Modeling and Role-Modeling Theory in Nursing Practice
Margaret E. Erickson
Modeling and Role-Modeling is based on the philosophy that all humans have the desire to live healthy, happy lives, to find meaning and purpose in their lives, and to become the most that they can be. This holds true across the lifespan. When we use strategies that focus on the strengths of our clients, help them become more fully alive (even as they approach physical death), and to live their lives to the fullest, then we are truly helping them grow, heal, and transcend. We help them discover the essence of their being, to find or reclaim their soul.
History and Background
The Modeling and Role-Modeling (MRM) paradigm, conceived by Helen Erickson in the late 1950s, was an outcome of her exposure to the work of her father-in-law, Milton H. Erickson, coupled with her own experiences as a professional nurse. During the late 1940s and the 1950s, M. Erickson, MD, developed an international reputation for his unorthodox methods, views on human nature, and clinical results (Rossi & O’Ryan, 1985, 1992; Rossi, O’Ryan, & Sharp, 1983). H. Erickson states that she repeatedly asked him to tell her “what to do and how to do it” (H. Erickson, personal communication, February 2000). She hoped for protocols, treatment recommendations, and quick fixes, but instead she was told that she must model the client’s world and plan strategies within that context. M. Erickson, MD, advised that each human has a unique view of the world and needs to maintain his or her role in unique ways and that the practice of health care professionals was to help clients succeed in living quality lives and growing to the maximum of their potential.
Over a period of approximately 16 years, H. Erickson came to understand the wisdom of her father-in-law’s advice. As a result, by the mid-1970s, she hadconceived and developed a practice framework that she called Modeling and Role-Modeling. She began to label and articulate the theoretical components during her baccalaureate completion and master’s study at the University of Michigan (1972-1976). Refinement of the concepts and their linkages continued as she worked with and was challenged by two colleagues, Mary Ann Swain and Evelyn Tomlin.
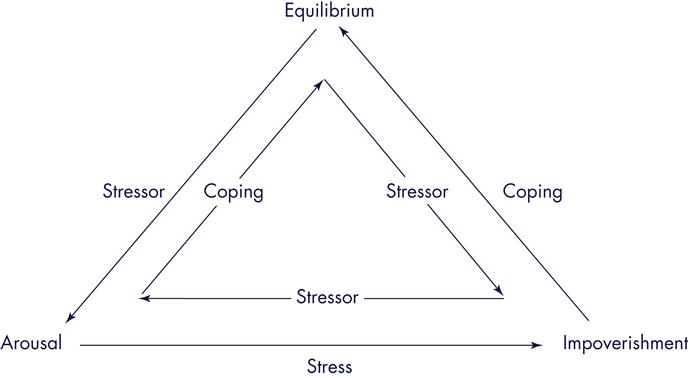
H. Erickson’s first independent research study occurred during graduate school. Under Swain’s supervision, a study was designed to test the Adaptive Potential Assessment Model (APAM) (Erickson, 1976), which had been conceived, labeled, and articulated in the mid-1970s (Figure 16-1). Concurrently, Swain and Erickson collaborated on another project designed to test the effects of MRM nursing interventions with persons who had hypertension. This work led to a third study that explored the effects of using MRM with persons who had diabetes (Erickson & Swain, 1982). Tomlin joined the research team for this project.
During these years Erickson also expanded and tested the concept of self-care knowledge (Erickson, 1984, 1990) that was conceived during the 1960s and early 1970s. She presented numerous papers, consulted in various agencies, taught at the University of Michigan, and continued her independent practice. Tomlin continued to explore ways to apply MRM in practice and to teach the theory and paradigm to undergraduate students while Swain supervised Erickson’s research, collaborated with her on further elaboration of the theory, and facilitated the administrative phase of Erickson’s career.
Finally, innumerable requests for written materials from practicing nurses, students, and faculty mandated that the book Modeling and Role-Modeling: A Theory and Paradigm for Nursing be written. After the book was published, it was used as a text at the University of Michigan. Undergraduates were taught the basic premises; several university hospital units adopted it as a guide for practice (Walsh, Vandenbosch, & Boehm, 1989); a modified assessment form was developed at the University of Michigan Medical Center (Campbell, Finch, Allport, et al., 1985); graduate students used it to guide their master’s theses (Calvin, 1991; Finch, 1987; Hannon & McLaughlin, 1983; Smith, 1980; Walker, 1990); and doctoral students used it for their dissertations (Acton, 1993; Baas, 1992; Baldwin, 1996; Barnfather, 1987; Beltz, 1999; Benson, 2003; Boodley, 1986; Bowman, 1998; Bray, 2005; Chen, 1996; Clayton, 2001; Curl, 1992; Daniels, 1994; Darling-Fisher, 1987; Dildy, 1992; Erickson, 1996; Hertz, 1991; Holl, 1992; Hopkins, 1994; Irvin, 1993; Jensen, 1995; Keck, 1989; Kennedy, 1991; Kline, 1988; Landis, 1991; MacLean, 1987; Miller, 1994; Miller, 1986; Nash, 2004; Raudonis, 1991; Robinson, 1992; Rogers, 2003; Rosenow, 1991; Scheela, 1991; Sofhauser, 1996; Straub, 1993; Weber, 1995). These studies helped identify and support many of the theoretical concepts and proposed midrange theories.
The Society for the Advancement of Modeling and Role-Modeling
In 1986, a website (www.mrmnursingtheory.org) was established by a cohort of students, faculty, and practitioners, and national biennial conferences were initiated. The first conference was co-sponsored by the University of Michigan in Ann Arbor in 1986, followed by the University of South Carolina at Hilton Head in 1988, and the University of Texas at Austin in 1990. National conferences continue to be held biennially. The Society for the Advancement of Modeling and Role-Modeling was established in 1986.
Schools and health care organizations—including, but not limited to Metro State University in St. Paul, Minnesota; State University of New York at Buffalo; University of Tennessee at Knoxville; Capital University, Columbus, Ohio; St. Catherine’s Hospital in Minneapolis, Minnesota; Lamar University, Joanne Gay Dishman Department of Nursing, Beaumont, Texas; the University of Texas at Austin, Galveston, and Brownsville; and others—have adopted and use MRM as the bases for either parts or all of their nursing curricula. In addition, health care agencies throughout the country such as the University Health System in Knoxville, Tennessee, or Salina Regional Health Center, Salina, Kansas, have applied MRM to implement and guide holistic nursing practice (Alligood, 2011; Perese, 2002).
Continued research has provided support for several of the middle-range theories proposed in MRM. The three states of the APAM model have been tested and found to be independent of one another and predictors for stress (Barnfather, 1990; Barnfather, Swain, & Erickson, 1989a,b; Erickson & Swain, 1982, 1990). Relationships have been shown between the following: stress and needs status (Barnfather, 1990, 1993); needs status and developmental residual and hope (as developmental residual) (Curl, 1992); burden and affiliated-individuation in caretakers of persons with Alzheimer’s disease (Acton, 1993); needs satisfaction (Leidy, 1994); needs and affiliated-individuation (Acton & Miller, 1996); stressand affiliated-individuation (Irvin & Acton, 1996); perceived support, control, and well-being in the elderly (Chen, 1996); and stress, psychological resources, and physical well-being (Leidy, 1989, 1990).
Several studies also have been conducted to explore perceived enactment of autonomy (PEA) in the elderly (Hertz & Baas, 2006), PEA and self-care, and holistic health in the elderly (Anschutz, 2000; Anschutz & Hertz, 2002); PEA and related socioeconomic factors among noninstitutionalized elders (Hwang & Lin, 2004); and PEA, self-care resources, among seniors (Matsui & Capezuti, 2008).
Other studies have provided support for linkages between role-modeled interventions and outcomes (Acton, 1993; Acton, Irvin, Jensen, et al., 1997; Erickson, 1996, 2006; Erickson, Thomlin, & Swain, 1983; Hertz, 1991; Holl, 1992; Hopkins, 1994; Irvin, 1993; Jensen, 1995; Keck, 1989; Kennedy, 1991; Kline, 1988; Scheela, 1991).
Instruments have been developed to enhance application of MRM in practice and research. Tools include those designed to measure the following: needs status (Leidy, 1994); developmental residual (Darling-Fisher & Leidy, 1988); the APAM stress states using content analysis (Hopkins, 1994); self-care resources of cardiac patients (Baas, 1992, 2011); denial in postcoronary patients (Robinson, 1992); perceived enactment of autonomy in the elderly (Hertz, 1991); family experience with eating disorders (Folse, 2007); patients’ adjustment to implanted cardiac devices (Beery, Baas, Mathews, et al., 2005); and the bonding-attachment process within the context of needs satisfaction in teenage mothers (Erickson, 1996).
This theory also can be applied in all settings and with all populations. MRM has been used to provide a theoretical foundation for exploration and examination of how persons ages 85 and older manage their health (Beltz, 1999), quality care of diverse older adults (Hertz, 2008); urinary incontinence and assessment of the Bladder Health Program among rural elders (Liang, 2008, 2011); to achieve greater understanding of families’ experience through prolonged periods of suffering and their evolution toward spiritual identity (Clayton, 2001); caring for people living with advanced cancer (Haylock, 2010); finding meaning in life (Clayton, Erickson, & Rogers, 2006; Erickson, 2006); living with mental health disorders (Hagglund, 2009; Sung & Yu, 2006); mentoring students (Lamb, 2005); and coping with stress (Benson, 2006). Benson’s application of MRM was supportive and provided insight into the subsequent use of APAM in small groups (Benson, 2003, 2011). MRM also has provided a foundation for exploration of how patients adjust to implanted cardiac devices (Beery, Baas, & Henthorn, 2007).
Researchers have used this holistic nursing theory and paradigm to explore the following situations: lived experiences and perceptions of hope of elementary children in urban areas (Baldwin, 1996); the experience and perceptions of mothers using child health services in South Africa (Jonker, 2012); the meaning of encouragement and its connection to the inner-spirit perceived by caregivers of the cognitively impaired (Miller, 1994); the evaluation of holistic peer education and support group programs aimed at facilitating self-care resources in adolescents (Nash, 2004, 2007); the experiential meaning of well-being for employed mothers (Weber, 1995); the relationship between psychosocial attributes, self-care resources, basic needs satisfaction, and measures of cognitive and psychological health ofadolescents (Bray, 2005); psychosocial aspects of heart failure management (Baas & Conway, 2004); and self-care resources and activity as predictors of quality of life in person’s with post-myocardial infarction (Baas, 2004). In addition, holistic healing for women with breast cancer through a mind, body, and spirit self-empowerment program (Kinney, Rodgers, Nash, et al., 2003); morbid obesity (Lombardo & Roof, 2005); patient’s perceptions regarding nurse-client interactions (Rogers, 2003), the relationship between basic need satisfaction and emotional eating (Cleary & Crafti, 2007; Timmerman & Acton, 2001) has been studied using MRM.
Finally, research has been conducted to further explore major constructs or philosophical assumptions in the MRM theory. Baas, Beery, Allen, and colleagues (2004) studied self-care knowledge in patients with heart failure and transplant; Baldwin (2004) studied self-care for clients in early menopause; Baldwin and Herr (2004) studied the effect of self-care on treatment of interstitial cystitis; Baldwin, Hibbeln, Herr, and colleagues explored self-care as defined by members of an Amish community (2002); and Beery, Baas, Fowler, & Allen (2002) studied spirituality in persons with heart failure.
Overview of Modeling and Role-Modeling
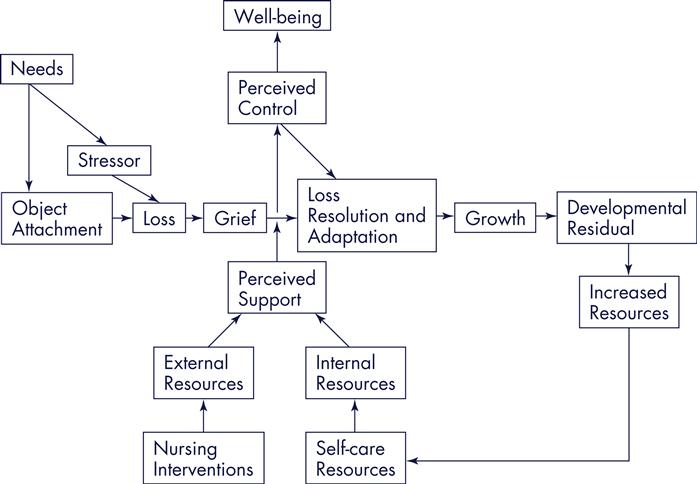
Modeling and Role-Modeling (Erickson, et al., 1983 [reprinted in 2002]), conceived within the context of numerous philosophical assumptions, was labeled and articulated by Erickson synthesizing several concepts from established theories. Concepts were drawn from the works of Maslow (1968, 1970), Bowlby (1969, 1973, 1980), Erikson (1963), Engel (1962, 1968), and Selye (1974) to create a new theory that described relations among needs, loss, grief, adaptation, developmental processes, growth, and well-being of the holistic person (Figure 16-2). The practice paradigm was derived from integrating philosophical assumptions with theoretical underpinnings.
Philosophical Assumptions and Constructs
Holism
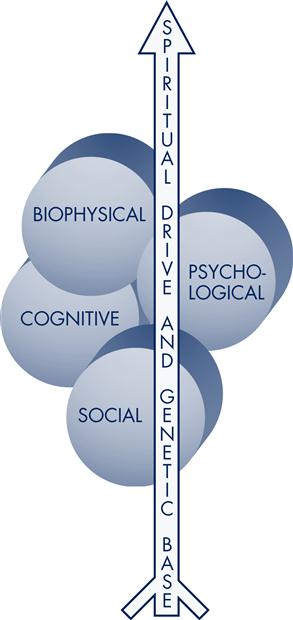
Humans consist of cognitive, biophysical, social, and psychological subsystems permeated by genetic predispositions and a spiritual drive (Figure 16-3). The ongoing interaction of these multiple components creates a dynamic, holistic system that is greater than a sum of the parts (Erickson, Tomlin, & Swain, 2005). Health, which is affected by these dynamic interactions, is a perception of well-being, as perceived by the client. Although physical status influences perceptions of health, persons can perceive a high level of well-being even as they take their last breath. Therefore, health can be defined as a dynamic, eudaemonistic sense of well-being (Erickson, et al., 2005) associated with self-fulfillment and transcendence beyond the objective reality of the moment (Erickson, 2001).
Affiliated-Individuation
Essential to a person’s sense of well-being is the need for affiliated-individuation (AI). AI, coined by Erickson, is defined as “the need to be dependent on support systems while simultaneously maintaining independence from these support systems (Erickson, et al., 1983, p. 252). AI is usually first recognized, and acceptedas normal, during the stage of autonomy as a toddler explores the world but reconnects regularly with his or her care provider. Although AI is a lifelong need for all people, it is commonly not recognized as acceptable behavior as people get older and are expected to be independent.
Need Satisfaction, Growth, and Development
Humans are in a continual state of change and have inherent drives that motivate behavior. These include a drive for needs satisfaction, adaptation, and growth sequential development. According to Erickson and colleagues (2005), “Growth is defined as the changes in body, mind, and spirit that occur over time” (p. 46) and facilitates an individual’s development. Development is defined as “the holistic synthesis of the growth-produced…differentiations in a person’s body, ideas, social relations, and so forth” (Erickson, et al., 1983, p. 47). When individuals are given necessary information, adequate emotional support, and are empowered in making satisfactory decisions, growth and subsequent development occur and health is enhanced.
Internal and External Resources
According to the MRM paradigm, the nurse facilitates an interactive, interpersonal relationship with the client. During this process the nurse assists the client inidentifying, developing, and mobilizing internal and external resources—resources needed to cope with life’s stressors, to grow and heal. Essential to this process is the nurse’s unconditional acceptance of the client. Erickson and colleagues (1983) argue that “[b]eing accepted as a unique, worthwhile, important individual—with no strings attached—is imperative if the individual is to be facilitated in developing his or her own potential” (p. 49).
Modeling
In a supportive and caring environment, a nurse attempts to understand “the client’s personal model of his or her world and to appreciate its value and significance for the client from the client’s perspective” (Erickson, et al., 1983, p. 49). The act of developing an image and understanding of the clients’ worldviews from within their perspectives and framework is called modeling. “The way an individual communicates, thinks, feels, acts, and reacts—all of these factors comprise the individual’s model of his or her world” (Erickson, et al., 1983, p. 84).
Role-Modeling
After the client’s world has been modeled, the nurse facilitates and nurtures the individual “in attaining, maintaining, or promoting health through purposeful interventions” (Erickson, et al., 1983, p. 254). This is known as role-modeling. In role-modeling the client’s world, the nurse plans interventions that do the following:
These interventions are aimed at helping the client “achieve an optimal state of perceived health and contentment” (Erickson, et al., 1983, p. 49).
Self-Care Knowledge, Self-Care Resources, Self-Care Actions
Nursing interventions are designed based on the belief that all individuals at some level understand what has interfered with their growth and development and altered their health status. Accordingly, people also know what they need to improve and optimize their state of health, facilitate their growth and development, and maximize their quality of life and well-being. This inherent knowledge is called self-care knowledge. Individuals also have internal and external self-care resources. Internal self-care resources (or self-strengths) refer to all of the “internal resources that an individual can use to promote health and growth” (Erickson, et al., 1983, p. 128). These strengths are defined by the perceptions of both the nurse and the client and can include attitudes, endurance, patterns, or whatever else is perceived to be a personal strength and resource of that individual. External self-care resources include the client’s social network and support systems. The social network is a set of individuals with whom the client is socially acquainted, and support systems are a set of individuals who are perceived to support, energize, and provide resources for the client.
Development and utilization of self-care knowledge and self-care resources is known as self-care action. “Through self-care action the individual mobilizes internal resources and acquires additional resources that will help the individual gain, maintain, and promote an optimal level of holistic health” (Erickson, et al., 1983, p. 49).
Finally, an individual’s potential for mobilizing resources and achieving a state of coping is directly related to his or her level of needs satisfaction (Erickson, et al., 1983). Individuals who have a high level of needs satisfaction have a greater ability to positively cope with life’s stressors and to achieve a state of equilibrium. However, individuals who have a high level of unmet needs have less ability to mobilize resources and are at risk when confronted with stressors.
Nursing interventions are designed to facilitate clients in using self-care actions that will help them meet their physiological, psychological, social, cognitive, and spiritual needs. Repeated needs satisfaction results in growth; continued growth produces healthy developmental residual. Fundamental to this theory is the understanding that an individual’s needs are met only when the individual perceives that they are met.
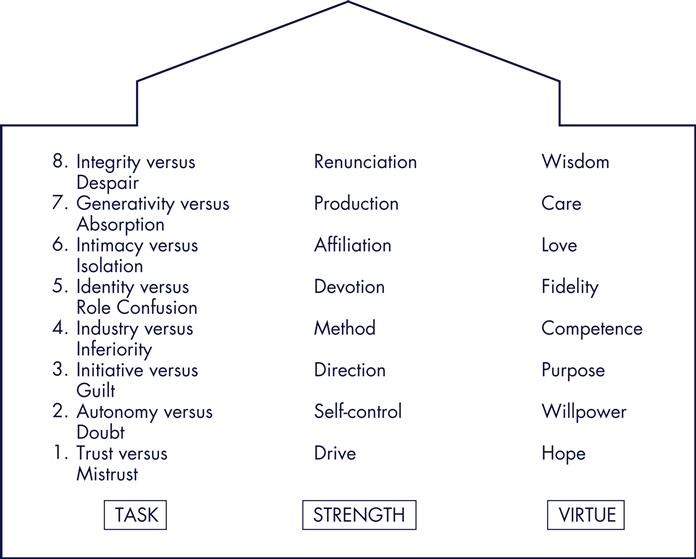
Theoretical Underpinnings
Developmental processes are sequential tasks, strengths, and virtues that are associated with biological time periods (Figure 16-4). Each stage has a central focusand related life task to be accomplished. The manner in which this task is completed will determine what type of developmental residual results. Residual from stage one serves as a resource (or hindrance) for task resolution of stage two, and so forth across the life span. Because of the epigenetic nature of the developmental processes, people are constantly reworking earlier stages. One’s ability to resolve developmental tasks in a healthy manner (and to rework earlier acquired residual) is dependent on resources accrued from having one’s needs met across the life span.
Need Satisfaction, Growth, and Development
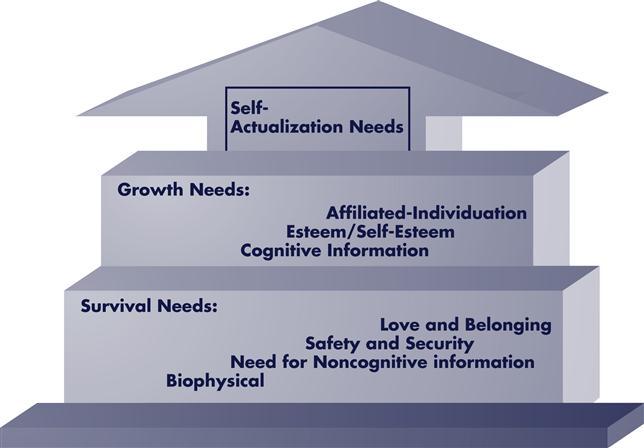
Inherent needs, classified as survival, AI, or growth-related, emerge in a quasi-ordered manner. Lower-level needs must be satisfied to some degree before higher-level needs emerge (Figure 16-5). Minimal lower-level and mid-level needs satisfaction is necessary for survival; repeated needs satisfaction facilitates growth and development. Lower-level and mid-level needs deficits create tension and drive behaviors aimed at meeting those unmet needs; satisfaction of these needs dissipates the tension. Higher-level needs satisfaction creates tension and desirefor additional growth experiences. People who repeatedly experience unmet needs during the early years of life develop a deficit motivation toward relationships. Those who repeatedly experience needs satisfaction during the early years of life develop a being motivation.
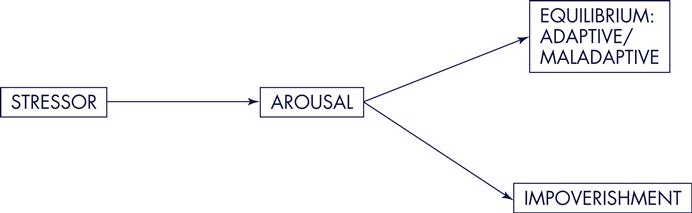
Unmet Needs as Stressors and Stress Responses
Unmet needs are stressors; stressors produce stress responses. Resolution of stress requires adequate resources; one’s ability to mobilize adequate resources determines the outcome of the stress response. Stressors, stress responses, and resources may be within the same subsystem; however, they are not limited to a single subsystem. For example, an individual may experience an accident that can affect his or her physiological subsystem, or depending on the severity and the client’s perception of the event, it may affect the client’s physiological, emotional, cognitive, and spiritual subsystems.
Stress Response States: Arousal and Impoverishment
The two types of stress response states are arousal and impoverishment. When adequate resources are available and readily mobilized, arousal occurs (Figure 16-6). When inadequate (or diminished) resources are available, impoverishment occurs. Those in impoverishment are at greatest risk for continued stress, depletion of resources, and resulting illness, disease, and/or physical death than are those in arousal (see Figure 16-6).
Adaptation, Attachment Objects, Loss and Grief Response
Adaptation occurs as needs are met, stress responses are diminished, and new resources are built. Those objects that repeatedly meet needs become attachment objects. These objects change as people move through various developmental stages. When attachment occurs, loss of attachment objects will result in feelings of loss. Loss can be situational and developmental. Loss is real, threatened, or perceived. Examples of situational losses are the loss of a favored item, the perceived rejection by a loved one, or a major flooding of one’s home. Developmental losses are phases of movement through the developmental sequence, such as weaning during infancy, going to school, or leaving home. When loss occurs—whether it is real, threatened, or perceived—people experience grief.
The grief process has sequential phases; movement through the grief process requires mobilization of resources. One’s ability to mobilize adequate resources determines the outcome of the grief response. Inadequate resources and one’s inability to deal with a loss result in morbid grief (Lindemann, 1942); morbid grief affects future developmental processes, as Box 16-1 illustrates. A synthesis of these multiple theories provided the bases for the MRM theory. Major theoretical linkages are shown in Box 16-1.
Critical Thinking in Nursing Practice with the Modeling and Role-Modeling Theory
The MRM practice paradigm is guided by five related nursing principles, intervention aims, and outcome goals for the nursing process (Table 16-1). There are interview guidelines that influence the type of data collected and specify the purpose of the data (Table 16-2). Table 16-3 illustrates the process for each phase of assessment. It discusses the data interpretation and analysis that lead to nursing impressions.
TABLE 16-1
Nursing Principles, Aims, and Goals
| Intervention Goal | Principle | Aim |
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|