonly used for evaluation of the heart and brain and in many aspects of oncology.
|
Nursing considerations
Keep in mind that many people haven’t heard of PET scanning; the child and his parents may be anxious about what they perceive to be a new procedure. To prepare the child and parents for the procedure, follow these steps:
Explain the procedure to the child and his family.
Explain to the child that an intravenous (I.V.) injection will be inserted and that this is the only “hurting part” of the procedure.
Explain that food or fluids may need to be restricted for 4 hours on the day of the test.
Don’t sedate the child; he may need to perform certain mental activities during a brain PET scan.
After the scan, encourage the child to drink fluids and urinate frequently to aid removal of the radioisotope from the bladder.
Ventricular tap
A ventricular tap may be performed if an infant has unexplained, excessive head growth or a bulging fontanel caused by increased intracranial pressure (ICP), associated with an increased accumulation of CSF that has been confirmed by ultrasound or CT scan.
Going in
When performing a ventricular tap:
The needle is inserted into the subdural space or the ventricle through the open anterior fontanel or the coronal suture.
The fluid is removed slowly to prevent intracranial hemorrhage caused by pressure shifts.
Nursing considerations
Parents are likely to feel anxious when their infant must undergo a procedure that involves pain, discomfort, or stress. The nurse should encourage the parents to ask questions and express concerns.
Explain the procedure to the parents.
Hold the infant’s head securely in the correct position to prevent meningeal laceration.
Number and label the tubes of fluid in the order in which they’re collected.
Maintain the infant in a semi-erect position (an infant seat may be used) to reduce the possibility of further leakage of fluid from the site of the puncture.
Assess the pressure dressing for leakage of fluid and bleeding.
Keep the infant as quiet and comfortable as possible; crying increases ICP.
Procedures and treatments
The care of a child with suspected or diagnosed neurologic problems may involve invasive procedures to monitor or treat the child’s condition.
ICP monitoring
ICP monitoring allows assessment of the pressure exerted by the blood, brain, CSF, and any other space-occupying fluid or mass; increased ICP is defined as pressure sustained at 20 mm Hg or higher.
Look closely …
Assessment of the child with increased ICP requires close observation because the common signs and symptoms may not appear until ICP is significantly elevated, placing the child in grave danger. The subarachnoid bolt and the intraventricular catheter (gold standard of ICP monitoring) are the two major instruments used for monitoring ICP in a child:
The end of the bolt is placed in the subarachnoid space. The top of the bolt is attached to a transducer to conduct a waveform to the monitor.
The catheter is placed in the lateral ventricle or subarachnoid space. (The catheter provides a method for measuring pressure as well as a conduit to drain off extra fluid into a drainage bag.) The drainage bag and the manometer are part of a sterile closed system. (The manometer is used to measure the ICP within the closed system.)
Less invasive
In an infant, ICP monitoring can be performed without penetrating the scalp. In this external method, a photoelectric transducer with a pressure-sensitive membrane is taped to the infant’s anterior fontanel. The transducer responds to pressure at the site and transmits readings to a bedside monitor and recording system.
Sorry, not for everyone
The external method is restricted to infants because pressure readings can be obtained only at the fontanels (the incompletely ossified areas of the skull). ICP monitoring from the fontanels can be inaccurate if the equipment is poorly placed or inconsistently calibrated.
Nursing considerations
Before ICP monitoring is performed, thoroughly explain the procedure to the child and his parents. In addition, follow these steps:
Be thoroughly familiar with the monitoring system being used, and prepare the child and his family for what they can expect after placement of the selected monitoring device.
Explain that the procedure doesn’t hurt the child and that he may have sand bags placed on either side of his head to prevent head movement.
Head of bed is usually elevated 15 to 30 degrees.
Assess whether the child has an allergy to iodine preparations.
Maintain the sterility of the system.
Monitor the child closely for signs of infection.
Monitor the amount of fluid in the drainage bag.
Constantly monitor the child for signs of increased ICP.
Minimize activities that may elevate ICP, such as those that may cause stress, pain, or crying; bright lights, noise, and other environmental stimuli, and vigorous range-of-motion (ROM) exercises. Remember that suctioning and percussion are contraindicated because they acutely elevate ICP. Suctioning may be performed if absolutely necessary by hyperoxygenating the patient with 100% oxygen before the procedure. Vibration may be used instead of percussion because it doesn’t increase ICP.
VP shunt insertion
A ventriculoperitoneal (VP) shunt is implanted in the child with hydrocephalus to prevent excess accumulation of CSF in the ventricles. The tubing diverts the CSF from the ventricles into the peritoneal cavity, where it’s reabsorbed. The procedure is performed under general anesthesia.
Nursing considerations
Young children may have misconceptions about procedures involving general anesthesia. When explaining this procedure (and all procedures involving general anesthesia), make sure the child understands that he will be given “a special medicine” to make sure he doesn’t feel anything during the procedure.
|
A special sleep
Rather than telling a child he’ll be asleep (which may make him afraid to go to sleep at night or nap time or cause him to worry that he’ll wake up during the procedure), tell him, “The medicine gives you a special kind of sleep that isn’t like sleeping at night or nap time.”
Monitor and measure
In addition to preparing the child for the procedure, follow these care measures:
Preoperatively
Frequent neurologic assessments:
Monitor the patient for signs of increased ICP.
Measure head circumference daily at the occipital frontal circumference; place the tape measure just above the top of the ears, around the midforehead, and around the most prominent part of the occiput.
Gently palpate fontanels and suture lines for signs of bulging, tenseness, and separation, which may indicate increased ICP or increasing ventricular size.
Postoperatively
Continue frequent neurologic assessments:
Monitor the patient for pain, and administer pain medications as ordered.
Check orders regarding allowable activities.
Observe the child for signs of increased ICP, which may indicate an obstructed shunt.
Monitor the child for abdominal distention, which may indicate distal catheter displacement.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access