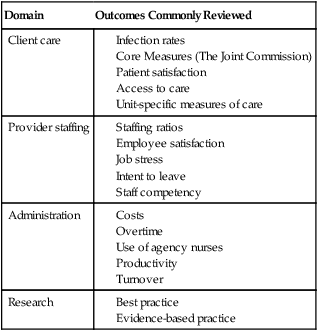
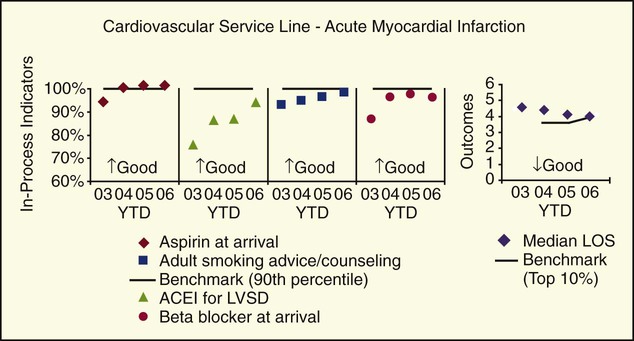
1. Relate the principles of performance improvement to the monitoring of patient care data. 2. Discuss routine information monitored by nurse managers. 3. Identify methods of analyzing data in health care. 4. Identify outcomes for various areas of nursing responsibility. 5. Differentiate between data and information. 6. Analyze the role of the nurse manager in assisting unit staff to deal with the information provided by the data collected. Factual information (as measurements or statistics) used as a basis for reasoning or decision making Nursing data fall into four domains (Table 12-1). Nurses need data to provide information about client care, provider staffing, administration of care and the organization, and knowledge-based research for evidence-based practice. Collecting specific sets of data related to each of these domains give nurses information about practice and its effectiveness. Table 12-1 Adapted from Huber, D. (2006). Leadership and nursing care management. Philadelphia, PA: Elsevier. P. 273. The patient care outcomes that are routinely collected vary from unit to unit and from institution to institution. There are nationwide measures, such as the National Patient Safety Goals and the Core Measures of The Joint Commission. These were discussed in Chapter 10. All institutions also collect information on infection rates. This information is required by both state and federal regulating agencies. Sometimes these measures are intertwined; one such example is the Core Measure of Pneumonia, which is also an infectious process. Infectious disease evidence shows two actions that result in lower mortality: administering antibiotics within 4 hours of admission and acting on the information obtained from blood cultures. By reviewing the levels of performance on these two “in-process” measures of caring for a patient with pneumonia (administering antibiotics within 4 hours of arrival and acting on information obtained from blood cultures), an organization may be able to improve their performance on the outcome for the care of the pneumonia patient. In reviewing Figure 12-1, look at the performance of a particular hospital in the Core Measures for a patient with acute myocardial infarction. If you review the levels of performance for angiotensin-converting enzyme inhibitors (ACEIs) for left ventricular systolic dysfunction, you will see an improvement in performance from 2003 to 2006. You will also see improved performance for two of the other in-process measures for care of the patient with acute myocardial infarction: adult smoking advice/counseling and aspirin on arrival. Processes were created by the hospital based on performance in 2003 to make it easier to give aspirin on arrival, to give β-blockers, and to give smoking advice. This change in process led to the result of better performance in the following years. Also, it led to a lower length of stay for these patients. Also, many hospitals will have organization- and unit-specific dashboards that visually display current levels of performance on key indicators. For a further discussion of dashboards, go to Chapter 10. Common satisfaction data results in information about: • Accessibility—both physical access and financial access to care • Communication skills—of the physicians, nurses, physician assistants, nurse practitioners, and others involved in direct patient care • Personality and demeanor—of the same group • Quality of medical-care processes—as provided directly to the patient • Care continuity—regarding the handoffs made provider-to-provider, as well as across time • Quality of health care facilities—in terms of having the appropriate equipment, supplies, and peripheral resources available • Efficiency of office staff—in handling scheduling, billing, etc. • Greater patient trust and acceptance with treatment plans • Increasing buy-in for treatment plans more quickly, making best use of scarce physician time • Increasing trust, which allows caregivers to discover more factors that may affect the care needs of the patient • Enhancing patient involvement in their own care through preventative measures, corrective measures, and so forth • Driving efficiency into the organization by focusing on what works well with patients and eliminating what does not work well • Cross-over trust is enhanced. For instance, a good experience in scheduling appointments can cross over into a better experience with the care provider. In addition, a good experience with the patient’s primary care physician can cross over into a more positive experience with specialists to whom the primary care physician has referred the patient. • Increased internal support for other quality improvement efforts, such as timeliness improvement, care process improvement, etc.
Monitoring Outcomes and Use of Data for Improvement
FOUR DOMAINS OF NURSING DATA
Domain
Outcomes Commonly Reviewed
Client care
Provider staffing
Administration
Research
THE CORE MEASURES
PATIENT SATISFACTION REPORTS
DRIVING FORCES FOR INCREASING PATIENT SATISFACTION
Clinical Benefits
Operational Benefits
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Monitoring Outcomes and Use of Data for Improvement
Get Clinical Tree app for offline access
