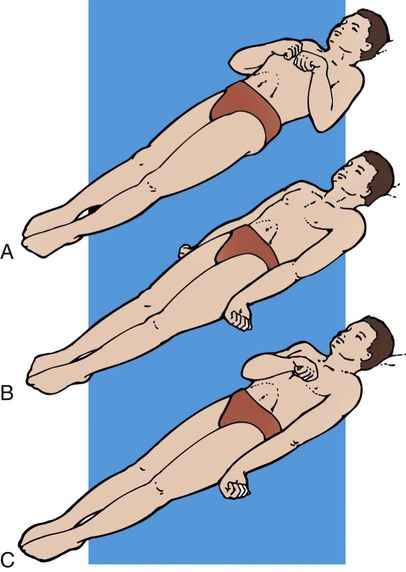
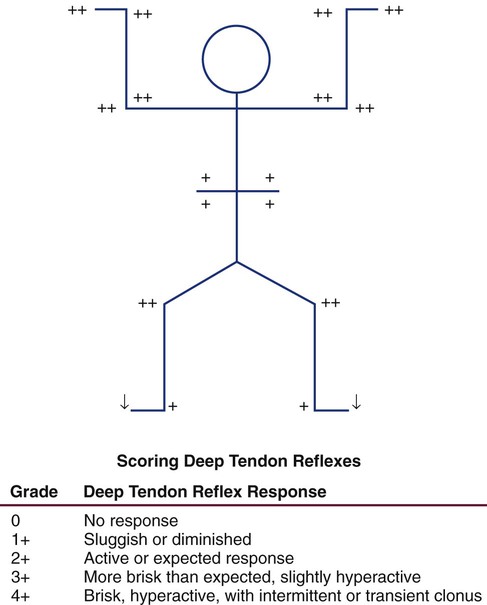
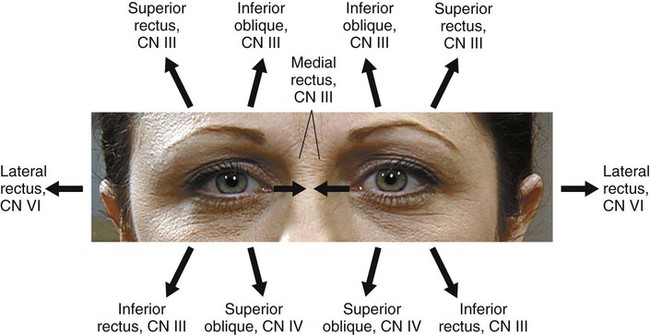
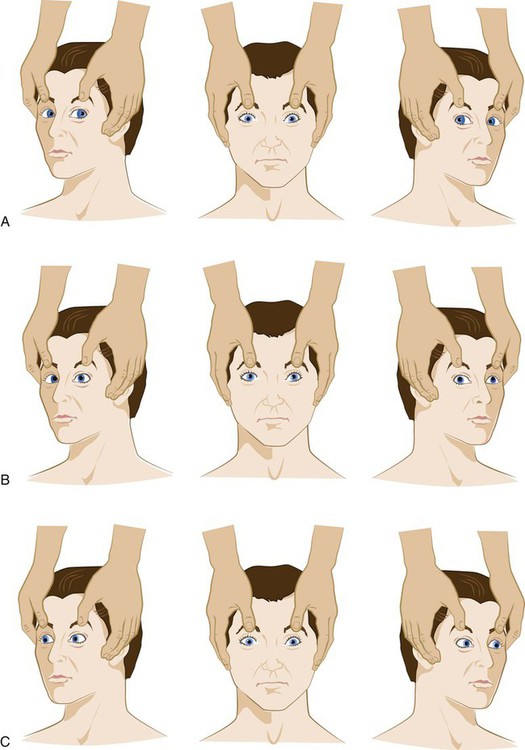
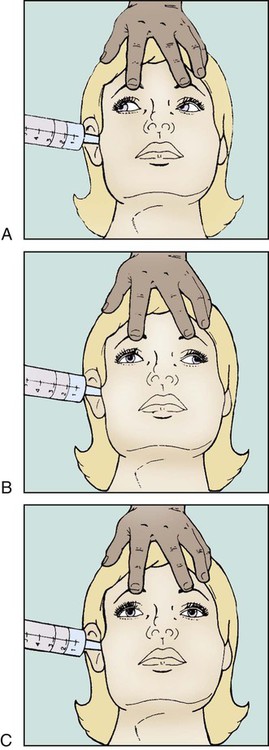
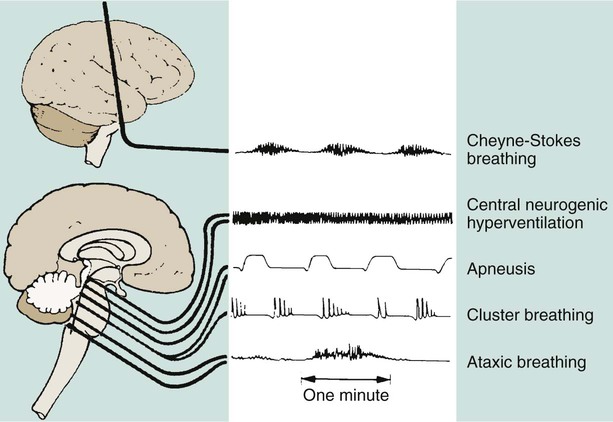
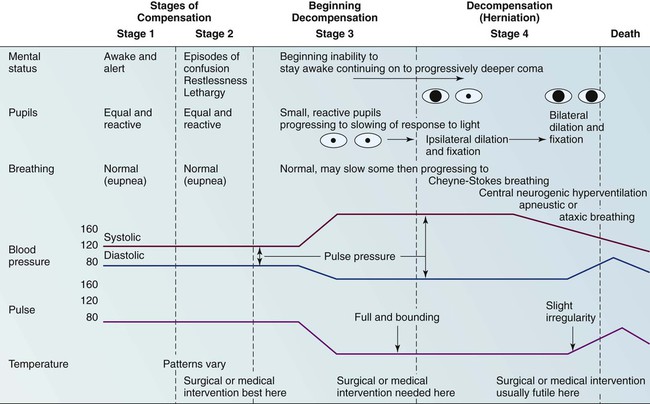
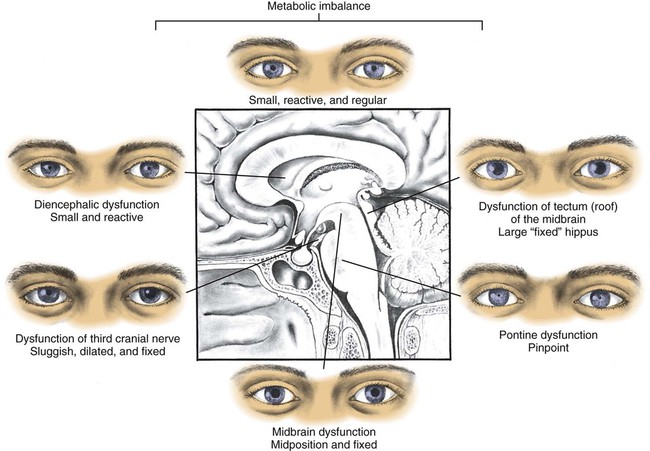
Chapter 23 A thorough clinical assessment of the critically ill patient with neurologic dysfunction is imperative for the early identification and treatment of a neurologic disorder and serves as source of comparison for ongoing assessments of the patient. The most important finding in any neurologic assessment is change, which should be reported promptly. Early identification of neurologic deterioration is vital to preventing secondary brain injury.1 Other medical conditions, as well as the administration of medications, can affect the clinical assessment and should be taken into consideration when the results of the neurologic examination are abnormal. Common to all neurologic assessments is the need to obtain a comprehensive history of events preceding hospitalization. An adequate neurologic history includes information about clinical manifestations, associated complaints, precipitating factors, progression, and familial occurrences (Box 23-1).2 The ideal historian for recounting this information is someone who is able to provide a detailed description and chronology of events. If the patient is incapable of serving as the historian, family members or significant others who have contact with the patient on a daily basis should be contacted as soon as possible. Through history taking, the caregiver gains valuable information that directs him or her to focus on certain aspects of the patient’s clinical assessment.3 Five major components make up the neurologic evaluation of the critically ill patient: 1) level of consciousness, 2) motor function, 3) pupillary function, 4) respiratory function, and 5) vital signs. A complete neurologic examination requires assessment of all five components.3,4 Assessment of the level of consciousness is the most important aspect of the neurologic examination. In most situations, a patient’s level of consciousness deteriorates before any other neurologic changes are noticed. These deteriorations often are subtle and must be monitored carefully. Assessment of level of consciousness focuses on two areas: 1) evaluation of arousal or alertness and 2) appraisal of content of consciousness or awareness.3,5 Although universally accepted definitions for various levels of consciousness do not exist, the categories outlined in Box 23-2 are often used to describe the patient’s level of consciousness.3,4,6 Assessment of the arousal component of consciousness is an evaluation of the reticular activating system and its connection to the thalamus and the cerebral cortex. Arousal is the lowest level of consciousness, and observation centers on the patient’s ability to respond to verbal or noxious stimuli in an appropriate manner.5 To stimulate the patient, the nurse should begin with verbal stimuli in a normal tone. If the patient does not respond, the nurse should increase the stimuli by talking very loudly to the patient. If the patient still does not respond, the nurse should further increase the stimuli by shaking the patient. Noxious stimuli should follow if previous attempts to arouse the patient are unsuccessful. To assess arousal, central stimulation techniques should be used (Box 23-3).3 Content of consciousness is a higher-level function, and appraisal of awareness is concerned with assessment of the patient’s orientation to person, place, time, and situation.5 Assessment of content of consciousness requires the patient to give appropriate answers to a variety of questions. Changes in the patient’s answers that indicate increasing degrees of confusion and disorientation may be the first sign of neurologic deterioration.2,3 The most widely recognized tool for assessing level of consciousness tool is the Glasgow Coma Scale (GCS).7 This scored scale is based on evaluation of three categories: 1) eye opening, 2) verbal response, and 3) best motor response (Table 23-1). The highest possible score on the GCS is 15, and the lowest score is 3. A score of 7 or less on the GCS usually indicates coma. Originally, the scoring system was developed to assist in general communication concerning the severity of neurologic injury. Recently, however, the usefulness of the GCS has been called into question, particularly because of poor inter-rater reliability.8 Several points should be kept in mind when the GCS is used for serial assessment. It provides data about level of consciousness only, and it never should be considered a complete neurologic examination. Additionally, it is not a sensitive tool for evaluation of an altered sensorium, and it does not account for possible aphasia or mechanical intubation. It is also a poor indicator of lateralization of neurologic deterioration.9 Lateralization involves decreasing motor response on one side or unilateral changes in pupillary reaction. TABLE 23-1 Assessment of motor function focuses on muscle size and tone and on an estimation of muscle strength. Each side should be assessed individually and then compared with the other.3,10 Initially, muscles should be inspected for size and shape. The presence of atrophy is noted. Muscle tone is assessed by evaluating opposition to passive movement. The patient is instructed to relax the extremity while the nurse performs passive range-of-motion movements and evaluates the degree of resistance. Muscle tone is appraised for signs of flaccidity (no resistance), hypotonia (little resistance), hypertonia (increased resistance), spasticity, or rigidity.6 Having the patient perform a number of movements against resistance assesses muscle strength. The strength of the movement is then graded on a six-point scale (Box 23-4). The patient is asked to extend both arms with the palms turned upward and to hold that position with the eyes closed. If the patient has a weaker side, that arm will drift downward and pronate. The lower extremities are tested by asking the patient to push and pull the feet against resistance or to elevate the legs.6 If the patient is incapable of comprehending and following a simple command, noxious stimuli are necessary to determine motor responses. The stimulus is applied to each extremity separately to allow evaluation of individual extremity function. Peripheral stimulation is used to assess motor function (see Box 23-2).3,4 Motor responses elicited by noxious stimuli are interpreted differently from those elicited by voluntary demonstration.3 These responses may be classified as shown in Box 23-5. Abnormal flexion also is known as decorticate posturing (Fig. 23-1A). In response to painful stimuli, the upper extremities exhibit flexion of the arm, wrist, and fingers, with adduction of the limb. The lower extremity exhibits extension, internal rotation, and plantar flexion. Abnormal flexion occurs with lesions above the midbrain, located in the region of the thalamus or cerebral hemispheres. Abnormal extension also is known as decerebrate rigidity or posturing (see Fig. 23-1B); when the patient is stimulated, teeth clench, and the arms are stiffly extended, adducted, and hyperpronated. The legs are stiffly extended, with plantar flexion of the feet. Abnormal extension occurs with lesions in the area of the brainstem.10 Because abnormal flexion and extension appear similar in the lower extremities, the upper extremities are used to determine the presence of these abnormal movements. It is possible for the patient to exhibit abnormal flexion on one side of the body and extension on the other (see Fig. 23-1C).3,4 Outcome studies indicate abnormal flexion, which has a less serious prognosis than does extension, or decerebrate posturing.10 Onset of posturing or a change from abnormal flexion to abnormal extension requires immediate physician notification. Deep tendon reflexes (DTRs) are usually evaluated by a physician when a complete neurologic evaluation is performed. DTRs are tested by tapping the appropriate tendon using a reflex or percussion hammer. The muscle needs to be relaxed and the joint at midposition for reflex testing to be accurate.5 The four reflexes tested are: 1) the Achilles (ankle jerk), 2) the quadriceps (knee jerk), 3) the biceps, and 4) the triceps. DTRs are graded on a scale from 0 (absent) to 4 (hyperactive). A DTR grade of 2 is normal (Fig. 23-2). Hyper-reflexia is associated with upper motor neuron interruption, and areflexia is associated with lesions of the lower motor neurons.6 Superficial reflexes are normal if present and abnormal if absent. Superficial reflexes are tested by stimulating cutaneous receptors of the skin, cornea, or mucous membrane. Stroking, scratching, or touching can be used as the stimulus (Table 23-2). The corneal reflex is present if the eyelids quickly close when the cornea is lightly stroked with a wisp of cotton. An alternative approach is to drop a small amount of water or saline onto the cornea.4,6 The pathway for the corneal reflex is formed by the trigeminal cranial nerve V (CN V), the facial nerve (CN VII), and the pons. The pharyngeal reflex is present if retching or gagging occurs with stimulation of the back of the pharynx.3,4,6 TABLE 23-2 From Barker E. Neuroscience Nursing: A Spectrum of Care. ed 3. St. Louis: Mosby; 2008. The presence of pathologic reflexes is an abnormal neurologic finding.11 The grasp reflex is present when tactile stimulation of the palm of the hand produces a grasp response that is not a conscious voluntary act. The grasp reflex is a primitive reflex that normally disappears with maturational development. Presence of the grasp reflex in the adult indicates cortical damage. Babinski reflex is a pathologic sign in any individual older than 2 years. The presence of this reflex is tested by slow, deliberate stroking of the lateral half of the sole of the foot. Sustained extensor response of the big toe is indicative of a positive Babinski’s reflex. This response is sometimes accompanied by the fanning out of the other four toes. Flexor response of all the toes in response to the same stimuli is a normal finding and indicates absence of Babinski reflex (Fig. 23-3). Babinski reflex is a significant neurologic finding because it indicates an upper motor neuron lesion in the brain, brainstem, or spinal cord.11 The disease may be degenerative, neoplastic, inflammatory, vascular, or posttraumatic. Babinski reflex may also become positive during transtentorial herniation.3 Pupillary function is an extension of the autonomic nervous system. Parasympathetic control of the pupil occurs through innervation of the oculomotor nerve (CN III), which exits from the brainstem in the midbrain area. When the parasympathetic fibers are stimulated, the pupil constricts. Sympathetic control originates in the hypothalamus and travels down the entire length of the brainstem. When the sympathetic fibers are stimulated, the pupil dilates. Pupillary changes provide a valuable assessment tool because of pathway locations. The oculomotor nerve lies at the junction of the midbrain and the tentorial notch. Any increase of pressure that exerts force down through the tentorial notch compresses the oculomotor nerve. Oculomotor nerve compression results in a dilated, nonreactive pupil. Sympathetic pathway disruption occurs with involvement in the brainstem. Loss of sympathetic control leads to pinpoint, nonreactive pupils. Control of eye movements occurs with interaction of three cranial nerves: 1) oculomotor (CN III), 2) trochlear (CN IV), and 3) abducens (CN VI). The pathways for these cranial nerves provide integrated function through the internuclear pathway of the medial longitudinal fasciculus (MLF) located in the brainstem. The MLF provides coordination of eye movements with the vestibular nerve (CN VIII) and the reticular formation.12 Pupil diameter should be documented in millimeters (mm) with the use of a pupil gauge to reduce the subjectivity of description. Most people have pupils of equal size, between 2 and 5 mm. A discrepancy up to 1 mm between the two pupils is normal; it is called anisocoria and occurs in 16% to 17% of the human population.13 Change or inequality in pupil size, especially in patients who previously have not shown this discrepancy, is a significant neurologic sign. It may indicate impending danger of herniation and should be reported immediately. With the location of CN III at the notch of the tentorium, pupil size and reactivity play a key role in the physical assessment of intracranial pressure (ICP) changes and herniation syndromes. In addition to CN III compression, changes in pupil size occur for other reasons. Large pupils can result from the instillation of cycloplegic agents such as atropine or scopolamine or can indicate extreme stress. Extremely small pupils can indicate opioid overdose, lower brainstem compression, or bilateral damage to the pons.13,14 Pupil shape is included in the assessment of pupils. Although the pupil is normally round, an irregularly shaped or oval pupil may be observed in patients who have undergone eye surgery. Initial stages of CN III compression from elevated ICP can cause the pupil to have an oval shape.3,13 The pupillary light reflex depends on optic nerve (CN II) and oculomotor nerve (CN III) function (Fig. 23-4).6,13 The technique for evaluation of the pupillary light response involves use of a narrow-beamed bright light shined into the pupil from the outer canthus of the eye. If the light is shined directly onto the pupil, glare or reflection of the light may prevent the assessor’s proper visualization. Pupillary reaction to light is identified as brisk, sluggish, or nonreactive or fixed.3 Each pupil should be evaluated for direct light response and for consensual response. The consensual pupillary response is constriction in response to a light shined into the opposite eye. This reflex occurs as a result of the crossing of nerve fibers at the optic chiasm.3 Evaluation of consensual response is necessary to rule out optic nerve dysfunction as a cause for lack of a direct light reflex. Because the optic nerve is the afferent pathway for the light reflex, shining a light into a blind eye produces neither a direct light response in that eye nor a consensual response in the opposite eye. A consensual response in the blind eye produced by shining a light into the opposite eye demonstrates an intact oculomotor nerve. Oculomotor compression associated with transtentorial herniation affects the direct light response and the consensual response in the affected pupil.3,4,12,13 In the conscious patient, the function of the three cranial nerves of the eye and their MLF innervation can be assessed by asking the patient to follow a finger through the full range of eye motion. If the eyes move together into all six fields, extraocular movements are intact (Fig. 23-5).3,12 In the unconscious patient, assessment of ocular function and innervation of the MLF is performed by eliciting the doll’s eyes reflex. If the patient is unconscious as a result of trauma, the nurse must ascertain the absence of cervical injury before performing this examination. To assess the oculocephalic reflex, the nurse holds the patient’s eyelids open and briskly turns the head to one side while observing the eye movement and then briskly turns the head to the other side and observes the eye movement again. If the eye movement deviates to the opposite direction in which the head is turned, the doll’s eyes reflex is present, and the oculocephalic reflex arc is intact (Fig. 23-6A). If the oculocephalic reflex arc is not intact, the reflex is absent. This lack of response, in which the eyes remain midline and move with the head, indicates significant brainstem injury (see Fig. 23-6C). The reflex may also be absent in severe metabolic coma. An abnormal oculocephalic reflex is present when the eyes rove or move in opposite directions from each other (see Fig. 23-6B). Abnormal oculocephalic reflex indicates some degree of brainstem injury.3,4,12 The oculovestibular reflex is performed by a physician, often as one of the final clinical assessments of brainstem function. After confirmation that the tympanic membrane is intact, the patient’s head is raised to a 30-degree angle, and 20 to 100 milliliters (mL) of ice water is injected into the external auditory canal. The normal eye movement response is a conjugate, slow, tonic nystagmus, deviating toward the irrigated ear and lasting 30 to 120 seconds. This response indicates brainstem integrity. Rapid nystagmus returns the eye position back to the midline only in a conscious patient with cortical functioning (Fig. 23-7).3,10 An abnormal response is disconjugate eye movement, which indicates a brainstem lesion, or no response, which indicates little or no brainstem function. The oculovestibular reflex may be temporarily absent in reversible metabolic encephalopathy.8 This test is an extremely noxious stimulation and may produce a decorticate or decerebrate posturing response in a comatose patient. In the conscious patient, this procedure may produce nausea, vomiting, or dizziness.3,12,14 The activity of respiration is a highly integrated function that receives input from the cerebrum, brainstem, and metabolic mechanisms. In clinical assessment, correlations exist among altered levels of consciousness, the level of brain or brainstem injury, and the patient’s respiratory pattern. Under the influence of the cerebral cortex and the diencephalon, three brainstem centers control respirations. The lowest center, the medullary respiratory center, sends impulses through the vagus nerve to innervate muscles of inspiration and expiration. The apneustic and pneumotaxic centers of the pons are responsible for the length of inspiration and expiration and the underlying respiratory rate.3,4,10 Changes in respiratory patterns assist in identifying the level of brainstem dysfunction or injury (Fig. 23-8 and Table 23-3). Evaluation of the respiratory pattern must include assessment of the effectiveness of gas exchange in maintaining adequate oxygen and carbon dioxide levels. Hypoventilation is not uncommon in the patient with an altered level of consciousness. Alterations in oxygenation or carbon dioxide levels can result in further neurologic dysfunction. ICP increases with hypoxemia or hypercapnia.3,4,10 TABLE 23-3 Assessment of vital signs focuses on two areas: 1) evaluation of blood pressure and 2) observation of heart rate and rhythm. As a result of the brain and brainstem influences on cardiac, respiratory, and body temperature functions, changes in vital signs could be signs of deterioration in neurologic status.3,4 A common manifestation of intracranial injury is systemic hypertension. Cerebral autoregulation, responsible for the control of cerebral blood flow (CBF), frequently is lost with any type of intracranial injury. After cerebral injury, the body often is in a hyperdynamic state (increased heart rate, blood pressure, and cardiac output) as part of a compensatory response. With the loss of autoregulation as blood pressure increases, CBF and cerebral blood volume increase, and ICP therefore increases. Control of systemic hypertension is necessary to stop this cycle, but caution must be exercised. The mean arterial pressure must be maintained at a level sufficient to produce adequate CBF in the presence of elevated ICP. Attention must also be paid to the pulse pressure because widening of this value may occur in the late stages of intracranial hypertension.15,16 The medulla and the vagus nerve provide parasympathetic control to the heart. When stimulated, this lower brainstem system produces bradycardia. Sympathetic stimulation increases the rate and contractility. Various intracranial pathologies and abrupt ICP changes can produce bradycardia, premature ventricular contractions (PVCs), QT changes, and myocardial damage.17 Cushing reflex, also known as Cushing triad or Cushing phenomena, is a set of three clinical manifestations (systolic hypertension, bradycardia, and abnormal respirations) related to pressure on the medullary area of the brainstem. These signs may occur in response to intracranial hypertension or a herniation syndrome. The appearance of Cushing reflex is a late finding that may be absent in patients with severe neurologic deterioration. Attention should be paid to alteration in each component of the triad and intervention initiated accordingly.18 A neurologic assessment should be organized, thorough, and simple so that it can be performed accurately and easily at each assessment point.3 A complete neurologic assessment should cover all major areas of neurologic control. Any abnormalities identified can then be further evaluated and investigated in a more focused and rapid manner. Findings should always be evaluated with respect to those of previous examinations. One critical assessment point is handoff between nurses who are caring for the patient. It is extremely important that the off-going nurse perform a neurologic assessment with the on-coming nurse. This ensures reliability of the assessment and decreases variability between caregivers. An example of a rapid neurologic assessment that can be performed during handoff of a conscious patient with known or potential neurologic deficit is outlined in Box 23-6. This assessment, which usually takes less than 4 minutes, is meant to provide a starting point. If any neurologic deficit is identified that is new or different from that of the last assessment, more detailed attention must be focused on that abnormality. In the assessment of the unconscious patient (Box 23-7), initial efforts are directed at achieving maximal arousal of the patient. Calling the patient’s name, patting the chest, or shaking a shoulder accomplishes this task. After the patient has been stimulated, the examiner can proceed with the neurologic evaluation. As in the assessment of the conscious patient, if any abnormalities or changes from previous assessment are noticed, further investigation must occur. This assessment takes 3 to 4 minutes. Assessment of the patient for signs of increasing ICP is an important responsibility of the critical care nurse. Increasing ICP can be identified by changes in level of consciousness, pupillary reaction, motor response, vital signs, and respiratory patterns (Fig. 23-9).10,19
Neurologic Clinical Assessment and Diagnostic Procedures
Clinical Assessment
History
Physical Examination
Level of Consciousness
Evaluation of Arousal
Appraisal of Awareness
Glasgow Coma Scale
CATEGORY
SCORE
RESPONSE
Eye Opening
4
Spontaneous: Eyes open spontaneously without stimulation
3
To speech: Eyes open with verbal stimulation but not necessarily to command
2
To pain: Eyes open with noxious stimuli
1
None: No eye opening regardless of stimulation
Verbal Response
5
Oriented: Accurate information about person, place, time, reason for hospitalization, and personal data
4
Confused: Answers not appropriate to question, but use of language is correct
3
Inappropriate words: Disorganized, random speech, no sustained conversation
2
Incomprehensible sounds: Moans, groans, and incomprehensible mumbles
1
None: No verbalization despite stimulation
Best Motor Response
6
Obeys commands: Performs simple tasks on command; able to repeat performance
5
Localizes to pain: Organized attempt to localize and remove painful stimuli
4
Withdraws from pain: Withdraws extremity from source of painful stimuli
3
Abnormal flexion: Decorticate posturing spontaneously or in response to noxious stimuli
2
Extension: Decerebrate posturing spontaneously or in response to noxious stimuli
1
None: No response to noxious stimuli; flaccid
Motor Function
Evaluation of Muscle Size and Tone
Estimation of Muscle Strength
Abnormal Motor Responses
Evaluation of Reflexes
REFLEX
NERVES INVOLVED
NORMAL REACTION
Corneal
CN V and VII
Prompt closure of both eyelids when cornea touched with wisp of cotton
Pharyngeal
CN IX and X
Gagging response to pharyngeal stimulation
Abdominal
Epigastric (T6-T9); midabdominal (T9-T11); hypogastric (T11-L1)
Contraction of abdominal muscle when stroked, so that a brief, brisk movement of umbilicus toward stimulus occurs
Cremasteric
L1, L2
Elevation of testicle when inner aspect of thigh stroked
Anal
Contraction of anal ring as perineum is stroked or scratched
Bulbocutaneous
S4, S5
Anocutaneous
S5
Plantar
L5, S1
Flexion of toes from stimulation of sole of foot
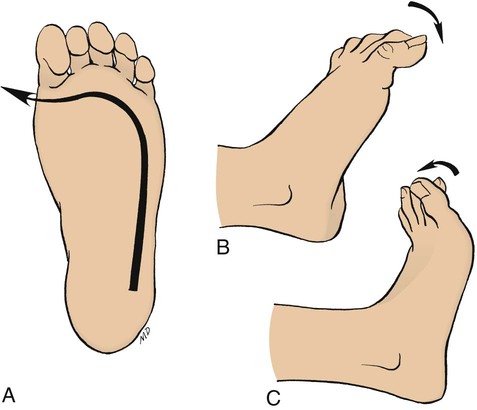
A, Test maneuver: using a blunt point, scratch the sole of the foot as shown. B, Normal response (absence of Babinski response) is plantiflexion of the toes. C, Abnormal response (presence of Babinski’s response) is dorsiflexion of the big toe and often a fanning of the other toes. (From Black JM, Hawks JH. Medical-Surgical Nursing: Clinical Management for Positive Outcomes. 8th ed. Philadelphia: Saunders; 2009.)
Pupillary Function
Estimation of Pupil Size and Shape
Evaluation of Pupillary Reaction to Light
Assessment of Eye Movement
Respiratory Function
Observation of Respiratory Pattern
PATTERN OF RESPIRATION
DESCRIPTION OF PATTERN
SIGNIFICANCE
Cheyne-Stokes breathing
Rhythmic crescendo and decrescendo of rate and depth of respiration; includes brief periods of apnea
Usually seen with bilateral deep cerebral lesions or some cerebellar lesions
Central neurogenic hyperventilation
Very deep, very rapid respirations with no apneic periods
Usually seen with lesions of the midbrain and upper pons
Apneustic breathing
Prolonged inspiratory and/or expiratory pause of 2-3 seconds
Usually seen in lesions of the middle to lower pons
Cluster breathing
Clusters of irregular, gasping respirations separated by long periods of apnea
Usually seen in lesions of the lower pons or upper medulla
Ataxic respirations
Irregular, random pattern of deep and shallow respirations with irregular apneic periods
Usually seen in lesions of the medulla
Vital Signs
Evaluation of Blood Pressure
Observation of Heart Rate and Rhythm
Cushing Reflex.
Rapid Neurologic Assessment
The Conscious Patient
The Unconscious Patient
Neurologic Changes Associated with Intracranial Hypertension
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Neurologic Clinical Assessment and Diagnostic Procedures
Get Clinical Tree app for offline access